Metadata
DOI: 10.36205/trocarAB.20231
Section 1 | Endoscopy and MIGS
Paravaginal Repair and High Uterosacral Suspension: An Alternative to The Mesh?
- Inge Putri
- Introduction: Surgery for anterior wall prolapse from the lateral detachment secondary to paravaginal defect able can be performed laparoscopically, this approach is able to reduce the risk of vaginal shortening (1). Compared to anterior colporrhaphy, the laparoscopic paravaginal repair is a much more anatomic repair of anterior vaginal wall prolapse caused by lateral defects (2).
Objective: To describe our technique for robotic assisted paravaginal repair (level 2 support) along with high uterosacral suspension (level 1 support).
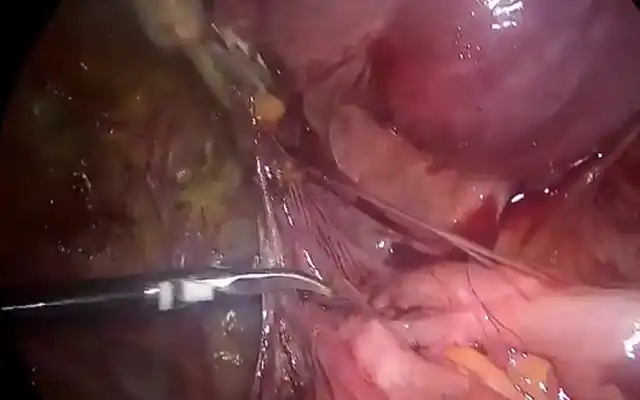
- Methods and results: We present a case of a 55-year-old patient who had recurrent symptomatic prolapse following an anterior repair, posterior repair, as well as sacrospinous fixation and vaginal hysterectomy performed 18 months ago. She was a Para 4, with a history of normal vaginal births and BMI 30. Findings preoperatively was Aa +1, Ba +2, Ap +2, Bp +2, C 0, as well as a widened genital hiatus. Prior to surgery, her preoperative assessment was Aa +1 Ba +2 C -10 Ap -2 Bp -2 Pb 3 TVL 10 Gh 3. She was also found to have shallow vaginal fornixes, secondary to paravaginal defect. Firstly, we establish the retropubic space through backfilling of the bladder with normal saline, in the setting of previous anterior repair, meticulous dissection was performed through adherent tissues. Secondly, the lateral aspect of the anterior vaginal wall is sutured to the arcus tendinous fascia pelvis (ATFP), or the “white line”, this re-approximation of vaginal wall to fascia overlying obturator internus muscle will restore bladder and bladder neck to its normal anatomical position. This repair is performed bilaterally with a nonabsorbable Ethibond excel sutures and knots are tied intracorporeally. Following this, the uterosacral ligaments are identified and the space of Okabayashi is opened to identify ureters and bladder peritoneum opened and bladder dissected away to reveal the pubo-vesical fascia. A non-dissolvable suture (0 Ethibond excel or 0 Prolene suture) is used to plicate the uterosacral ligament to the bulky uterosacral ligament to the peri cervical ring and incorporating the rectovaginal fascia. Following this, the suture is tied intracorporeally with 5 squared knots. The procedure is then repeated on the other side.
- Conclusion: We consider this technique an armamentarium to the routine vaginal route of prolapse repair.
- References: 1. Chinthakanan O, Miklos JR, Moore RD. Laparoscopic Paravaginal Defect Repair: Surgical Technique and a Literature Review. Surg Technol Int. 2015;27:173-183.
2. Maher C. Laparoscopic paravaginal wall repair, retrieved from https://urogynaecology.com.au/laparoscopic-paravaginal-repair/ on Dec 9 2022
Overcoming the Giants, Managing the Difficult Total Laparoscopic Hysterectomy
- Inge Putri
- Objective: To demonstrate different techniques in navigating a difficult Total Laparoscopic Hysterectomy
- Methods: To showcase a video presentation in overcoming the more challenging cases of performing total laparoscopic hysterectomy, when bowel adhesions are encountered in a patient with a prior midline laparotomy, when bladder adhesions are present, as well as reducing blood loss in a large multifibroid uterus.
- Results:
- Stop and be cautious of bowel adhesions
– Only divide adhesions that is restricting access to pathology or contributing to patient’s symptoms
– Visualise adhesions from multiple angles, to gauge their full extent and assess omental/ small or large bowel involvement
– If you can see through it, you can cut through it (transparent adhesions)
– Cold scissors should be used – particularly for dense adhesions
– When in doubt, leave fascia on bowel. - Slow down and carefully assess the adherent bladder
– The low lateral approach is used to find the avascular plane between bladder and cervix - Go to the pelvic side walls and reduce bleeding at its source
– Open the round ligament and broad ligament to allow for retroperitoneal dissection to the origin of the uterine artery from the anterior branch of the internal iliac artery following location of the obliterated umbilical artery and ureterolysis. This should be done bilaterally.
- Stop and be cautious of bowel adhesions
- Conclusion: Laparoscopic hysterectomy is proven to have multiple patient benefits such as lesser pain and shorter hospital admissions. When encountered with challenges of a difficult laparoscopic hysterectomy, it is important to approach them in a systematic manner as described.
- References:Bryant-Smith A, Bowel adhesions: Divide and conquer! 2019 AGES Annual Scientific Meeting 2020.
Eisner IS, Wadhwa RK, Downing KT, Singhal PK. Prevention and management of bowel injury during gynecologic laparoscopy: an update. Curr Opin Obstet Gynecol. 2019;31(4):245-250.
Foley C. A stepwise approach to the difficult bladder flap to prevent urinary tract injury during laparoscopic hysterectomy. 2019
A 5-Years’ Experience of Total Laparoscopic Hysterectomy Without Uterine Manipulator. Single Institution Retrospective Study Of 882 Cases.
Tamriko Dzotsenidze, Irakli Todua, Tamar Giorgadze, Mariam Matcharashvili, Medical Canter “Innova” Tbilisi, Georgia.
Email: tamro_dz@yahoo.com Phone number: +995595115115 Presenter: Tamriko DzotsenidzeObjective: The aim of the retrospective study was to investigate the feasibility and safety of the total laparoscopic hysterectomy without uterine manipulator.
Methods: This is the retrospective study of cases of total laparoscopic hysterectomy without uterine manipulator, performed in one institution between January 2016 and March 2022 in women with benign indications for hysterectomy. The patients’ medical records were used as the database for the study, surgical procedure details, intra and postoperative complications were evaluated.
Results: 882 cases of Total Laparoscopic Hysterectomy (TLH) from January 2016 to March 2022 are reported. Mean age of patients was 52,8 years (range, 29 – 88 years), approximately half of the patients were postmenopausal. BMI ranged between 23.4 kg/m2 and 44, 3 kg/m2 the mean operative time was 37 minutes (range, 25-110 minutes). The estimated blood loss was 59.6 ml (range, 20-200 ml), the median uterine weight was 273,3 g.(45-780g), the average length of stay in hospital was 58 hours (range 47-71 hours). Total number of complications was 28 (3.2%). Intraoperatively there were five cases of conversion to laparotomy (0.6%), due to large uterine size, a ureteral stent was placed in three cases (0,3%). Laparoscopic revision was performed in five cases (0,6%) because of pelvic haematomas. Urinary tract infection in six cases (0,7 %), blood transfusion was performed in seven cases (0.8%), including 3 cases of preoperative blood transfusion due to severe anaemia. We reported two cases of vaginal vault dehiscence in the postoperative period, managed through vaginal approach. A positive correlation was revealed between uterine weight and intraoperative blood loss volume. (Pearson Correlation =0,564, P<0.001.)
Conclusion: The study shows that THL without uterine manipulator is the feasible and safe procedure due to its low complication rates, short operative time and hospital stay.
Early-stage Cervical Cancer with Tumour Size under two centimetres associated with good safety and comparable efficacy outcome in minimally invasive surgery compared with abdominal radical hysterectomy: systematic review and meta-analysis.
- I Gusti Bagus Mulia Agung Pradnyaandara1, I Gde Sastra Winata2
1 Faculty of Medicine, Udayana University, Prof. IGNG Ngoerah General Hospital, Denpasar, Bali, Indonesia
2 Department of Obstetrics and Gynecology, Faculty of Medicine, Udayana University, Prof. IGNG Ngoerah General Hospital, Denpasar, Bali, Indonesia. Background: Abdominal radical hysterectomy (ARH) is the standard treatment for early-stage cervical cancer (ECC). Optional treatments using minimally invasive surgery (MIS) are still debatable.
