Authors / metadata
DOI: 10.36205/trocar1.2023002
Abstract
This article provides a brief and evidence-based overview of the basic principles related to the evaluation and preparation of the patients planned to undergo diagnostic hysteroscopy. Anamnestic data should be taken and analyzed, general and pelvic physical examination performed, pregnancy and genital infections excluded, and a gynecological ultrasound realized. The patients should be advised about alternative diagnostic procedures and informed in details about the benefits, expected success of diagnostic hysteroscopy, but also about possible discomfort/pain and complications. In addition to adequate patient counseling, preparation for a successful hysteroscopy includes proper timing of the procedure and cervical ripening in selected women. Analgesia is addressed in a separated review of this journal issue. There are no evidence-based indications for antibiotic prophylaxis to be given before or during hysteroscopy.
Introduction
Hysteroscopy provides an accurate, minimally invasive and direct-vision approach to diagnose structural endometrial and uterine cavity pathologies associated with abnormal uterine bleeding (AUB) and reproductive failure, which may be congenital (e.g., uterine septa) or acquired (e.g., polyps, fibroids, adhesions) (1). Currently, in most cases, diagnostic hysteroscopy is performed on an outpatient basis, as a safe and well-tolerated technique, thanks to the progress of endoscopic technology, the use of minimal caliber instruments as well as the vaginoscopic approach to introduce the hysteroscope into the cervical canal and uterine cavity (2, 3, 4). As with any procedure involving uterine instrumentation, it requires appropriate preprocedural assessment and preparation of the patients to improve not only the diagnostic success but also the technique safety and patient comfort (5). The aim of this article is to provide a clear, brief and evidence-based overview of the basic principles related to the evaluation and preparation of the women undergoing hysteroscopy for diagnostic purposes.
Methods
non-systematic review of the literature published in English language until November 1st, 2022 was performed by searching PubMed using 3 search term combinations: (1) diagnostic hysteroscopy AND guidelines; (2) diagnostic hysteroscopy AND patient evaluation OR patient assessment; and (3) diagnostic hysteroscopy AND patient preparation. The abstracts were analyzed, pertinent articles included and the references of all included articles were also searched in order to find additional relevant articles. Through multiple cycles of literature review and discussion between the authors, consensus answers were reached to questions related to the clinical and imaging assessment of women before hysteroscopy, patient counseling, diagnostic hysteroscopy timing, cervical preparation and prophylactic antibiotic prescription. Pain management is addressed in a separated review of this journal issue.
Literature review
Preprocedural patient evaluation
The patient evaluation prior to performing diagnostic hysteroscopy aims to thoroughly characterize women who are scheduled for this exam, reducing the likelihood of both procedural failure and complications. In this important phase, anamnestic data are taken and analyzed, physical examination performed and pregnancy reasonably excluded (5). On this occasion, it is adequate to check whether gynecological (cervical) cancer has been adequately screened and to carry out screening if not. Before the diagnostic hysteroscopy, an anatomical examination of the uterus is performed, whereby ultrasound represents the first-line imaging approach (6).
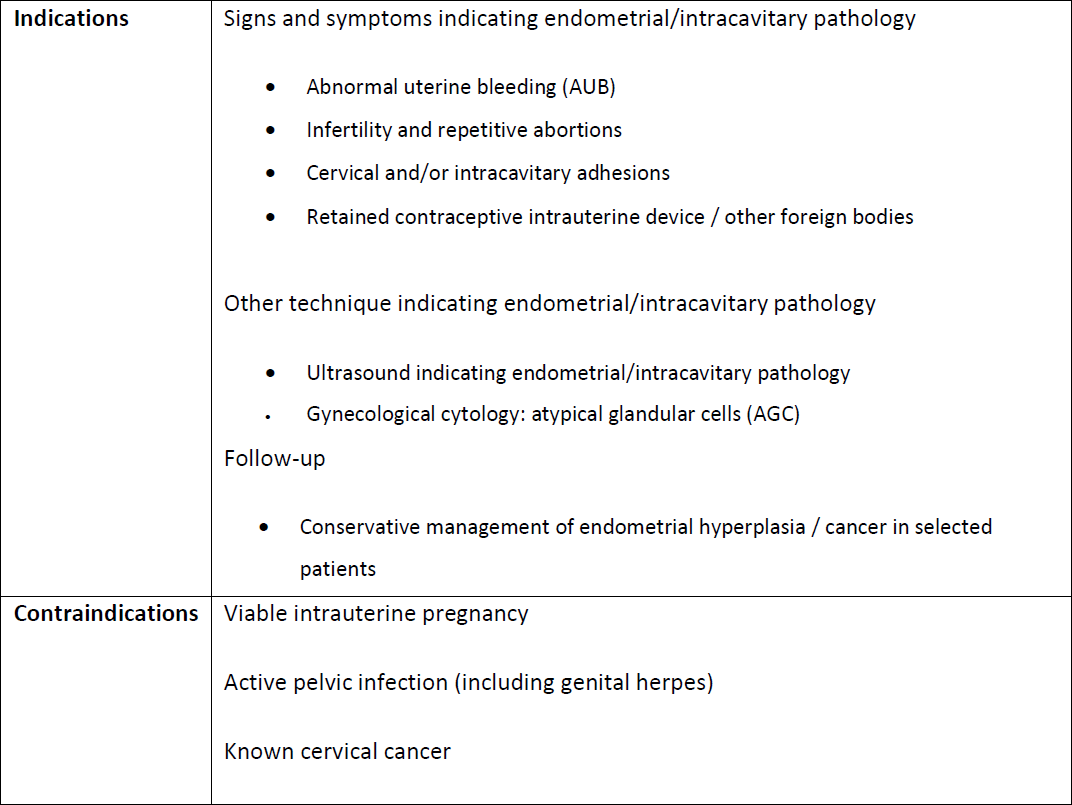
Medical history. Medical history taking is the initial step in the patient evaluation. Comprehensive data should be properly structured. Particular attention should be paid to the symptoms [all, but especially those that indicate hysteroscopy (Panel 1.)] and previous treatments, as well as obstetric/gynecological history, comorbidities, previous surgeries, medications, allergies and habits (6).
