Authors / metadata
DOI 10.36205/trocar3.2021001
Abstract
Objective: Correlation between hysteroscopic appearance of cystic atrophy with serum estradiol levels of < 37 pg/ml (biological reference, age /gender specific) and histopathological results of endometrial tissue biopsy.
Type of Study: Prospective observational cohort ongoing study. Ethics committee approved this study.
Participants: Postmenopausal women undergoing hysteroscopy.
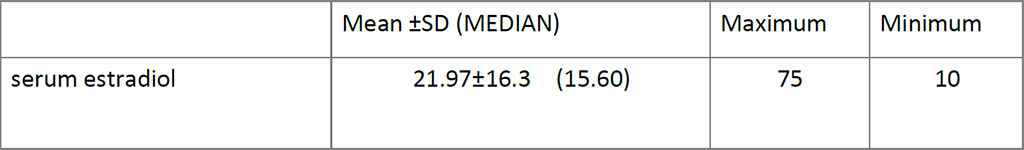
Intervention: Hysteroscopy was performed without anesthesia using a 5 mm continuous flow Bettocchi Office Hysteroscope, Karl Storz with 5Fr mechanical instruments i.e., grasping forceps or Hysteroscopic Tissue Removal System 5C with incisor insert. Endometrial biopsy is obtained by targeted or visual dilatation & curettage (D&C) and tissue sent for Histo Pathological Examination (HPE). Venous blood is collected for serum estradiol levels (S. El), analyzed using chemiluminescence immunoassay