Objective: To compare efficacy and safety of MIS and ARH in ECC.
Methods: Relevant literature in databases were retrieved from 2012-2022. Studies comparing MIS (Laparoscopic/Robotic) and ARH in ECC were involved. Primary outcomes involved overall survival (OS) and disease-free survival (DFS) for efficacy. Blood loss, intra and post-operative complications categorized as safety outcomes. In addition, we performed sub-analysis based on tumor size, year of event, and type of MIS. Meta-analysis was performed by RevMan 5.4
Results: 42 studies involving 26.636 patients were included. Although DFS is superior in ARH (OR=1.49;95%CI=1.27-1.74; p<0.00001), in sub analysis group with tumour size ≤2cm, MIS wasn’t inferior compared to ARH in 5-year DFS (p=0.07). MIS and ARH had no difference in OS (p=0.07), but patients with tumour size >2cm at 5-year OS, MIS showed inferiority (OR=1.76;95%CI=1.06-2.91; p=0.03). MIS has better safety outcome in blood loss (MD=(- 198.5);95%CI=(-262.4) -(-134.36);p<0.00001). Although there was no difference in total intra- operative complications, robotic subgroup was significantly better than ARH (OR=0.35;95%CI=0.18-0.68; p=0.002).
Conclusion: MIS is proven have good safety outcomes. Adjusting tumour size, especially ≤2cm has potential to provide efficacy outcomes comparable to ARH.
Laparoscopy as an Effective Microsurgery Option for Niche Repair Without Hysteroscopy Assistance.
- Irwanto Thengkano1, Ashon Saadi2, and Relly Yanuari2 1Trainee Obgyn FER,
2Staff Obgyn FER Department of Obstetrics and Gynecology Dr. Soetomo General Hospital, Faculty of Medicine Airlangga University, Surabaya Introduction: The rising rate of Caesarean Section (CS) in recent decades increases the risk for surgical incisions scar in the uterine wall to rise. The uterine scar defect or insufficiency caused by incomplete healing of myometrium is also called niche, isthmocoele or scar dehiscence. A niche with as result an indentation is reported to be the highest risk factor associated with symptoms of abnormal uterine bleeding, dysmenorrhea, chronic pelvic pain, subfertility, and near uterine rupture during a subsequent pregnancy(1). The reported incidence of niche complications is 1,9% of CS cases, 30% of cases are found 6-12 months after CS. Some rreconstructive niche surgery often uses a dual laparoscopic approach with the aid of observation illuminated by the hysteroscope (2,3).
Case: We report a case Mrs. N, 31 years old post CS 115 days before. The main complaint of this patient is heavy-frequent menstrual bleeding with irregular bleeding episodes (Abnormal Uterine Bleeding (AUB)). The AUB episodes did start one month after the second SC. The indication for the last CS was placenta previa accompanied by antepartum bleeding, alive baby weighing 2300 gram at birth. When the patient has been referred to our clinic with a diagnose anaemia caused by AUB caused by the dehiscent uterine scar (niche). Patient and partner still have the desire to become pregnant again. At the department be main clinical examination consists of using ultrasound examination and evaluation. Maximizing the function of the transvaginal ultrasound and sonoinfusion sonography. The diagnostic tools used are color doppler imaging and 4-dimensional (4D) imaging Ultrasound results: uterus in anteversion Ø 7.89 x 4.49 x 3.65 cm. Endometrial thickness: 8.9 mm, homogenic and hypoechoic appearance. A defect was found on the interior wall of the right lateral lower uterine segment in the shape of an inverted “V” with a width of 0.85 and a depth of 0.51 cm with increased vascularity. The niche area > 2 cm square and the residual myometrium did measure 1,8 – 2,6 mm. Located 0.8 cm from the right uterine artery, no free liquid in the Douglas pouch. Right Ovary: 1.76x 1.16×2.38 cm. Left Ovary: 1.98x 1.81x 1.78 cm. These results point at a high risk for uterine wall perforation if operative hysteroscopy is performed.
Laparoscopic Procedure: Laparoscopy for niche repair was performed at 25 August 2022 at 411 Operating theatre in Dr. Soetomo hospital qualified as an urgent surgery. Operation time 1 hr and 25 minutes with less than 50 cc measured blood loss. The sequence of steps during operation is as follows: remove the uterine attachment, identify the niche area with the injection of methylene blue into uterine cavity, excise the uterine scar and separate the peritoneal lining, suture the uterus using the 1-layer vertical mattress sutures using the “far-near-far-near” technique with a distance of ± 0,8 cm, testing of the watertightness of the anterior wall uterine suture with repeated injections of methylene blue solution to the uterine cavity, and interrupted reperitonealization. The materials used during the operation are: methylene blue contrast liquid using a pediatric catheter whose tip is inserted into the uterine cavity, monofilament thread which is absorbed for the size number 1 and 4.
Clinical Discussion : The accuracy of choosing a laparoscopic surgery technique over a laparotomy is an advantage considering the principles of gynecology micro-reconstructive surgery (3). The advantages of laparoscopic surgery in these patients include the reduced potential for infection. Lack of touching the organ by the operator’s hands and a good control of the bleeding can reduce postoperative adhesions. The Halstedian principle, maintaining tissue wet, is more easily controlled by irrigation. Precision electrocautery can reduce the amount of tissue damage due to desiccation. Smaller instruments and optical visibility and lighting help operators to perform actions in reduced operating fields. However, the laparoscopic technique is highly dependent on the skills of the operator (4). To improve the outcome of suturing in this case, the correct way is to start removing the tissue adhesions around the niche. Identify niche position, depth and breadth of niche and ischemic areas. Tissue debridement or resection are carried out by minimizing tissue trauma guided by the blue tissue area. A suture in a far-near-near-far vertical mattress way is appropriate to bring the myometrial tissue closer to the inside and outside. The vertical mattress technique ensures vascularization of the uterine arteries that run vertically lateral to the uterus in most of the cases. This suturing pattern can bring the two sides of the myometrial tissue closer from inside to the outside and does not cause indentations on the inner and outer suture surfaces. The choice of thread for this procedure is appropriate based on the principles of microsurgery. The fact of separating the serosa of the uterus, as wide as one cm from the wound edges, to prevent distortion of the architecture of the uterine wall at suturing will also accelerate the tissue integration. After suturing the myometrium and testing for water tightness, one can continue with the reperitonealization sutures (5,6,7,8). The healing period of tissues of the myometrium operated upon depends not only on the surgical technique but also on the general condition of the patients and hormonal cyclic influences on the uterine muscle. Post operative patient follow up can also be done by observing the menstrual pattern. The choice of combined oral contraception is the right choice for mothers who are not in the exclusive breastfeeding period. The period of giving combination oral contraception in the literature varies greatly, at least 12 months of use as a dual function for contraception (1,3).
Conclusion: The presence of AUB within 6-12 months after CS must be considered for ultrasound evaluation with suspicion of niche. Optimizing the use of transvaginal ultrasound examination is very useful for the diagnosis and the description of the conditions that will be encountered during surgery. Laparoscopy is an appropriate choice for the application of the microsurgery principles on the reproductive organs in cases where niche repair is mandatory. The vertical mattress suturing technique with a ’far-near-far near’ pattern is one of the right choices. The use of short-term combined oral contraceptive methods is an appropriate choice during post laparoscopy transvaginal ultrasound follow up.
References:
- Vissers, J. et all.2020. Post-Caesarean section niche-related impaired fertility: hypothetical mechanisms. Human Reproduction, Vol.35, 7:1484-1494.
- Situmorang, H., et all. 2020. Double Approach(Laparoscopy and Hysteroscopy) Repair of Isthmocele (Niche). A Case Report. Indones J Obstet Gynecol. Vol 8, 4:254-257.
- Zang N.N., et all. 2021. Novel laparoscopic surgery for the repair of caesarean scar defect without processing scar resection. BMC Pregnancy and Childbirth. 21:815.
- Brown, K, Tkacz, Z. 2021. Hysteroscopic and laparoscopy management of caesarean scar (niche) defects in symptomatic patients. Journal of Obstetrics and Gynaecology. Vol 38, 5: 730
- Darwish, AMM. 2011. Reconstructive Endoscopic Myomectomy. In: Darwish, A (Ed). Advanced Gynaecology Endoscopy. Department of Obstetrics and Gynaecologic Women’s Health University Hospitals Assiut, Egypt. 11 (163-176)
- Kuder, M.H., et all. 2009. Sutures and suturing techniques in skin closure. Indian J. Derm. 75:4.