Physical examination. A general and complete abdominal and pelvic physical examination should be performed. Particular attention should be paid to the characteristics of the uterus that affect the performance of the hysteroscopic technique, including the position, size, mobility and cervical patency (6). It is appropriate to carry out cervical cancer screening on this occasion, if indicated and not previously performed in accordance with current national/international guidelines (7). Observation of the signs of cervicitis indicates the need to sample material for cervical cultures. Infectious and other contraindications for hysteroscopy are shown in Panel 1.
Laboratory testing. For the performance of diagnostic hysteroscopy, especially in outpatient settings, no laboratory tests are required, unless it is indicated by specific anamnestic data or clinical circumstances. In women of reproductive age, if the procedure is not scheduled immediately after menstruation, a pregnancy test may be needed (5).
Anatomical uterine assessment by imaging. Although hysteroscopy is considered the diagnostic gold standard for endometrial and intracavitary pathology, ultrasonography represents the first-line assessment tool (along with the clinical examination) for anatomical evaluation of the uterus in patients with symptoms and signs suggestive of endometrial and/or myometrial lesion(s). Well-known ultrasound advantages include its availability, noninvasiveness, reliability and cost-effectiveness (8). Transvaginal ultrasound (TVUS) offers better resolution then abdominal ultrasound (9), which is useful, due to its wide vision, to exclude or, when present, to evaluate pathology extending beyond the pelvis (6). A consensus opinion from the International Endometrial Tumor Analysis (IETA) group on the terms, definitions and measurements to describe the sonographic features of the endometrium and intrauterine lesions was published in 2010 (10). The Morphological Uterus Sonographic Assessment (MUSA) paper, published in 2015, provides a consensus statement on terms, definitions and measurements that can be used to describe and report normal and pathological myometrial findings during an ultrasound examination (9). The use of standardized methodology to assess the uterus (both endometrium and myometrium), as well as common definitions and terminology to report findings is highly desirable, resulting in reduced intra- and inter-observer variability and better communication between sonographers, sonologists, gynecologist, other clinicians and researchers (6, 9, 10). The typical ultrasound features of endometrial atrophy, polyps, hyperplasia and cancer, and intracavitary leiomyomas, in symptomatic and asymptomatic women, have been described using the IETA terminology (11, 12). In patients with AUB, the TVUS detection of some easy-to-assess IETA features (endometrial thickness < 3 mm, three-layer pattern, linear midline and single vessel without branching) makes endometrial cancer unlikely (11). When endometrial malignancy is suspected by ultrasound, blind sampling is often performed, followed by diagnostic hysteroscopy and direct-vision biopsy in cases where the diagnosis of malignancy is not confirmed by pathohistological examination. Hysteroscopy is a safe diagnostic method and has no significant effect on the prognosis of early-stage endometrial cancer (13).
Contrast-using saline-infusion sono-hysterography (SIS) and gel-instillation sonohysterography, in two (2D) or three dimensions (3D), are very accurate diagnostic procedures to describe submucous leiomyomas (14, 15, 16), cesarean scar niche (17, 18, 19) and congenital uterine malformations (20, 21). For instance, in accordance with a Cochrane systematic review and a 2017 systematic review and meta-analysis of 1398 citations and 5 studies, high-quality evidence supports that SIS is equally performant as hysteroscopy to diagnose submucous leiomyomas (6, 15, 22). By defining the extent to which a leiomyoma protrudes into the uterine cavity and, in parallel, the depth of myometrial penetration by the lesion, SIS provides the information analog to that from the combined use of hysteroscopy and TVUS (23). If an atypical intracavitary leiomyoma is observed during the pre-hysteroscopy ultrasound assessment, the 2017 ISGE guidelines for the assessment of the sarcoma risk can be used (24).
