Authors / metadata
DOI: 10.36205/ trocar3.2022004
Abstract
Congenital malformations of the female genital tract are being diagnosed more frequently due to advances in imaging techniques. A broad international consensus on their classification is still lacking. This paper aimed to comparatively summarize the most frequently and widely used, as well as the most recently developed classification systems of congenital female genital malformations. A non-systematic review was done through a search on major databases with the medical subject heading (MeSH) term ‘‘congenital abnormalities” in combination with ‘‘classification” and ‘‘female genitalia”. All available systems, including, among others, the American Fertility Society Classification (1988), the Acien and Acien classification (1992, 2004), the VCUAM system (2005), the European Society for Human Reproduction and Embryology – European Society for Gynecological Endoscopy classification (2013), the Congenital Uterine Malformation Experts (CUME) group recommendations, and the American Society for Reproductive Medicine Classification (2021) possess the advantages and disadvantages listed in this article. Regarding the most common situations, the criteria for differentiating physiologic arcuate and discrete partial septate uteri vary widely between classifications, while difficulties also persist with the rarer complex abnormalities that cannot be easily classified, contributing to a gap in clinical and research protocols. The main factor compromising any attempt to reach an ideal classification system is the lack of evidence-based data, justifying the need for comparative multicenter international randomized control trials in this field. Pending new research data and a broad international consensus, it seems essential for adequate patient orientation to describe each detected malformation in detail and to correlate it with the clinical presentation, regardless the type of classification used.
Introduction
Congenital malformations of the female genital tract consist on a heterogeneous group of deviations from normal anatomy (1, 2), which may result from the maldevelopment of the Mullerian or paramesonephric ducts during fetal life (3). Although considered rare in the past, with technological advancements and increasingly available diagnostic tools, these anomalies seem to be present in about 7% of the general population, with an even higher prevalence in the infertile population (4). Congenital malformations of the female genital tract often receive inappropriate, insufficient and/or late clinical attention, resulting in persistent symptomatology such as chronic pelvic pain or impaired reproductive function (5, 6).
Since the 1800s, there have been attempts to classify the female congenital anomalies; however, the first classifications were lacking organization and clarity (7). In 1979, Buttram and Gibbons developed a classification system based on their analysis of 144 cases, dividing the anomalies in five different groups in accordance with the degree of failure of normal uterine anatomical development, clinical presentation and related pregnancy outcomes (8). In 1988, the American Fertility Society (AFS) published the first widely used classification system. Since then, many other classifications have been proposed, some of them quite broadly, but no one universally accepted.
The ideal classification system should be: (a) clear and precise in respect with the definitions and terms used; (b) accurate for diagnosis and differential diagnosis; (c) schematic and visually user-friendly to help classify the malformation in daily clinical practice; (d) comprehensive, incorporating all possible anatomical variations; (e) well correlated with the clinical presentation, treatment and prognosis of the patients; (f) based on scientific evidence and validated and (g) as simple as possible (2). Such a system does not exist. Each classification for congenital malformations of the female genital tract presents some advantages and disadvantages in comparison with other available classification systems.
This paper aims to comparatively summarize the most frequently and widely used, as well as the most recently developed classifications of congenital female genital malformations.
Material Method
A non-systematic review was done through a search on the following databases: MEDLINE, Global Health, EMBASE, The Cochrane Library, Web of Science and Health Technology Assessment Database. The medical subject heading (MeSH) term ‘‘congenital abnormalities” (MeSH Unique ID: D000013) in combination with ‘‘classification” (MeSH Unique ID D002965) and ‘‘female genitalia” (MeSH Unique ID D005836) was used. The papers written in English language were selected from inception of the above-mentioned databases until August 1st, 2022. Titles and/or abstracts of studies retrieved using the search strategy were screened independently by two authors (P.P.A. and D.D.) to identify studies that couldpotentially meet the aims of this project. Potentially eligible articles (full texts) were retrieved and independently assessed for eligibility by the authors (P.P.A. and D.D. in the first phase; P.A., R.C. and A.B. in the second phase), who subsequently extracted data from pertinent articles. Due to the nature of the findings, the working group (all authors) opted for a narrative synthesis of the extracted information from currently available literature.