- Huirne, J.A.F., et all. 2017. Technical aspects of the laparoscopic niche resection, a step-by- step tutorial. European Journal of Obstetrics & Gynaecology and Reproductive Biology.219:106-112.
- Gomel, V.MD., 2016. Microsurgical principles and post operative adhesions: Lesson from past. Fertil Steril. 106:1025-31
Twin Pregnancy After Laparoscopic Myomectomy of Subserous Myoma: A Case Report
- Mahida El Shafi1, Arif Tunjungseto2
1 Obstetric and Gynecologic Resident, Airlangga University/ Dr. Soetomo Hospital Surabaya, Indonesia
2 Fertility Division Staff, Obstetric and Gynecologic Airlangga University/ Dr. Soetomo Hospital Surabaya, Indonesia
Correspondence: Mahidael2204@gmail.com Objective: The purpose of this article is to report a case of laparoscopic myomectomy in an infertile patient.
Methods: We report the case of a 27 years old women who is referred to our hospital with abdominal distension and vaginal bleeding. An ultrasonic examination confirms a uterus containing a subserous myoma of 4,34 x 2,31 cm. Preoperative we performed a SIS procedure to evaluate the implantation of the myoma. At Laparoscopy an enlarged uterus was found (myoma 6 x 6 cm on the posterior side of the uterus). We decided to perform a myomectomy where we penetrated 4-5 cm into the uterine cavity. The endometrium was repaired with a continuous suture and the myomectomy wound was sutured in two layers with monofilament. The entire myoma was removed using a morcellator. The total duration of the operation was 55 minutes.
Result: Three months post-surgery the patient experienced a spontaneous twin pregnancy.
Conclusion: Laparoscopic myomectomy offers advantages as compared to laparotomy; as there are as a small incision, a fast recovery, reduced postoperative pain and first choice surgery for women in their reproductive age who desire fertility. Laparoscopic myomectomy does significantly improve patient’s fertility rate in subserous myoma depending on the age of the patient, the diameter of myoma and the location of myoma.
Successful Laparoscopy Assisted Extirpation of a Very Large “Born” Myoma, a Vaginal Prolapse of a Type I Intramural – Submucosal Leiomyoma with a three cm Stalk: A Case Report.
- Dina Priliasanti Subroto1, Muhammad Yohanes Ardianta Widyanugraha2, Relly Yanuar Primariawan2
1Residence, Obstetric and gynecologic Airlangga University/ Dr. Soetomo Hospital Surabaya 2Fertility Divison Staff, Obstetric and gynecologic Airlangga University/ Dr. Soetomo Hospital Surabaya
Correspondence: dnprilia@gmail.com Phone: +6281230304448 Objective: This article is reporting a case of a rare vaginal prolapse of a type I intramural – submucosal leiomyoma, with the size of a “baby head”. It is a Type I leiomyoma, mimicking a Type 0 appearance because of its pedunculated stalk connecting the intramural with submucosal part of the myoma. The submucosal part did grow, prolapsing beyond the cervix, to be “born” and visible at the vaginal introitus. Although leiomyomas are common, submucosal leiomyomas prolapsing are uncommon. Moreover, a very large vaginal prolapse of a type I leiomyoma is rare. Vaginal extirpation is common for the Type 0 leiomyomas, whilst laparoscopic myomectomy is the common technique for type I, suggested to be performed if the mass does not exceed ten cm and their number does not exceed four. Despite its huge size, we decided to stick with minimally invasive treatment for its advantages by combining both techniques.
Methods : A 35-year-old nulliparous, unmarried, woman complaining of AUB had been hospitalized and given several blood transfusions due to severe anaemia with the lowest Haemoglobin level at 2,6 g/dL. A bulky mass was visible at the vaginal introitus. An MRI found the submucosal part to measure 15,86 x 9,67 x 8,82 cm and the intramural part of 2,92 cm, with a +/- 3 cm stalk-form connecting both parts. Laparoscopy was performed. The intramural part was excised at the margin of the peduncle and pulled out using laparoscopic Kocher’s. The remaining intracavity mass was pulled out by vaginal gentle pulling and twisting, extracting its prolapsed vaginal portion using a myoma extractor device. The uterine defect was stitched using a baseball suture by laparoscopy. At the end of the procedure an IUD was inserted to prevent adhesions. The operation went without any significant difficulties.
Result: Postoperatively the patient remained in the hospital for five days, and was discharged in good condition without AUB or other significant complications. Patient was relieved and happy with the result.
Conclusion : The management of leiomyomas depends on the symptoms, the myoma characteristic, and the need to preserve fertility. In this case, we discussed the best treatment to be most beneficial to the patient. Minimally invasive surgery was chosen for its advantages of being less traumatic, quicker recovery, and possibility to preserve fertility.
Uterus Unicornis with Haematometra presenting with a Non-Communicating Left Horn and a history of Abdominal Pregnancy: A Rare Case
- Arinil Haque1, Jimmy Yanuar Annas2
1Resident, Obstetric and gynecologic Airlangga University/ Dr. Soetomo Hospital Surabaya
2Fertility Divison Staff, Obstetric and gynecologic Airlangga University/ Dr. Soetomo Hospital Surabaya
Correspondence: vearine.ah@gmail.com Objective: The uterus unicornis with non-communicating horns is a rare Müllerian anomaly (incidence 0.06%). The condition is complicated by severe pelvic pain due to haematometra or endometriosis causing retrograde menstruation. The aim this study is to describe a case of uterus unicornis with non-communicating horns with the aim to prevent delayed diagnosis and serious complications.
Methods: This case report concerns a 39 year out female, presenting with as main complaint severe dysmenorrhea for 5 years. The patient had been treated by hormonal therapy but the complaints did not diminish. Her only child is 19 years of age and in her history an abdominal pregnancy. Ultrasound resulted in detecting an endometrioma of 2.8 x 3 cm. The patient was planned for laparoscopic surgery and at surgery a uterus unicornis was found at the right side of the patient with a normal cervix and further a haematometra in a non-communicating left horn which did rupture upon release of the adhesions present causing chocolate fluid leakage. There was also a left side endometrioma of 3 x 3 cm. Hysterectomy and bilateral salpingo-oophorectomy were then performed.
Result: The correct diagnosis of uterus unicornis with non-communicating horns has important clinical implications, but is sometimes misdiagnosed. The abdominal pregnancy in this patient could occur in the rudimentary horn following transperitoneal migration of sperm or zygote and would have resulted in a life-threatening situation if it ruptured. Severe dysmenorrhea during hormonal therapy in this patient can be caused by the haematometra in the non-communicating left horn and the endometrioma. Laparoscopic hysterectomy was chosen to remediate to the main complaint.
Conclusion: The uterus with unicornis with non-communicating horn is a rare condition, but it can cause serious complications. Laparoscopy was essential to confirm the diagnosis and should be considered as therapy to avoid associated morbidity.
Davydov Procedure in Mayer-Rokitansky-Küster-Hauser Case
- M. Dimas Abdi Putra1; Azami Denas1 †; Jimmy Yanuar Anas2 1Urogynecology Reconstructive Division
2Fertility Endocrinology Reproduction Division Department of Obstetrics and Gynecology dr. Soetomo General Hospital – Medical Faculty of Airlangga University Objective: Reporting one case of Davydov procedure in a Mayer-Rokitansky-Küster-Hauser (MRKH) case where the neovagina successfully did remain patent.
Case: We report the case of a 26 years old married woman complaining of primary amenorrhea and unable to have intercourse. At clinical evaluation, the findings are that the secondary sexual characteristics are positive, chromosome examination reveals 46 XX, and at gynecologic examination, the vaginal opening is not present. MRI examination results showed a rudimentary uterus, and normal ovaries. The diagnosis of MRKH. Davydov procedure was chosen for the creation of a neovagina. A vaginal mould has been placed for three months, and post-operative dilator application was routinely applied. FSFI questionnaire is used for evaluating the sexual function.
Result: The patency of the neovagina has been successfully obtained. The vaginal canal length is of 7 cm, and the genital hiatus is of 2.5 cm. Intercourse and penetration are possible, however, the FSFI questionnaire score is 20.4, indicating sexual dysfunction. Also, the patient still complains about pain during intercourse.
Conclusion: The Davydov procedure is one of the surgical approaches for the creation of a neovagina in cases presenting with MRKH. Neovaginal patency can be reached if a dilator is routinely applied post- operatively. A holistic approach to sexual function after the procedure, particularly the pain aspect, is mandatory for further research.