method and levels of < 37 pg/ml (biological reference, age /gender specific) were considered low risk. Of 35 women, 1 was lost for follow up and 2 did not have S.El.
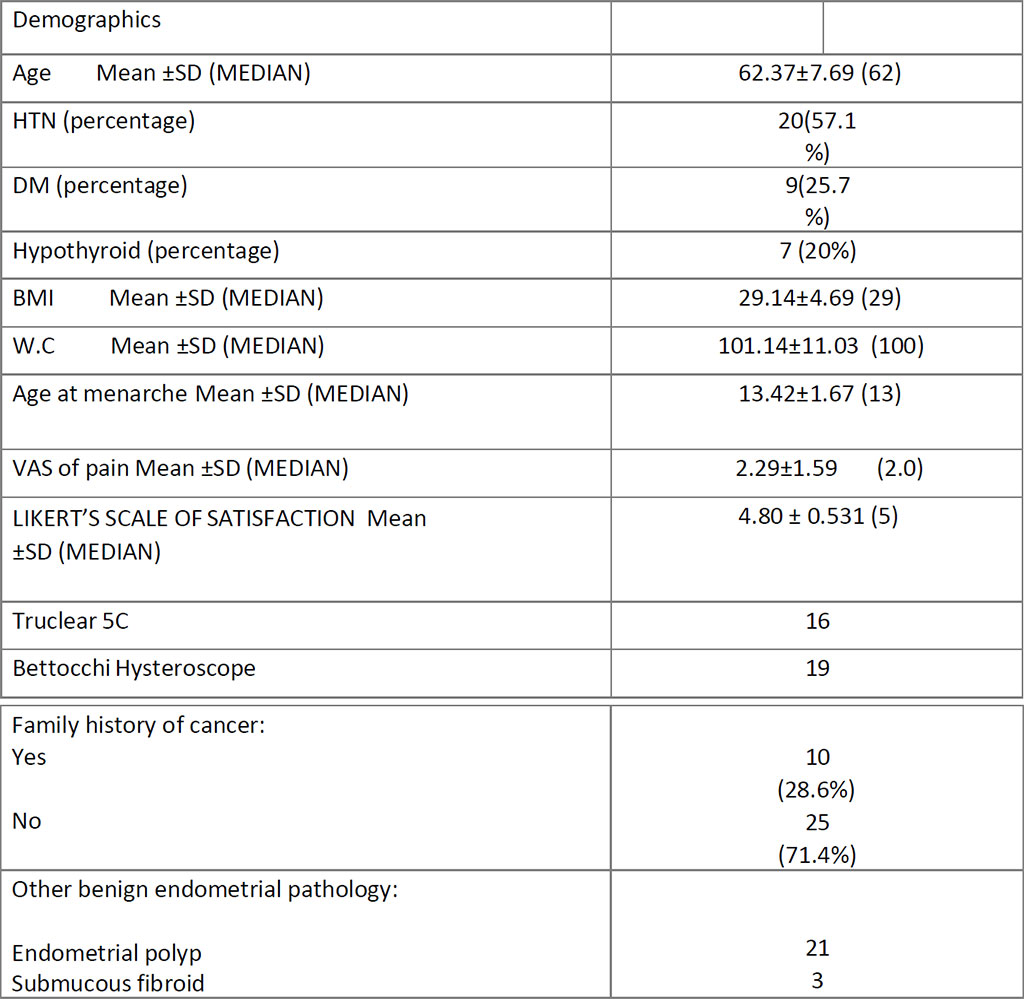
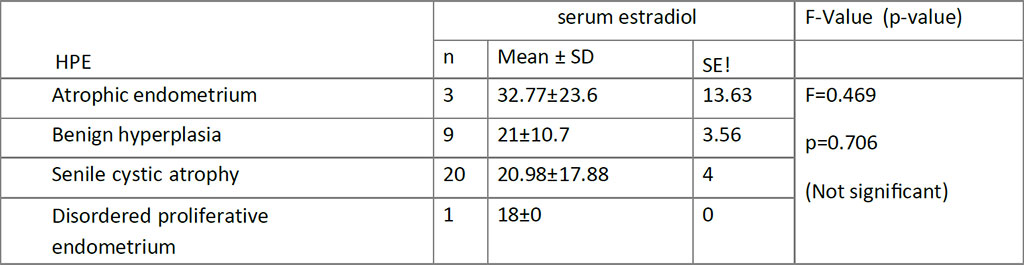
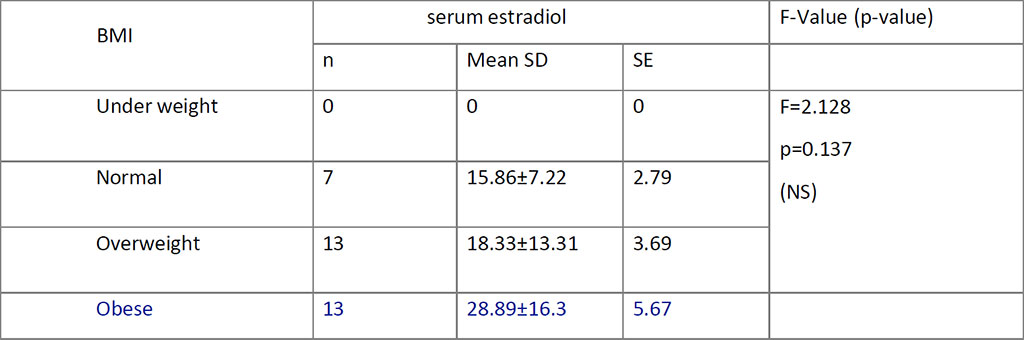
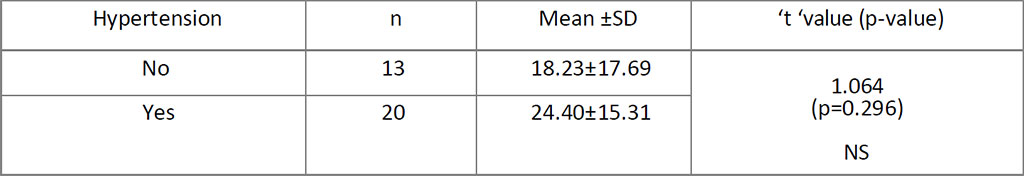
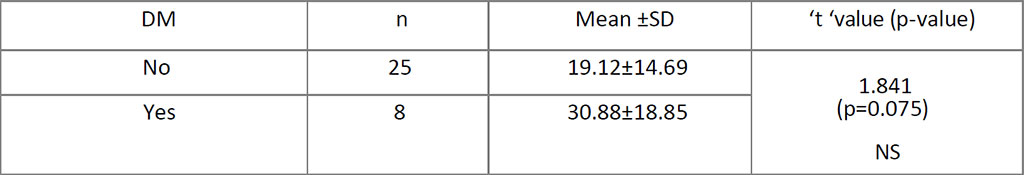
Main findings & Results: Mean age was 62.4 ±7.7years. 57% of the patients were biopsied by targeted technique and 43 % by visual D&C. Twenty women had Senile Cystic Atrophy (SCA) on HPE with a mean S. El of 20.98±17.88; p=0.706. The prevalence of cystic atrophy by HPE confirmation is 20.6 %. The other HPE diagnosis were atrophic (3), benign hyperplasia (9) and disordered proliferative endometrium (1). Obese (n=13; mean S. El = 28.89±16.3; p=0.137), hypertensive (N=20 S. El = 24.40±15.31; p=0.296) and diabetic (n=8 ; S.El = 30.88±18.85;p=0.075) women with HPE confirmed SCA seem to have higher S.El.