Results of the review
The American Fertility Society (AFS) Classification
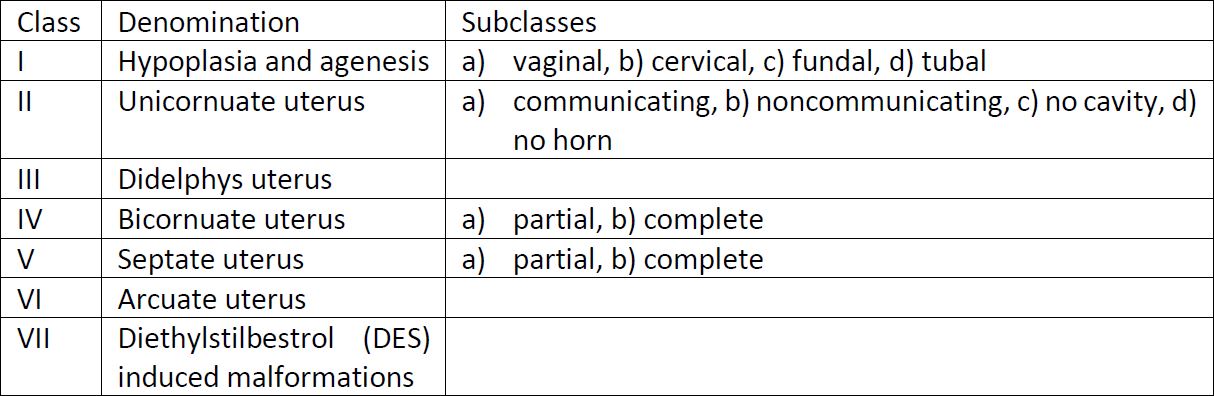
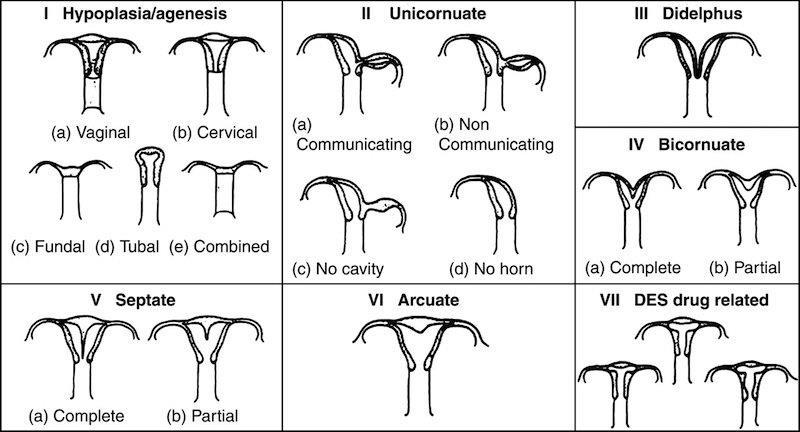
In 1988, the American Fertility Society (AFS), later renamed to the American Society for Reproductive medicine (ASRM), proposed a revision of the Buttram and Gibbons classification. This system became the most universally used classification system (7), containing seven basic groups. The classification is based on the degree of impaired Mullerian development and its interference with the fertility (9).
In this system (Table 1.), the anomalies are classified according to the major uterine pathoanatomic types. Vaginal, tubal and cervix anomalies are considered additional findings (10). This system is simple, user-friendly and clear (2). However, there are three most relevant disadvantages of this classification: (I) it is focused primarily on uterine anomalies (7), leaving vaginal, tubal and cervix malformations topic addressed inappropriately; (II) some congenital anomalies are not included, specially complex malformations; (III) the system lacks clear diagnostic criteria, relying on pictures depicting the anomalies without clear descriptive definitions of the female genital tract malformations (7).