Two cases of ureteral duplication diagnosed during robot-assisted total laparoscopic hysterectomy
- Takayuki Okada1, Masaaki Andou1, Shintaro Sakate1 Kurashiki Medical Center, Japan
Objective: The incidence of ureteral injury during total laparoscopic hysterectomy was reported to be approximately 0.35%, and anatomical variations in the ureter are a risk factor for ureteral injury. To prevent ureteral injury, understanding the anatomy around the cardinal ligament and identification of the ureters are fundamental. We report two cases of ureteral duplication that were incidentally diagnosed during robot-assisted total laparoscopic hysterectomy.
Case 1: Case 1: A 53-year-old woman (gravida 2, para 1) presented with menorrhagia and anaemia associated with adenomyosis. A robot-assisted total laparoscopic hysterectomy was scheduled. While dissecting the retroperitoneal space and tracing the course of the ureter, the duplex ureters were identified on both sides, leading to a diagnosis of bilateral ureteral duplication. The operative time was 57 min, and the intraoperative blood loss was minimal.
Case 2: A 44-year-old woman (gravida 2, para 2) had uterine fibroid and adenomyosis. Robot- assisted total laparoscopic hysterectomy was planned. Fibrosis and adhesions associated with endometriosis were found around the left ureter. After the uterine artery was isolated and the left ureteral peristalsis was observed, a ductal structure with peristalsis was also observed on the caudal side of the left ureter. The operative time was 85 min, and the intraoperative blood loss was 100 g. In both cases, the surgery was completed without any ureteral injury.
Conclusion: In most cases, ureteral anatomical anomalies are not diagnosed preoperatively; therefore, confirmation of the ureteral anatomical orientation is crucial to prevent ureteral injury in minimally invasive hysterectomy. In gynecologic surgery, knowledge of the pelvic anatomy, including anatomical variants, is important to prevent complications.
Laparoscopic Salpingectomy in Ruptured Ectopic Pregnancy: A Case Report.
- Suganda A1, Susilo S1
Obstetrics and Gynecology Department Mitra Plumbon Hospital Cirebon Objective: To understand the safety and effectiveness of laparoscopic salpingectomy management of ruptured ectopic pregnancy.
Case: Patient 30 years old came to the emergency room with acute abdominal pain. At clinical examination the blood pressure was 80 mm Hg, palpation revealed a slinger pain. A pregnancy test was positive. The diagnosis of ruptured ectopic pregnancy was established. Thirty minutes later, patient went to operating theatre, a laparoscopic procedure was performed.
Results: At laparoscopic view, a haemato-peritoneum was found inside the abdominal cavity. During the exploration, a ruptured ectopic pregnancy was found in the right ampullary part of the tube. A right salpingectomy was performed, the active bleeding was treated, and blood clots were removed. The Hb level before operation was 11 g/dl, during surgery, two units of packed cells were given. Patient was discharged 1 day after surgery, with VAS 2 and Hb level 9 g/dl.
Conclusion: Laparoscopic salpingectomy can be safely and effectively utilized even in cases of ruptured ectopic pregnancy provided the anaesthetic team is comfortable with the procedure.
Safety and Feasibility of Total Laparoscopic Retrograde Hysterectomy (TLreH) In Patients with Frozen Pelvic Due to Severe Endometriosis.
- Adhitya Yudha Maulana1, Luky Satria Marwali2
1 Obstetrics and Gynecology Resident in Faculty of Medicine, University of Indonesia
2 Reproductive Endocrinology Fertility – Obstetrics and Gynecology Department, Fatmawati National Hospital Background: Surgical treatment of severe endometriosis is often challenging. This surgery often requires hysterectomy as a definitive treatment. Most of hysterectomies can be performed laparoscopically in general way but in some cases complicated by frozen pelvic conditions due to severe endometriosis, it needs another technique such as retrograde hysterectomy. There exists no study in Indonesia that reports the safety and feasibility of total laparoscopic retrograde hysterectomy (TLreH) in patients with frozen pelvic due to severe endometriosis.
Objective: To examine the safety and feasibility of total laparoscopic retrograde hysterectomy (TLreH) in patients with obliterated cul-de-sac due to severe endometriosis.
Methods: This retrospective observational study was performed at the Fatmawati National Hospital between January 2020 and Februari 2023. Seventeen women who underwent TLreH and who had uterine fibroids, adenomyosis, or both, complicated by frozen pelvic due to severe endometriosis were enrolled.
Results: Surgical outcomes were retrospectively analysed. The median operation time was 240 min (range, 165-390) and the median blood loss was 125 mL (range, 80-500). There were no cases of conversion to open surgery. Intraoperative complication occurred in two cases; both were lacerations of the rectum serosa. The median post operative pain was VAS 2. Post operative blood transfusion was required in two cases, both did get only 250 ml PRC transfusion. Post operative complication occurred in one case (ureterovaginal fistula). The median post operative length of stay was 4 days.
Conclusion: Our study demonstrated that TLreH for severe endometriosis with frozen pelvic was feasible and safe.
A Five-Year Trend and Experience of Laparoscopic Bilateral Tubal Sterilization using Falope Rings in a Single Centre at Sardjito Hospital, Yogyakarta, Indonesia
- Sarrah Ayuandari1, 3, Muhammad Nurhadi Rahman2, 3
1Division of Fertility and Reproductive Endocrinology, Department of Obstetrics and Gynecology, Faculty of Medicine, Public Health and Nursing, Universitas Gadjah Mada, Yogyakarta, Indonesia 2Division of Urogynaecology and Reconstruction, Department of Obstetrics and Gynecology, Faculty of Medicine, Public Health and Nursing, Universitas Gadjah Mada, Yogyakarta, Indonesia 3Obstetrics and Gynecology, Sardjito Hospital, Yogyakarta, Indonesia
Email: sarrah.ayuandari@ugm.ac.id Phone number: +6281263926116 Email: adirahman@ymail.com Phone number: +62811251200 Objective: Laparoscopic bilateral tubal sterilization using Falope rings is one of the most efficient yet effective procedure of permanent contraception. The demographic and geographic variety in Indonesia have provided certain challenges and uniqueness in each procedure, including in Yogyakarta province. The objective of this study was to depict the sociodemographic characteristics, techniques, and associated complications in the course of 5 years in a single centre.
Method: This study was a retrospective analysis of the laparoscopic bilateral tubal sterilization procedures using Falope rings which were conducted in Sardjito hospital over a five-year period from January 1st, 2018 until December 31st, 2022.
Results: A total of 1,040 laparoscopic bilateral tubal sterilization using a trans-umbilical trocar with Falope rings were performed in Sardjito Hospital over five years. It was shown a trend of increasing numbers of procedures over the time period, from 89 in 2018, 201 in 2019, 153 in 2020 (decreased due to Covid pandemic), 272 in 2021 and 325 procedures in 2022, which was three times higher than in 2018. The patients originally came from 6 regions in 2 provinces, Yogyakarta and Central Java. The average age of the patient was 38.7 4.7 years old. Patients with > 2 children were 50.2%, meanwhile 49.7% have equal and less than 2 children. It was observed that in the year of 2022, 96% of the procedures were successful without any complication and pregnancy, meanwhile 4% did fail (n= 12 out of 325) caused by severe adhesions due to the patients surgical history or pelvic inflammation, endometriotic cyst, severe obesity and acute hypertension of the patient. The patients with failed laparoscopic tubal sterilization were counselled to have another long term contraceptive methods (IUD or implant).
Conclusion: Laparoscopic tubal sterilization is associated with a low failure rate, low morbidity and therefore it is safe in women even with previous pelvic surgery. Due to the increasing trend in patient numbers who undergo this procedure, it is important for a single centre to improve the data collection and analysis, in order to upgrade the quality service and in doing so reduce the complication rate in the future.
Clinical outcomes of Laparoscopic assisted vaginal hysterectomy (LAVH) combined with Bilateral uterine artery ligation (BUAL) procedure.
- Jeong Soo Lee
Department of Obstetrics and Gynecology, Nowon Eulji Medical Center, Eulji University, South Korea.
Correspondence: Yong-Soon Kwon kbongchun73@naver.com Objective: To evaluate whether performing of bilateral uterine artery ligation (BUAL) is safe and effective during LAVH procedures and could reduce risks of transfusion, laparotomic conversion, and intraoperative injury in case of large sized uterus.
Methods: This was a retro prospective cohort study performed by a single surgeon Yong Soon Kwon in the Department of Obstetrics and Gynecology, Nowon Eulji Medical Center, Eulji University from April 2019 to September 2022, excluding patients with malignancy. A total of two hundred and five patients underwent the operation. Analytic parameters are operation time, uterus weight, total blood loss, before and after differences in haemoglobin level, hospital stay and intraoperative and postoperative complications.