Informed consent and patient preparation for diagnostic hysteroscopy
Diagnostic hysteroscopy is a minimally invasive and generally safe procedure (5). However, patients planned to undergo diagnostic hysteroscopy should be advised about alternative diagnostic procedures, as well as informed about the benefits and expected success of the procedure, but also about possible discomfort/pain and complications. They should be informed about the possibility of abandoning or prematurely ending the procedure due to complications, intolerance or the impossibility to introduce safely the hysteroscope into the uterine cavity. The patients should agree to undergo eventual laparoscopy or laparotomy if necessary to rule out iatrogenic visceral or vascular pelvic injury. The patient should receive an explanation about the limits for hysteroscopy, after which the procedure must be stopped immediately even if it is not completed due to the complications that could arise or to the patient’s significant discomfort (detailed in the articles “complications” and “pain management of this monothematic issue). It should be noted that in such a case it will be necessary to schedule another hysteroscopic procedure. Also, the patient should receive information about transient symptoms (primarily pelvic discomfort and spotting) that she may have even after an uncomplicated hysteroscopy, about the expected duration and ways of controlling the discomfort, as well as about the expected time for returning to daily routines and work. The most common reasons for failure to complete outpatient hysteroscopy are pain, cervical stenosis and poor visualization (25). Thus, the preparation for successful ambulatory hysteroscopy includes adequate patient counseling, procedure timing, considerations related to pain management, and cervical preparation in selected women.
Timing and endometrial preparation. While in postmenopausal patients, diagnostic hysteroscopy may be performed at any time, in premenopausal women, specifically the follicular or luteal phase may be of interest to study (26). Most authors perform hysteroscopic examinations in the proliferative phase, when the mucosa is thinner, in order to avoid misinterpretation of physiological changes and their confusion with polypoid or hyperplastic endometrium (5, 26). Furthermore, the increased tonus of the cervix caused by the luteal phase progesterone is avoided, thus facilitating the technique (26).
Some women with unpredictable menstruation may be scheduled for hysteroscopy at any time, but visualization may be impaired by active bleeding. Pharmacologic thinning of the endometrium, i.e. pretreatment with combined oral contraceptives, progestins alone or gonadotropin-releasing hormone (GnRH) agonists may improve visualization by thinning of the endometrium (27, 28, 29, 30, 31). Thinning agents should be avoided whenever possible when only diagnostic hysteroscopy is planned, as these hormones may affect endometrial histology.
Cervical preparation. Almost 50% of hysteroscopic complications are associated with difficult insertion of the hysteroscope through the cervical canal into the uterine cavity (25). Many patients do not require cervical dilatation for diagnostic hysteroscopy, particularly premenopausal women undergoing the procedure with a narrow caliber (<5 mm) hysteroscope. Although there is insufficient evidence to support routine cervical ripening prior to diagnostic hysteroscopy, it may be considered for patients with cervical stenosis and/or at increased risk of pain with the procedure (5). According to a systematic review and meta-analysis of 19 studies focusing on cervical ripening before operative hysteroscopy, both pre- and postmenopausal women treated with misoprostol were significantly less likely to require additional mechanical dilation than women who were untreated or treated with dinoprostone or placebo (32). Many practitioners extrapolate these data and apply them to diagnostic hysteroscopy.
The use of misoprostol reduces the hysteroscopy complication rates, being associated with adverse effects, primarily abdominal pain, fever and vaginal bleeding (32). Most often 200 – 400 micrograms of misoprostol are given orally or vaginally, resulting in easier entry into the cervical canal, reduced pain perception, and shorter procedure time (33, 34). Intravaginal misoprostol (400 micrograms) has been shown to reduce pain associated with office hysteroscopy, during and after the procedure, when administered at least 4 hours before the procedure (35). Vaginal estrogen (25 micrograms) administered two weeks before the procedure, together with 400–1000 micrograms of vaginal misoprostol applied 12 hours before the procedure, facilitates dilatation of the cervix and significantly reduces pain in postmenopausal women (36, 37).
Prophylactic antibiotics. Infection occurs in <1% of women undergoing hysteroscopy (38). There is no evidence-based indication for antibiotic prophylaxis to be routinely given before or during hysteroscopy to prevent surgical site infection or endocarditis (5).
Conclusion
An adequate patient assessment and preparation prior to performing diagnostic hysteroscopy is essential to reduce the likelihood of procedural failure and complications, and to improve patient tolerance and satisfaction. After clinical history taking, physical examination and gynecological ultrasound, confirmation of indications and exclusion of contraindications for diagnostic hysteroscopy, preparation for a successful hysteroscopic examination includes appropriate patient counseling, timing of the procedure and cervical preparation in selected women. This preprocedural phase requires attention, training and updating according to new evidence that may appear in the literature.