Follow up of 12 months – 5 women underwent hysterectomy; 1 had a repeat endometrial biopsy with HPE as SCA and other remain asymptomatic.
Conclusion: Hysteroscopic view of cystic atrophy correlates 60 % with histopathology in the preliminary analysis. Cystic atrophy does not increase the risk of endometrial carcinoma.
Introduction
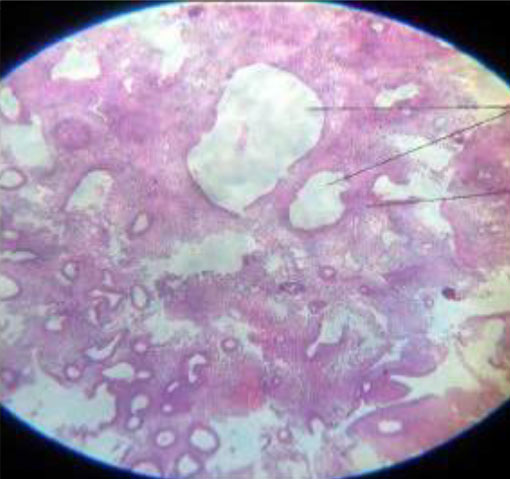
Endometrial senile cystic atrophy (SCA) is a variant of atrophic type of endometrium which is inactive and features cystic dilatation of the glands surrounded by flattened tubular cells with fibrosis. There is no proliferative or secretary active in SCA (1).
SCA is a benign and less frequently reported in literature, especially as a hysteroscopic finding. This type is seen more frequently in breast cancer patients on tamoxifen. Transvaginal ultrasound shows a thickened endometrium, urging an endometrial biopsy (2,3).
Different theories are proposed for the development of SCA -irregular proliferation or cystic glandular hyperplasia at perimenopause, prior to the decline in estrogen levels. (4).
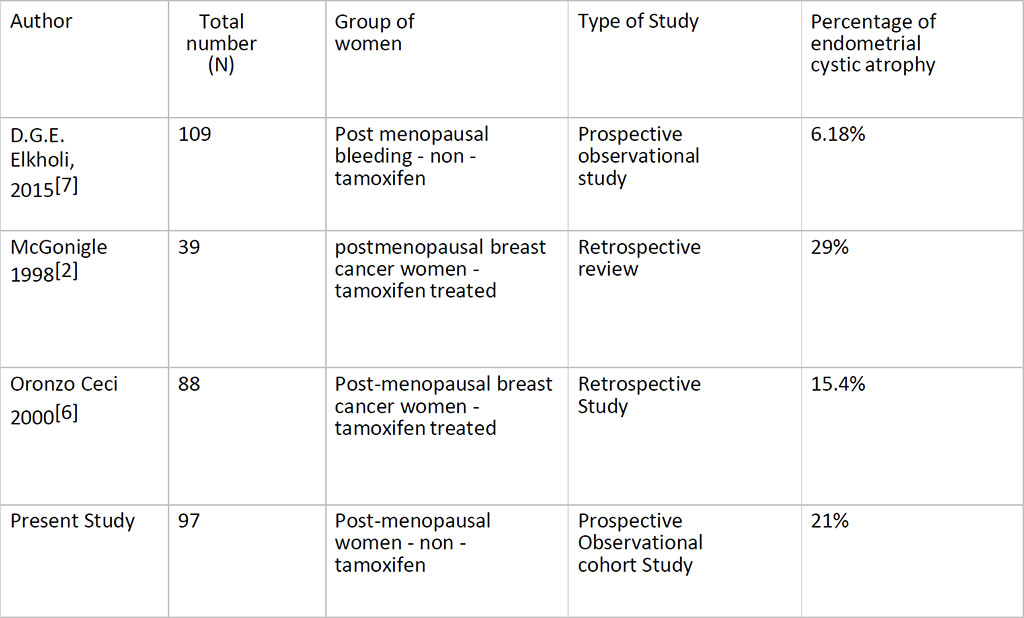
The other causes many be due to the presence of atrophic variants of cyclically dilated glands seen in the basal functional layer of the endometrium in women aged 35 years and over, or the stromal fibrosis may block the glands and causing distension (5). Most studies are done in postmenopausal women on tamoxifen treated breast cancer patients. Hysteroscopic evaluation showed an incidence of 15. 4 % with glandular cystic atrophy in 88 postmenopausal women (6), and a prevalence of 29% in 38 patients (2).