Results: The mean age (year) of the patients were rounded up to 48.58 ± 5.29 years. Patients without adhesiolysis (85.7%) was mainstream compared to whom with adhesiolysis (24.3%). The percentage of pathologic diagnosis of leiomyoma and adenomyosis was similar. Patients with both were majority. Others including Endometrial hyperplasia, Cervical intraepithelial neoplasm was also detected in minority. The mean operation time was less than an hour, 55.96 ± 16.54 (minute). Total Estimated blood loss was 85.57 ± 89.96 (mL). Mean hospital stay was 4.37 ± 0.78 (day). The change between pre- and post-operation haemoglobin change wasn’t significant. The difference was less than 1g/dL. None of the patients included in this study was given intraoperative transfusion and there was no case of conversion to laparotomy. Longer operation time (71.38 ±23.71 (min)) contrary to LAVH without adhesiolysis (53.39 ± 13.49 (min)) (P=<0.001) was noted. Patients with adhesiolysis had greater total EBL. (149.31 ± 152.78 (mL) to 74.94 ± 69.69 (mL) P=0.015). Total hospital stay was a bit lengthened in patients with adhesiolysis compared to without (4.76 ± 1.09 (day) to 4.31 ± 0.7 (day) P=0.04).
Conclusion: It is safe and effective to perform LAVH under BUAL. Also, LAVH under BUAL prevented postoperative bleeding and could keep the stable recovery period after the operation. BUAL can make it possible safely to perform LAVH with a huge sized uterus.
Advanced Laparoscopic surgical technique for Focal Uterine Adenomyosis.
- Soojin Kim
Department of Obstetrics and Gynecology, Nowon Eulji Medical Center, Eulji University, South Korea.
Correspondence: Jae Young Kwack podogazi@naver.com Objective: We evaluated the efficacy and outcomes of the new advanced laparoscopic adenomyosis resection with the wedge resection technique in focal uterine adenomyosis and introduce the new surgical technique.
Methods: From February 2019 to February 2020, 49 patients who received a t adenomyosis resection by the new surgical technique were enrolled in the study. The inclusion criteria were the presence of focal-type adenomyosis diagnosed by ultrasonography or magnetic resonance image (MRI) that was refractory to medical treatments and patients with a strong desire to preserve their uterus. All operations were performed by a single surgeon with a uniform technique under TOUA (Transient Occlusion of both Uterine Arteries).
Results: The mean patient age was 40.53 ± 5.93 years. The mean ± SD diameter of the adenomyoma lesions was 4.57 ± 1.21 cm, and the mean weight of the excised lesions was 40.53 ± 35.65 g (range, 15 – 209 g). The mean total operation time was 70.11 ± 15.05 minutes. The mean estimated blood loss was 88.88 ± 20.0 mL (20 – 500 ml) and there was no injury to the adjacent organs or pelvic nerves. No patient received an intraoperative transfusion. Conversion to laparotomy or major complications requiring reoperation was not occurred. At the 7-month follow-up, the main symptoms, including dysmenorrhea and menorrhagia improved. Complete remission of dysmenorrhea and menorrhagia occurred in 97.4% and 88.9% of the patients, respectively.
Conclusion: Laparoscopic adenomyomectomy using the wedge resection technique could be a safe and effective alternative technique in patents with focal uterine adenomyosis. The surgical indication could be widened and heavy lesion could be included performing wedge laparoscopic resection adenomyomectomy.
Laparoscopic Removal of Intra-Abdominal Mislocated Intrauterine Devices: Case Series.
- Damayanti Eka Fransiska Malau, Yusuf Effendi, Heriyadi Manan
Fertility, Endocrinology, Reproductive Division of Dr. Mohammad Hoesin General Hospital, Faculty of Medicine Sriwijaya University, Indonesia Objective: Intrauterine devices (IUDs) are a widely preferred method of contraception due to their effectiveness and safety. However, the use of IUD is also associated with side effects and complications. Uterine perforation is an uncommon complication with an incidence of 1 in 1,000 insertions. IUD perforation can involve adjacent organs (i.e., intestine and bladder) leading to tissue destruction and peritonitis. This paper aims to report cases of intra-abdominal mislocated intrauterine devices.
Methods: We conducted a case series study consisting of four cases of mislocated IUDs caused by complete uterine perforation at the Mohammad Hoesin General Hospital from February 2022 until February 2023.
Results: Patients came with pain in the lower abdomen, and a history of IUD insertion. Upon evaluation using transvaginal ultrasound, X-Ray, and CT-Scan, all four patients were found to have intra- abdominal mislocated IUDs. In three cases, devices were found in the peritoneal cavity, enveloped by omentum. In one other case the device had perforated the sigmoid colon. In all four patients, devices were removed using laparoscopic surgery, with minimal complications after surgery.
Conclusion: Intra-abdominal mislocated IUDs the devices can generally be removed successfully using laparoscopic surgery.
A Laparoscopic Salpingo-oophorectomy and Natural Orifice Specimen Extraction (NOSE)-colectomy: in a case of Suspected Colorectal Deep Infiltrating Endometriosis.
- Rilla Saeliputri1, Herbert Situmorang2
1.Department of Obstetrics and Gynecology, Cipto Mangunkusumo National Referral Hospital – Universitas Indonesia
2.Reproductive Health Division, Department of Obstetrics and Gynecology, Cipto Mangunkusumo National Referral Hospital – Universitas Indonesia Objective: To present an experience of laparoscopic salpingo-oophorectomy continued with the natural orifice specimen extraction (NOSE) technique for segmental bowel resection in patients with suspected colorectal endometriosis.
Methods: A case of a woman with complaint of a sudden twisting in the lower left abdomen, the complaint was not affected by pressure or a change in position. Difficult defecation and farting, with a history of menstrual pain arising especially for three months before admission. Contrast abdominal CT scan was performed showing a narrowing of the colorectal segment. Laparoscopically, a lesion was found on the colorectal segment suspected to be a deep infiltrating endometriosis nodule adherend to the left ovary. The operation continued with as salpingo-oophorectomy and a segmental colorectal resection.
Results: The specimen was then delivered through a natural orifice (rectum) to provide a minimal post operative pain, improved cosmesis, lowered risk of incisional hernia, shorter recovery and less analgesia required compared to mini-laparotomy for specimen extraction. The anatomic relationship with the rectum, has the advantage to access the abdominal cavity through the latter for specimen extraction in case of resection of a colorectal endometriosis nodule.
Conclusion: Laparoscopic salpingo-oophorectomy continued by Natural Orifice Specimen Extraction (NOSE)-colectomy for a case of suspected colorectal deep infiltrating endometriosis has several advantages compared to mini-laparotomy. The approach of natural orifice specimen extraction might be a next step in the evolution of minimally invasive surgery.
Characteristics of patients undergoing laparoscopic supracervical hysterectomy procedure at Bali Royal Hospital Denpasar in 2020-2022.
- IB Putra Adnyana1, IB Praja Putra Adnyana2, Olivia L Prawoto3, Hartanto3, Aldo Alberto Lawu3, Seyla Kresentia3
1 Division of Endocrine Reproductive Fertility, Department of Obstetrics and Gynecology, Faculty of Medicine, Udayana University-Prof. Dr. dr. I.G.N.G. Ngoerah General Hospital, Denpasar Bali
2 Department of Obstetrics and Gynecology, Bali Royal Hospital (BROS), Denpasar Bali
3 Department of Obstetrics and Gynecology, Faculty of Medicine, Udayana University – Prof. Dr. dr. I.G.N.G. Ngoerah General Hospital, Denpasar Bali Introduction: Laparoscopic Assisted Supracervical Hysterectomy (LASH) is a type of hysterectomy that is widely performed worldwide and has a relatively low rate of postoperative complications, less bleeding, shorter length of stay, and faster postoperative recovery.
Methods: This study is a descriptive study that includes women who underwent laparoscopic hysterectomy procedures at Bali Royal Hospital, Denpasar, Bali during the period of 2020-2022.
Results: In this study, 44 research subjects were obtained with the majority residing in Denpasar (35 subjects, 79.55%). The majority of patients were under the age of 35 (38.64%) with an average age of 36.6 ± 5.6 years. Patients with a history of one childbirth 29 subjects (65.91%), 2 children for 14 subjects (31.82%), and patients who had never given birth were 8 subjects (18.18%). Based on the body mass index (BMI), the average BMI of patients was 24.2 ± 2.1 with the majority in the BMI range of 18.5-24.9 for 25 subjects (56.82%). The most common preoperative diagnosis was adenomyosis for 22 people (50%), followed by uterine fibroids (13 subjects, 29.55%), abnormal uterine bleeding for (8 subjects, 18.18%), and endometrioma for (1 subjects, 2.27%). The majority of patients (72.73%) did not have any complications during the procedure, but 10 subjects (22.73%) were found to have adhesions. The duration of the operation procedure was 150-200 minutes for 17 subjects (38.64%) with an average of 200 minutes. Bleeding that occurred in 8 subjects (18.18%) was 100 cc, in 20 subjects (45.45%) 150 cc, 14 subjects (31.82%) lost 200 cc, and 2 subjects (4.55%) 250cc. All subjects (100%) were hospitalized for 2 days and none received intensive care.