Acién and Acién Classification
Acién and Acién proposed a classification of congenital female genital malformations in 1992 based on embryological and clinical features, and updated this system in 2004 and 2011 (1) (10). This classification takes into consideration embryological principles such as the fact that the mesonephric ducts and gubernaculum play a role in the adequate development of the mullerian ducts, helping in the distinction between groups and permitting also the classification of the anomalies beyond the uterine congenital malformations. The anomalies are divided into six groups. Although a classification system based not only on impaired anatomy but also on embryology seemed to be advantageous, most of the therapeutic options tend to restore the normal anatomy; thus, this classification has not been found particularly useful in clinical practice (2).
VCUAM Classification
Oppelt and collaborators came up with a new classification system in 2005 called Vagina, Cervix, Uterus, Adnexa and Associated malformations (VCUAM) (11). In this anatomical classification system, each organ is classified separately and it share some similarities with the tumor, node and metastasis (TNM) system for malignancies (11). This system´s main advantage is that it takes into account other commonly associated malformations (renal, skeletal, cardiac and neurological). It was initially validated in 99 patients (11). This system has never been widely accepted since it is not user-friendly. The anomaly is translated in a complicated succession of letters and numbers (for example, “V5b, C2b, U4b, A0, MR” corresponding to the Mayer-Rotitansky-Kuster-Hauser Syndrome)(2). Complete VCUAM classification can be consulted at https://www.fertstert.org/action/showPdf?pii=S0015-0282%2805%2902786-X.
The European Society of Human Reproduction and Embryology – European Society for Gynaecological Endoscopy (ESHRE-ESGE) Classification
In 2013, the ESHRE-ESGE, using a structured DELPHI procedure, published a classification system for Mullerian anomalies (12). This classification divides the anomalies into six classes based on anatomical and embryological principles. Sub-classes are based on anatomical variations of the main classes expressing different degrees of uterine deformity and being clinically significant. Cervical and vaginal anomalies are classified in independent supplementary sub-classes. The anomalies are described with numbers and letters (12).
ESHRE/ESGE has attempted to define uterine anomalies based on 3D ultrasound measurements of uterine wall thickness and external and internal fundal indentations, instead of using absolute numbers (e.g., indentation of 5mm) as the uterine wall thickness could normally vary from one patient to another (12). The defined uterine anomalies have not been correlated with reproductive outcomes (13). The arcuate uterus was considered normal, which may have an impact on management decision (5). According to the Congenital Uterine Malformation by experts of the CUME group, these cut-offs overestimate the prevalence of the septate uterus (14).
Although this system is an improvement of the pre-existing ones, being based on modern imaging methods (such as 3D ultrasound, histerosonosalpingograpy and hysteroscopy)(15), there are two main concerns: (I) there is no correlation between imaging findings and symptoms, treatment and obstetrical outcome; (II) it has not be externally validated. Complete classification can be consulted at https://pubmed.ncbi.nlm.nih.gov/23894234/.
In 2014, Ludwin and collaborators made a prospective study with a selected population to compare ESHRE-ESGE and AFS classifications. In this work, they came to the conclusion that ESHRE-ESGE classification was associated with an increase (almost 300%) in the frequency of septate uterus recognition. Most diagnoses of septate uterus according to the ESHRE–ESGE system corresponded to arcuate or normal uterus diagnosed by AFS, although the overall distinction between congenital uterine malformation and normal anatomy by both systems showed good agreement (16).