D.G.E. Elkholi et al in their prospectiveobservational study, performed serumconcentration of total testosterone (T),androstenedione (A), estrogen (E1) andestradiol (E2) and sex- hormone bindingglobulin (SHBG) in 50 postmenopausalpatients with bleeding. Cystic atrophicwas detected in 6 cases (6.18%). Theyfound that serum concentration of sexsteroid hormones T, A, E1, and E2 wassignificantly higher and SHBG was significantly lower in cases of atrophic/weakly proliferative and mixed endometrium than in cases of atrophic inactive and cystic atrophic endometrium (7). This may explain the development of endometrial adenocarcinoma in an atrophic endometrium.
Materials and Methods
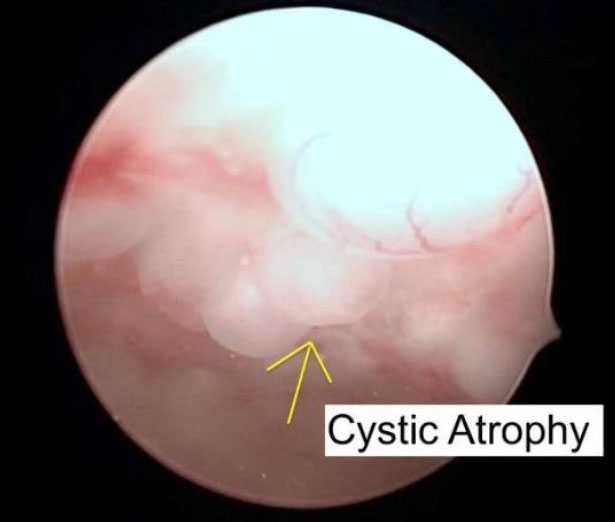
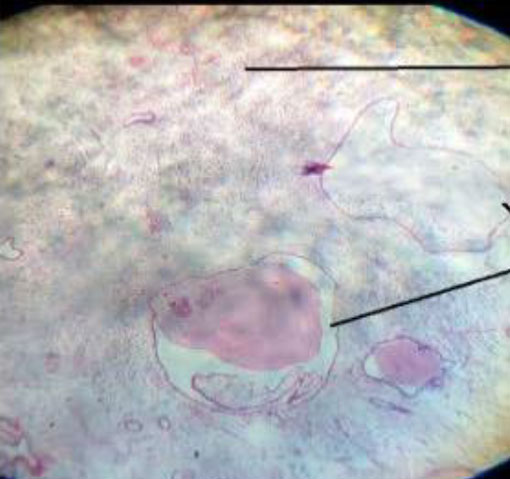
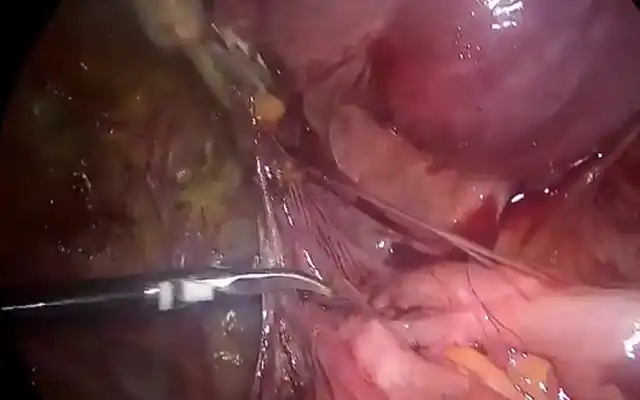
This is a prospective observational cohort ongoing study. The Ethics Committee approved the study. 97 postmenopausal women underwent Office Hysteroscopy (OH). 35 of them had a hysteroscopic appearance of cystic atrophy (Figure.1). Transvaginal ultrasound was done with Voluson GE-S 10 expert. Hysteroscopy is performed without anesthesia using a 5 mm continuous flow Bettocchi Office Hysteroscope, Karl Storz with 5Fr mechanical instruments i.e., grasping forceps or Hysteroscopic Tissue Removal System 5C with incisor insert. Endometrial biopsy is obtained by targeted or visual dilatation & curettage (D&C) and tissue is sent for HPE. Normal saline is used as distention media and pressures is controlled by the Hamou hysteromat. The outpatient hysteroscopy endometrial biopsy sample is sent for histopathological assessment. Venous blood is collected for serum estradiol levels (S. El), analyzed using chemiluminescence immunoassay method and levels of < 37 pg/ml (biological reference, age /gender specific) are considered low risk. Of 35 women, 1 was lost for follow up and 2 did not have S.El. We choose to perform only Serum estradiol levels, as following menopause, there is decreased level of circulating estradiol (8).