Conclusion: LASH in patients with benign gynecological tumours is a relatively easy procedure with few postoperative complications.
Laparoscopic Resection of Cesarean Scar Ectopic Pregnancy
- Jose Tymothy Manuputty 1, Yuli Trisetiyono 2
1Resident of Obstetrics and Gynecology Department, Faculty of Medicine, Diponegoro University, Kariadi General Hospital, Semarang, Indonesia
2 Staff Consultant of Fertility and Endocrinology Division, Department of Obstetrics and Gynecology, Faculty of Medicine, Diponegoro University, Kariadi General Hospital, Semarang, Indonesia. Introduction: A 30-year-old with a history of Cesarean section in two previous pregnancies, diagnosed with an 11-week-old pregnancy and presented with a heavy vaginal bleeding. Examination results conclude a diagnosis of blighted ovum. Curettage was done but the gestational sac couldn’t be taken out. Ultrasonography results show the pregnancy mass to be implanted at the level of the cesarean scar on the uterine isthmus. The mass dimensions are quite big 4x3x2 cm with active vascularization and a serum level of hCG 2123 mIU/mL. The patient underwent a laparoscopic resection.
Surgical technique: A uterine manipulator was installed first to facilitate the dissection. A three centimeters incision was made below the umbilicus to insert the primary trocar. Three other incisions were made to insert 3 three secondary trocars. Insufflation was done with CO2 gas. An exploration of the abdomen and the pelvic cavity was performed, the broad ligament was opened and the right and left uterine arteries were ligated by Endo clips with the help of uterine manipulation. Infiltration of the pregnancy mass was done by injecting vasopressin to minimize bleeding from the uterus. The vesico-uterine space was opened and set aside to find the isthmus. The pregnancy mass was resected from the isthmus by using a harmonic scalpel. The surgery time was 101 minutes with a bleeding of approximately 50 cc. The isthmus was sutured by v-lock and the vesicouterine space with Monosyn 1 suture. The pregnancy mass was removed through the primary trocar with an endobag. The abdominal cavity was deflated. The trocar incision was sutured layer by layer.
Conclusion: The laparoscopic approach with excision and repair of the uterine wall represents a safe and efficient therapeutic option for the treatment of the Cesarean scar ectopic pregnancy.
Laparoscopic Caesarean Scar Niche Repair: A Case Report
- Rustham Basyar1, Moh. Aerul Chakra1,2
1.Fertility, Endocrinology and Reproductive Division Faculty of Medicine Sriwijaya University, Indonesia.
2.Blastula IVF Clinic, Siloam Sriwijaya Hospital Palembang, Indonesia. Objective: The incidence rate of Cesarean section (CS) has continued to rise, and has led to many complications. One of the complication is niche, a defect in the CS scar. The niche may be associated with abnormal bleeding. During the next pregnancy, it can cause scar dehiscence, uterine rupture, and an abnormal adherent placenta. Several therapies can be used to treat symptoms related to the niche, such as hysteroscopic niche resection, laparoscopic repair, and vaginal repair. This paper aim to reported niche case managed by laparoscopic resection.
Methods: We performed a laparoscopic procedure to repair the CS niche, at Blastula IVF Clinic, Siloam Sriwijaya Hospital Palembang.
Results: A 32 years old women, P2A0, came to our clinic with as main complaint abnormal bleeding. Patient has a history of two CS. The bleeding complaint did appear after the second CS. We found the niche at CS scar when we explored the patient. Then we performed the niche resection by laparoscopy with no complication after procedure.
Conclusion: In case of niche CS scar, defect can generally be repaired successfully.
Complications of Gynecological Laparoscopic Surgeries In Dr. Mohammad Hoesin General Hospital from 2021 to 2022
- Aripin Syarifudin, Yusuf Effendi, Rizani Amran
Fertility, Endocrinology, Reproductive Division of Dr. Mohammad Hoesin General Hospital, Faculty of Medicine Sriwijaya University, Indonesia. Objective: Laparoscopy has now become one of the minimally invasive surgeries which is an excellent technique that is increasingly routinely performed in hospitals. Magrina, 2002, stated that in 1,549,360 patients who underwent laparoscopy, the incidence of complications ranged from 0.2 to 10.3%. This study reviews the complications that occur in gynaecological laparoscopic surgeries performed in dr. Mohammad Hoesin General Hospital, Palembang in the period 2021 to 2022.
Methods: We conducted a descriptive retrospective study in Mohammad Hoesin General Hospital from January 2021 until December 2022.
Results: During the period from January 2021 to December 2022, 739 gynecological laparoscopic surgeries were performed at the Mohammad Hoesin General Hospital, with a total of nine patients experiencing complications, six of which were trocar site hematomas, two patients had subcutaneous emphysema, and one patient had a posterior uterine perforation.
Conclusion: Complications of gynecological laparoscopic surgery can occur starting from trocar entry over intra-operative to post-operative. The incidence of laparoscopy in Mohammad Hoesin General Hospital is 1.21%. Although the incidence of laparoscopic complications is rare, it still requires the expertise of the operator and the team to recognize these early and treat promptly and appropriately.
A rare case: Idiopathic utero-colon fistula in 50 years old patient and what superior modalities to perform a diagnosis
- Adiguna Wibawa1 Eppy Darmadi Achmad1
1 Obstetric and Gynecologic Department, Hasan Sadikin Hospital, Padjadjaran University, Bandung, Indonesia.
Correspondence: adiguna.gurnita@gmail.com Tel: +6282118670482 Objectives: A utero-colon fistula is a rare condition, in this case causes are idiopathic. This case will review and evaluate how diagnosis was made and highlights the role of the healthcare team in managing patients with this condition.
Methods: This is a case report on a 50-year-old woman with a suspected utero-colon fistula who presented with passing stools from the vagina each time she defecated. Physical examination, fistulograhpy, abdominal CT scan was performed but did not reveal the diagnosis with certainty, diagnostic laparoscopy and hysteroscopy were conducted to confirm the diagnosis.
Results: Physical examination revealed no abdominal tenderness. Feces were coming out from the vagina. Fistulography from anal to rectum does not show a clearly visible track / fistula associated with the vagina, Abdominal CT showed multiple fistulas from rectum to vagina and suspected a uterus didelphys. A diagnostic Laparoscopy and hysteroscopy were performed and revealed severe adhesions between the sigmoid colon and the right posterior fundus of uterus, the fistula was found on hysteroscopy and it connected the right posterior part of the fundus to the sigmoid colon.
Conclusion: In cases of utero-colon fistula, despite good imaging modalities, the diagnosis remains challenging. Operative diagnostic procedures (hysteroscopy and laparoscopy) can be superior modalities for diagnosis and management
Laparoscopic Repair of Symptomatic Isthmocele Patients: Case Series.
- Herbert Situmorang1, Yuri Feharsal1, Dewita Nilasari1
1Department of Obstetrics and Gynecology, Faculty of Medicine, Universitas Indonesia Correspondence: Dewita Nilasari E-mail : dewita.nilasari@gmail.com Objective: Isthmocele is a common complication after Cesarean section. This condition can result in abnormal uterine bleeding and infertility. Meanwhile, laparoscopic repair of Isthmocele is a minimally invasive technique that has shown promising results in improving clinical outcomes. Herein, we present two patients of laparoscopic repair of isthmocele who presented with abnormal uterine bleeding.
Methods: The first case is a 27-year-old female with a history of Cesarean section who presented with abnormal uterine bleeding. Transvaginal ultrasound revealed an isthmocele with residual myometrial thickness of 0.11 cm, and laparoscopic repair was performed using a two-layered closure technique. The patient was discharged in three days and reported significant improvement of her symptoms at the first-week follow-up visit. Repeated ultrasound showed complete resolution of the isthmocele within one-month.