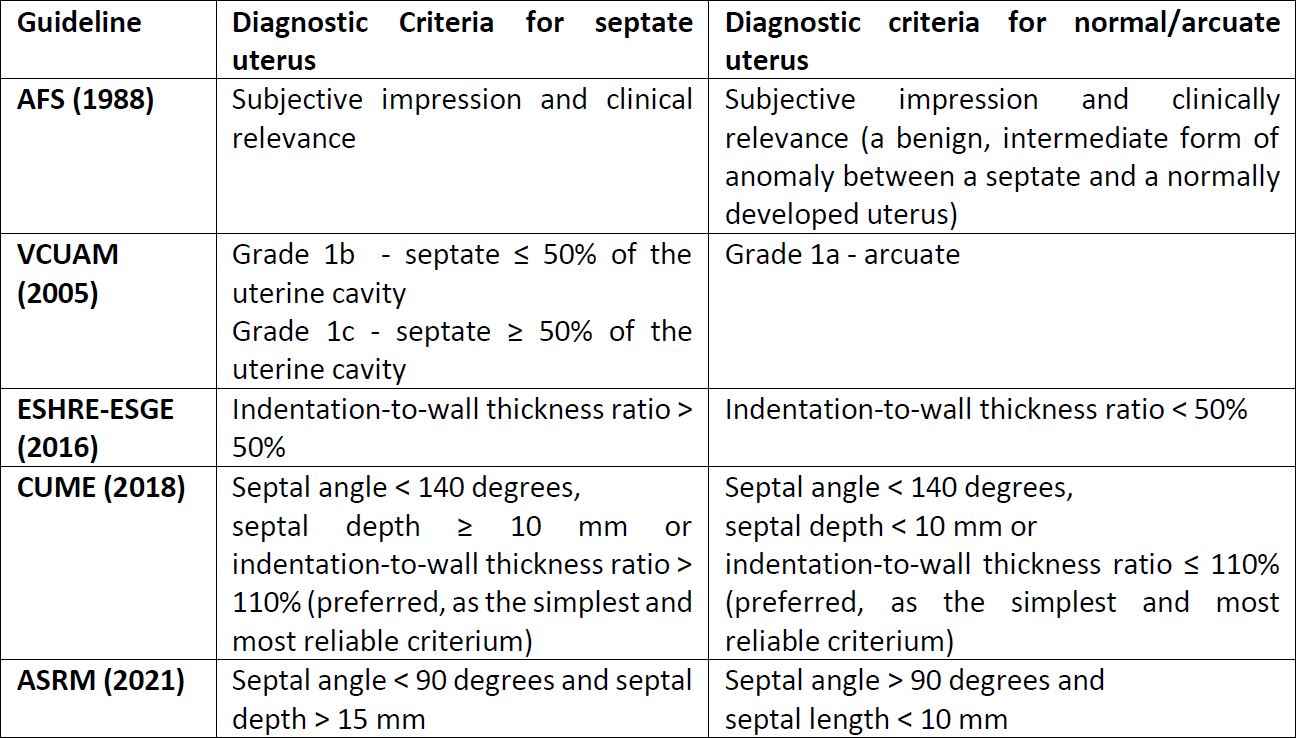
In 2016, the CONUTA CONgenital UTerine Anomalies Working Group (CONUTA), established during the ESHRE Campus Workshop on Female Genital Anomalies in Thessaloniki, reviewed the criteria proposed in 2013 and updated them, namely the definition of septate uterus (15), as presented in Table 2.
The American Society for Reproductive medicine (ASRM) Classification
The most recently published is the American Society for Reproductive (ASRM) Mullerian anomalies classification. This is based on AFS classification and divides the anomalies into nine categories, which one divided into five educational elements (variants, similar to, presentation, imaging and treatment) (17).
This classification has advantages to the previous ones because: (I) it is simple to use (relies on pictures); (II) has an interactive electronic format for educational proposes (link); (III) its categories are identified by descriptive terminology instead of codes with letters and numbers; (IV) it takes into account uterine, vaginal and cervical anomalies; (V) this classification recognizes the Mullerian anomalies as a continuum of the variation in the embryological development. Although this can be considered as a “true 21st century” classification with multiple online and interactive resources that even propose treatment, there are some critiques to be noted. Although this classification is presented as a simple, flexible and structured approach, some of the classification definitions are based on opinion of experts, rather than supported by scientific evidence (18). Also, there is a reported underestimation of the prevalence in the diagnosis of septate uterus, according to the Congenital Uterine Malformation Experts (CUME) group (14).