The study period was set for 2 years including data collection with a follow up of one year from January 2020 up to 31st December 2022. The report considers the preliminary report of the study January 2020 – August 2021.
Inclusion Criteria: 1. Postmenopausal women 2. Hysteroscopic appearance of cystic atrophywith the presence of protuberance in the endometrium, due to cystic dilatation of the endometrial glands.
Exclusion Criteria: 1. Women on Tamoxifen 2. Women on oral hormone replacement therapy. The sample size number is 89 based on the Number Needed to Diagnose (NND) of prospective studies in the literature with an absolute precision of 5 %. Statistical Analysis: In Descriptive statistics, the continuous variable are expressed as mean and standard deviation and categorical variables are expressed in frequency and percentage. In Inferential statistics, Independent Students ‘t’- test is used to test the comparison between group of continuous variables outcome. Chi- square test/ Fisher’s exact test is used to compare the categorical data between the variables. Karl–Pearson/Spearman rank and kappa test is used for correlation between variables outcomes. Statistical analyses are performed by using SPSS version 23.0. All statistical analyses are tested at 95% confidence interval and the P value of <0.05 is considered as statistically significant.
Primary outcome measure: Correlation between hysteroscopic appearance of cystic atrophy with serum estradiol levels of < 37 pg/ml (biological reference, age /gender specific) and histopathological results of endometrial tissue biopsy.
Secondary outcome measure: 1. To know the prevalence of cystic atrophy. 2. To understand the clinical significance of performing a serum estradiol level in women with cystic atrophy, i.e., is there a risk of endometrial cancer in women having cystic atrophy in non- tamoxifen users.
Results
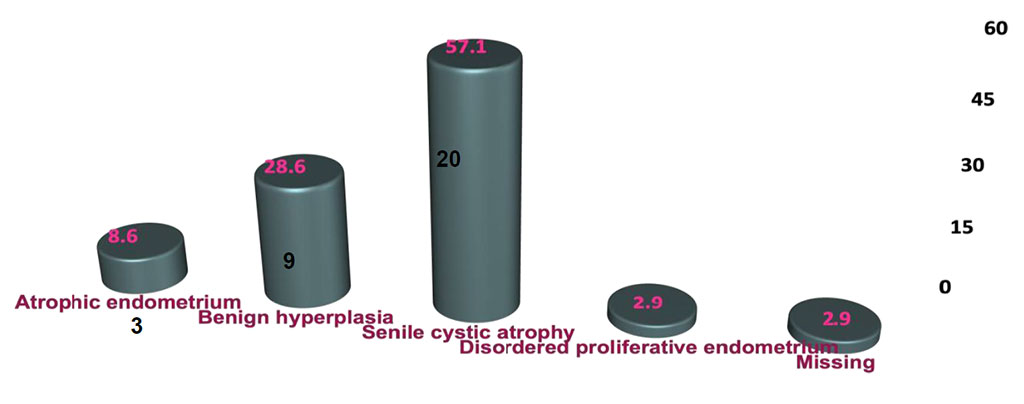
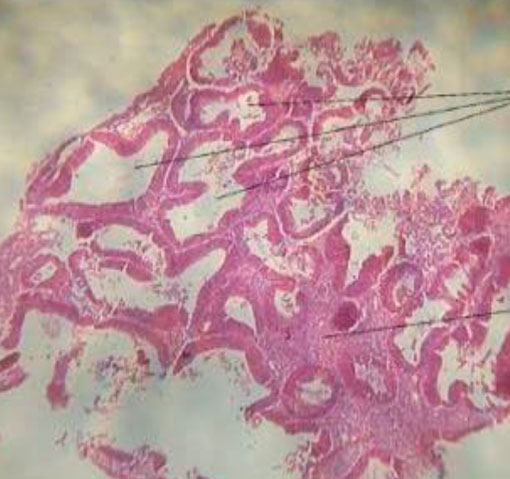
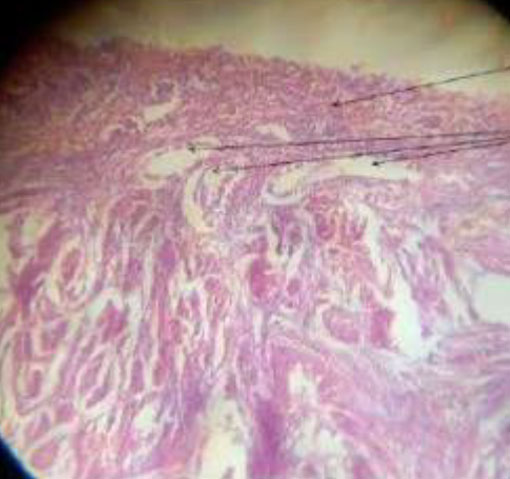
Mean age was 62.4 ±7.7years (Table. 1). 57% were biopsied by targeted technique and 43 % by visual D&C. 20 women had SCA on HPE with a mean S. El of 20.98±17.88; p=0.706. The prevalence of cystic atrophy by HPE confirmation is 20.6 %. The other HPE diagnosis were: atrophic (3), benign hyperplasia (9) and disordered proliferative endometrium (1) (Figure.2,3).
Obese (n=13; mean S. El = 28.89 ± 16.3; p=0.137), hypertensive (N=20 ;S.El = 24.40±15.31; p=0.296) and diabetic (n=8 ; S.El = 30.88±18.85;p=0.075)
women with HPE confirmed SCA seem to have higher S. El (Table.4,5,6).
Follow up of 12 months – 5 women underwent hysterectomy; 1 had a repeat endometrial biopsy with HPE as SCA and other remain asymptomatic.