The second case is a 27-year-old female who presented with repeated heavy menstrual bleeding following a Cesarean section four-months prior. Isthmocele was identified using both transvaginal ultrasound and hysteroscopy. Transvaginal ultrasound showed a residual myometrial thickness of 0.14 cm and hysteroscopy revealed arterial bleeding through the lesion. Laparoscopic repair was performed using a similar technique to the first case. Similarly, patient’s symptoms were resolved at the scheduled follow-up visits and ultrasound examinations showed complete healing of the isthmocele.
Conclusion: laparoscopic repair of isthmocele is a safe and effective treatment option for patients with abnormal uterine bleeding and a history of Cesarean section. Laparoscopy is a technique that has to be preferred especially if the residual myometrial thickness is <3 mm. It can improve the clinical symptoms among affected women, with minimal morbidity and short hospital stays. Further studies are needed to evaluate the long-term outcomes and cost-effectiveness of this approach in comparison to other modalities.
Apical Suspension at Time of Total Laparoscopic Hysterectomy – Should It Be Done? Introducing The REATTACH Study – RCT
- Inge Putri
Objective: To evaluate the effect of prophylactic uterosacral suspension at time of laparoscopic hysterectomy on reducing the risk of developing prolapse in the future.1
Methods: Primary outcomes: This will be the quantitative point C that will be recorded prior to surgery, immediately post-surgery, and at 6 and 12 months. The relevant change in point C post uterosacral suspension will be measured at each time point. A clinician blinded to the intervention will be performing all the postoperative assessments.
Secondary outcomes: This will be the length of operative time, as well as ascertaining the presence of complications such as rates of urinary retention, urinary tract infection, bladder injury, paraesthesia, changes to sexual function such as dyspareunia. A subjective assessment will also be completed through completion of the PISQ-12 score, as well as the PFDI-20 score. The pre operative and post operative scores will be compared.
Data collection: The project will be conducted at a tertiary single center through a randomised controlled trial with 2 arms of intervention and control. Intervention arm: patient will undergo high uterosacral suspension at time of total laparoscopic hysterectomy in addition to the routine 2-layer vault closure. Control arm: patients will undergo routine 2-layer vault closure incorporating the uterosacral ligaments. The number of patients needed to be recruited in each arm was calculated to be 33.
Conclusion: Post hysterectomy vault prolapse is a common issue for women and remain a challenging problem for the pelvic reconstructive surgeons. Given the morbidity and cost involved for surgical repair, we need to focus on the prevention of this condition.
References:
- Alperin M, Weinstein M, Kivnick S, Duong TH, Menefee S. A randomized trial of prophylactic uterosacral ligament suspension at the time of hysterectomy for Prevention of Vaginal Vault Prolapse (PULS): design and methods. Contemp Clin Trials. 2013;35(2):8-
- doi:10.1016/j.cct.2013.04.001
- O’ Neill A, Cario GM, Rosen D, Chou D, Laparoscopic Uterosacral Ligament Suspension (LUSLS): Its Role in the Prevention of Post Hysterectomy Vault Prolapse, Journal of Minimally Invasive Gynaecology, Volume 16, Issue 6, Supplement, 2009, Page S27, ISSN 1553-4650, https://doi.org/10.1016/j.jmig.2009.08.102.
- Abbott, J. A., Bajzak, K. I., Green, I. C., Jacobs, V. R., Johnson, N. P., Lieng, M., Munro, M.
- G., Singh, S., Sokol, E. R., Sokol, I., Kho, R., Margulies, R. U., Rardin, C. R., & Sokol, E. R. (2014). AAGL Practice Report: Practice Guidelines on the Prevention of Apical Prolapse at the Time of Benign Hysterectomy. Journal of Minimally Invasive Gynaecology, 21(5), 715- 722. https://doi.org/10.1016/j.jmig.2014.04.001
Section 2 | Vaginal Surgery
Vaginal Natural Orifice Transluminal Endoscopic Surgery(vNOTES) using a double balloon catheter for large benign ovarian cyst
- Yurina Shimomura2023 Bali 1, Shiori YANAI1, Masaaki ANDOU1 1Kurashiki Medical Center, Japan
Objective: vNOTES is one of the least invasive and cosmetically advantageous techniques for gynecologic tumours. However, with huge ovarian tumours, there is an intrinsic difficulty in maintaining the operative field as well as the question of how to retrieve the tumour. We experienced one case in which a huge ovarian cystic tumour was retrieved easily using a double balloon catheter.
Methods: The patient was a 67-year-old G 2 P 2 woman with a BMI of 29.0. The tumour was found during a regular check-up. MRI revealed a bilocular cystic tumour measuring φ13.6×13.8×9.9cm. Tumour markers such as CA19-9、CA125 and HE4 were not increased so we decided to perform a bilateral salpingo-oophorectomy with the aid of vNOTES.
Results: The tumour was located outside the pelvis due to its size. First, the adnexal ligament was desiccated and divided and then the left ureter was identified. The left Infundibulo Pelvic ligament was desiccated and divided. Although the supporting ligaments were all divided, the tumour was too big to descend to the pelvis. As a result, the tumour was carried into a protection bag in the upper abdomen. The isolation bag was introduced into the vagina and the tumour content was aspirated using a double balloon catheter.
Conclusion: Huge ovarian cysts are difficult to retrieve when performing vNOTES. One problem is the maintenance of the operative field and another problem is the spillage of tumour cells in the abdominal cavity. In this case we were able to solve these problems with minimally spillage using a double balloon catheter and a protection bag. This is one of the techniques that can be applied for cases of large ovarian tumours where a cosmetically friendly minimally invasive procedure is desired.
Section 3 | General Gynaecology
The relationship between lifestyle (Physical Activity, Anxiety, Dietary Diversity) and nutritional status with menstrual patterns of students at SMAN 3 Bandung before and during the COVID-19 pandemic.
- Anggun Cempaka Wulandari¹, Tita Husnitawati Madjid², Yenni Zuhairini³
¹Bachelor of Medicine, Padjadjaran University, Indonesia
²Obstetrics and Gynaecology Department, School of Medicine, Padjadjaran University, Indonesia
³Public Health Sciences Department, School of Medicine, Padjadjaran University, Indonesia Introduction: Menstruation is an important indicator in determining the health and fertility status of the female reproductive system, which is regulated by the hypothalamic-pituitary-ovarian axis. The COVID-19 pandemic has an impact on lifestyle, including physical activity, level of anxiety, dietary diversity, nutritional status, and weight changes. Changes in lifestyle and nutritional status have caused disruptions in menstrual patterns, including frequency, duration, regularity, intermenstrual bleeding, blood volume, and menstrual pain. This condition also occurs in female students at SMAN 3 Bandung who are using the Remote Learning System (PJJ).
Purpose: The purpose of this research is to determine the description and the relationship between physical activity, level of anxiety, dietary diversity, nutritional status, and menstrual patterns of students at SMAN 3 Bandung during the COVID-19 pandemic, which can provide information about changes in lifestyle towards menstrual patterns, eating patterns, and stress occurrences, thus will increase knowledge and awareness in preparing oneself in case of pandemic conditions in the future.
Method: This is a descriptive analytical comparative study with a cross-sectional approach to 143 out of 185 students from SMAN 3 Bandung who met the inclusion and exclusion criteria. Physical activity data was collected using the IPAQ (International Physical Activity Questionnaire); anxiety level data was collected using the DASS 42 (Depression Anxiety Stress Scale); dietary diversity data was collected using the DDS (Dietary Diversity Score); menstrual data was collected using guidelines from the FIGO (International Federation of Gynecology and Obstetrics) 2018. Menstrual pain was classified according to Speroff’s Clinical Gynecologic Endocrinology and Infertility, 9th edition, mild pain is defined as felt for +/- three days 3, while severe pain is defined as felt for >4 days and unable to be reduced by changing positions. Respondents were asked to fill out the questionnaires and had their weight and height measured to calculate Body Mass Index.
Results: No significant difference was found in the number of female students in aspects of physical activity, stress, dietary diversity, and menstrual patterns before and during the COVID-19 pandemic. No significant correlation was found between nutritional status and menstrual patterns during the COVID-19 pandemic. No significant correlation was found between changes in lifestyle in terms of physical activity and stress, and changes in body weight, with changes in menstrual patterns before and during the COVID-19 pandemic. A significant correlation (p = 0.074) was found between changes in lifestyle in terms of dietary diversity and changes in menstrual patterns before and during the COVID-19 pandemic among female students at SMAN 3 Bandung.
Conclusion: A significant correlation was found between changes in lifestyle in terms of dietary diversity and changes in menstrual patterns among female students at SMAN 3 Bandung before and during the COVID-19 pandemic. Female students with increased dietary diversity tend to have improved menstrual patterns, while those with decreased dietary diversity tend to have worsened menstrual patterns. It is suggested to conduct further research on menstrual patterns with other variables. In addition, for an individual, it is suggested to regularly check reproductive health and maintain a healthy lifestyle during the COVID-19 pandemic.