Most common malformations and diagnostic criteria discrepancies between classification systems
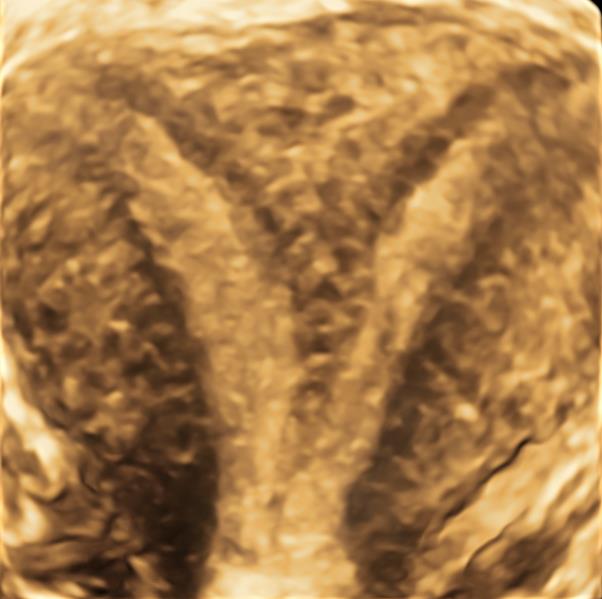
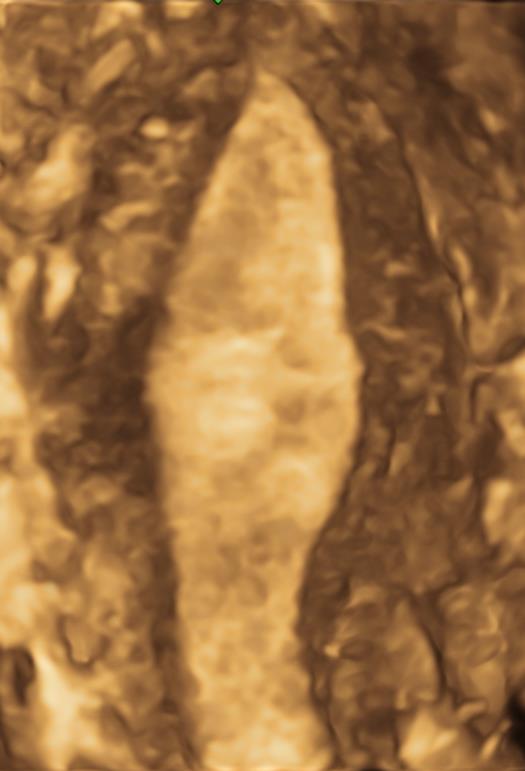
Septate uterus represents 55% of all Mullerian malformations and results from the lack of reabsorption of the median septum after the fusion of the müllerian structures. It can be classified as complete or partial depending on the moment when the failure occurs and has a deep impact in reproductive outcomes (19). On the other hand, arcuate uterus is considered a variant of the normal resulting from the failure in the final stage of reabsorption of the intermüllerian septum, with no clinical translation (9). Difficulties in differentiating between a normal/arcuate (Figure 1) and a septate uterus (Figure 2), inconsistent definitions and varying indications for surgery are associated with an increased likelihood of unnecessary iatrogenic treatment (14). The distinction criteria between normal/arcuate and septate uterus according to the most relevant classification systems are presented in Table 2. Even for the most frequent Müllerian anomalies, our literature search revealed that there is no international consensus on the criteria to be used. Moreover, while frequent non-extreme clinical situations are classified as pathological according to some systems, others consider them normal.