Discussion
The preliminary results of this study show an accuracy of 60 % hysteroscopic correlation with HPE. This may be due to the poorly defined hysteroscopic view of cystic atrophy and failure to obtain adequate tissue in cases of targeted biopsy and flattened endometrium. Table 7. Compares the prevalence of cystic atrophy in different studies.
It is now known that unopposed excessive estrogen stimulation at menopause may lead to endometrial adenocarcinoma in the background of atrophic endometrium (9).
High estradiol levels as seen in obesity, hypertension and diabetes may pose a risk of developing endometrium cancer in these women even in the background of cystic atrophy, and require a long term follow up with transvaginal ultrasound and doppler studies with control of the metabolic diseases.
Implications for research: Comparing visual dilatation and curettage versus targeted biopsy in post-menopausal patients requiring endometrial biopsy and correlation with histopathological reports.
Conclusion
The hysteroscopic view of cystic atrophy correlates 60 % with histopathology in the preliminary analysis. Cystic atrophy does not increase the risk of endometrial carcinoma, but presence of metabolic diseases may pose a risk of endometrial cancer due to the increased estradiol levels.
Hysteroscopic view: cystic atrophy. Immunohistochemistry may add value if the density of estrogen and progesterone receptors in the epithelial cells is high, in women with metabolic diseases and under evaluation for postmenopausal bleeding (9).
Limitations: The amount of endometrial tissue available for HPE varies in the two techniques of targeted biopsy and visual dilatation and curettage. Targeted biopsy with resection of the area or visual dilatation and curettage may increase the accuracy of the hysteroscopic view.
Strength: This is a prospective cohort ongoing study with a follow up of 12 months and aim to follow for 10 years.
Learning points: Evaluation for postmenopausal women must include a transvaginal ultrasound, hysteroscopy, as the technique involves direct vision, and an endometrial biopsy. Performing serum concentration of E2 may help in the management plan.
Sources / references
Figure 1. Cystic atrophy
Table 1. Demographics of Postmenopausal Women
Table 2. Serum Estradiol levels(pg/ml)
Table 3. Correlation of Histopathology findings with S. Estradiol levels (One way ANOVA)
Figure 2. Histopathological findings of the endometrium
Figure 3. Histopathological differentiation of the endometrium findings
Table 4. Comparison between BMI and S. Estradiol
Table 5. Comparison between Hypertension and S. Estradiol
Table 6. Comparison between DM and S. Estradiol
Table 7. Incidence / Prevalence in various studies