Discussion
Most of the criteria used in the diagnosis of Müllerian anomalies are based on anatomical, clinical and imaging data. Although physical examination is essential to detect vaginal and cervical anomalies, it should not be used for the diagnosis of uterine anomalies without complementary imaging studies due to lack of accuracy (15). In the past, laparoscopy and hysteroscopy were considered the gold standard for the diagnosis of these conditions. The surgical approaches are currently considered second-line because (I) they are (although minimally) invasive, (II) the diagnosis is mainly based on the subjective impression of the clinician(s) performing the procedures and (III) they evaluate primarily the uterine fundus (laparoscopy) and cavity (hysteroscopy) (20), providing no information on the uterine wall (15).
With technological progress, 3D ultrasound and MRI are now considered preferred tools to diagnose these anomalies. Although ultrasound is widely available, contrast-enhanced 3D sonography is currently recognized as the gold standard diagnostic technique. The 3D ultrasound is less operator-dependent than 2D ultrasound, having a better correlation with MRI (20), and providing high-quality spatial information on external contour, myometrium and uterine cavity (21). Hysterosalpingo-contrast-sonography is a non-invasive, cost-effective method that has high accuracy in identifying uterine anomalies (22). It is recommended to be performed during the early follicular phase to avoid pregnancy and artifacts. However, the distension of the uterine cavity could potentially modify the internal uterine contour resulting in false negative imaging of the uterine cavity (15). With increased usage of non/less invasive imaging techniques, the number of diagnosed cases have been increasing, including complex malformations which may not fit into any of the existing classifications.
Over the years, attempts have been made to classify all anomalies of the female reproductive system, initially from a purely anatomical point of view, later encompassing principles of embryology (5). As presented above, even in the most frequent situations, such as arcuate and septate uterus, there is still no consensus. The frequency and prevalence of these situations vary between studies depending on the applied criteria. On the other hand, complex abnormalities cannot be easily classified using any current classification system, contributing to a gap in clinical and research protocols. In our opinion, the major factor compromising the attempts to reach an ideal classification system is the lack of evidence-based data. Comparative multicenter international randomized control trials, including those focused on treatment outcomes and overall impact on women’s reproductive health, are greatly needed. In addition, it may be useful to group the patients who would benefit from the same treatment (medical and/or surgical), even with different anomalies, and evaluate the outcomes of offered management strategies.
Despite the challenges, it is crucial that international groups keep trying to standardize diagnostic criteria, allowing the development of therapeutic guidelines for multidisciplinary teams directly involved in the management of these patients including gynecologists, imaging specialists, pediatricians, general surgeons, urologists, among others. Meanwhile, when observing the patients, it´s of most importance to describe each detected malformation in detail, objectively, and to correlate it with the clinical presentation, regardless of how it will be classified by different systems. After a detailed description, it is adequate to classify the situation with the aid of two or more systems in parallel, if there is a discrepancy between the classifications, while the decision to implement a specific treatment should l be guided primarily, if not exclusively, by clinical relevance, i.e., clinical manifestations of the malformation.
Conclusion
Congenital malformations of the female reproductive system are increasingly diagnosed due to technological advances and the availability of imaging techniques, having a great impact on the well-being of women and couples, primarily due to their interference with the reproductive outcomes. Contrast-enhanced 3D sonography is the gold standard in diagnostics. Despite being many, there is no single ideal and universally accepted classification. A detailed and adequate description along with the correlation of the observed malformation with the associated symptoms are fundamental in the decision for the best treatment strategy. It is necessary to sustain international efforts and to conduct high-quality studies that offer evidence-based data in order to improve the classification and applicability of classification systems of congenital malformations of the female reproductive tract.
References
Table 1. AFS Classification system
Notes: Consult the images at https://www.researchgate.net/figure/American-fertility-society-classification-of-uterine-anomalies_fig1_320078833
Table 2. Diagnostic criteria for septate and normal/arcuate uterus as described by various classification systems
Figure 1. 3D ultrasound image of a normal/arcuate uterus with a cesarian scar niche
Figure 2. 3D ultrasound image of a septate uterus
Figure 3. 3D ultrasound image of T shaped uterus
Figure 4. 3D ultrasound image of an unicornuate uterus