A Systematic Review and Meta-Analysis of Delivery Outcome, Adverse Maternal, and Neonatal Outcomes and in Patients with Endometriosis.
- I Wayan Agus Surya Pradnyana1, I Gde Sastra Winata2, I Gusti Bagus Mulia Agung Pradnyaandara1
1Bachelor of Medicine, Faculty of Medicine, Udayana University, Denpasar, Bali, Indonesia
2 Gynecologic Oncology Division, Department of Obstetrics and Gynaecology Faculty of Medicine, Udayana University, Denpasar, Bali, Indonesia. Objective: One of the most common gynecological disorders is endometriosis. However, delivery and adverse maternal and neonatal outcomes remain understudied. This study aimed to assess the effect of endometriosis on pregnancy and neonatal outcomes.
Methods: A systematic search was performed in PubMed, ScienceDirect, and Cochrane using MeSH terms if applicable and in accordance with the PRISMA guidelines, to determine the effects of endometriosis on delivery outcomes which is caesarean delivery (CD), instrumental delivery (ID), and also adverse maternal which was post-partum haemorrhage (PPH) and neonatal outcomes. The Newcastle–Ottawa scale (NOS) was used to assess the risk of bias in this analysis and Review Manager 5.4 to calculate the result of 95% CI for the outcomes.
Results: A total of 25 studies with 4,243,447 patients were included. Pooled analysis showed patients with endometriosis was associated with an increased rate of CD (OR 1.80, 95% CI 1.20-2.70), increased rate of PPH (OR 1.69, 95% CI 1.28-2.22), increased rate of ID (OR 1.33, 95% CI 1.24-1.43). But interestingly patients with deep endometriosis were significantly more associated with PPH (OR 1.91, 95%CI 1.03-3.54) rather than CD (OR 1.20, 95%CI 0.72-2.02). Patients with endometriosis also significantly associated with premature birth (OR 1.62, 95%CI 1.38–1.90) and lower birthweight (SMD 0.23, 95%CI 0.08-0.38).
Conclusion: Overall, this study suggests that endometriosis is a significant risk factor for pregnant patients who will come to delivery and may be associated with higher rate of PPH, CD, ID. Pregnant patients with endometriosis may also have premature delivery and low birthweight babies. Since the number of patients with matched baseline characteristics study was still limited, further investigation is still needed to confirm the study results.
Fetoscopic Laser Photocoagulation in Twin-to-Twin Transfusion Syndrome (TTTS) at Harapan Kita Women and Children Hospital, Jakarta.
- Irvan Adenin1,2, Gatot Abdurrazak1,3, Sadina Pramuktini1,4
1Maternal-Fetal Medicine Department, Obstetrics and Gynecology, Harapan Kita Women and Children Hospital, Jakarta, Indonesia
2Correspondence: irv.adenin@gmail.com (+628121041370) Introduction: This study aims to investigate the survival rate of TTTS in Harapan Kita Women and Children Hospital, Jakarta after fetoscopic laser photocoagulation and to compare the survival rate between low and high Quintero staging.
Methods: All of TTTS cases in the gestational age of 18 to 26 weeks treated with fetoscopic laser photocoagulation in Harapan Kita Women and Children Hospital, Jakarta from the period of 2015 to 2020 were included to this study. The survival rate of fetoscopic laser photocoagulation was measured by perinatal survival; whether one or both twins survived or demised. Samples were classified based on low Quintero stages (II) and high Quintero stages (III and IV) to compare the effect of early to late referral in the outcome of TTTS.
Results: Among 86 TTTS cases in the 5-year period, the survival rate of at least one twin was 36,05%, both twins were 72,09%, and both fetal demises were 27,91%. Survival rate in one twin and both twin with the low Quintero stages were 80,05% and 58,3, respectively. In the higher Quintero stage group, the survival rate was 66% of at least one twin and 20% of both twins. The result was statistically significant between low and high Quintero stages (p=0,001) in survival of both twins and no significant difference of at least one twin survival (p=0,153).
Conclusion: Fetoscopic laser photocoagulation increase survival rate in TTTS patients. Low Quintero stages (stage II) showed higher significant survival rate of both twins compared to higher Quintero stages (stage III and IV).
Comparative clinical outcome following individualized follitropin alfa and follitropin delta in women undergoing ovarian stimulation for in vitro fertilization
- Mona Galatia1, Yuli Trisetiyono1
Department of Obstetrics and Gynecology, Faculty of Medicine Diponegoro University Kariadi General Hospital, Semarang, Central Java, Indonesia
Correspondence: galatiamona@gmail.com ; phone number : +6281223374647) Introduction: Current clinical practice of infertility treatment is moving from standardized to individualized FSH dosing, as new FSH preparations integrate individualized dosing as part of the clinical development. Among the most used regimens, are those using recombinant FSH associated with human menopausal gonadotropin. The aim of this study was to investigate the impact of follitropin delta and follitropin alfa for ovarian stimulation on embryo development and quality in in vitro fertilization cycles.
Methods: This study uses an analytic observational study with a cross sectional approach to analyze the impact of follitropin delta and follitropin alfa for ovarian stimulation on embryo development and quality in in vitro fertilization cycles who were treated at RSUP Dr. Kariadi Semarang during January 2022 to January 2023. All cycles involved controlled ovarian stimulation using recombinant FSH with gonadotropin-releasing hormone (GnRH) antagonist, long GnRH agonist, or flare GnRH agonist protocols. Inclusion criteria were 16 patient who want to have IVF cycles treated in a fertility clinic, completed laboratory examinations, and subjects would be excluded if not meeting the inclusion criteria. p value <0.05 considered significant.
Results: Total subjects n=16 women; 12 subjects to follitropin alfa and 4 subjects to follitropin delta. The mean value of body weight all subjects was 62,75 ± 8,84 according to each patient’s initial AMH level (1,50 ± 1,15). The age mostly less than 35 years (43.8%) subjects. Most of the indications for IVF is endometriosis (43,8%). Mean duration of stimulation was 8,00 ± 3,14. Total dosage of recombinant FSH in follitropin alfa were 1908,83 ± 867,97 while in follitropin delta were 1050,45 ± 857,23; P= 0,108. Mean oestradiol level follitropin alfa and delta (1965,60 ± 836,57 vs 1766,6 ± 1156,27) and progesterone 2,11 ± 2,41 vs 6,38 ± 10,85. When analysing the pregnancy rate follitropin alfa and delta were 2 (66,7%) vs 1 (33,3%); P= 0.607, higher on the follitropin alfa but it was not statistically significant. Treatment with follitropin alfa and follitropin delta gave different outcomes for mean number of oocytes retrieved (5,50 ± 1,93 vs 11,75 ± 4,99; P= 0,002), and different average number of embryos development (1,83 ± 0,72 vs 2,50 ± 0,58; P= 0,114). An assessment of the follitropin delta in this trial show a higher number of oocytes and embryo development. This result slightly different from the ESTHER-1 trial showed follitropin delta, with fewer excessive stimulation responses and fewer measures taken to prevent ovarian hyperstimulation syndrome.
Conclusion: Our findings contribute to the evidence on follitropin delta which resulted in more oocytes and embryo development in follitropin delta. This trial showed that follitropin delta is not inferior to follitropin alfa, and can be a choice for ovarian stimulation for in vitro fertilization.
Comparison of Ant-Müllerian Hormone (AMH) levels among stripping and partial excision cystectomy in endometrioma patients
- Ida Bagus Putra Adnyana1, Ni Luh Wita Astari Widhusadi2, I Nyoman Ardi Widiatmika2, Alit Darma Asmara2
1Fertility, Endocrinology and Reproduction Division, Department of Obstetrics and Gynecology, Prof. dr. I.G.N.G Ngoerah Denpasar General Hospital Denpasar and Bali Royal Hospital, Denpasar, Bali, Indonesia
2Resident of Department of Obstetrics and Gynecology, Faculty of Medicine, Udayana University Prof. dr. I.G.N.G Ngoerah Denpasar General Hospital Denpasar, Bali, Indonesia Introduction: Endometrioma is associated with the most advanced stages of endometriosis. Laparoscopic cystectomy usually be the treatment of choice for endometrioma. The optimal treatment for endometrioma patients who desire fertility remains unknown. There are partial and stripping excision of the endometriotic cyst. Impaired ovarian function after surgery can be evaluated by measuring the ovarian reserve. Anti-Mullerian Hormone (AMH) is the only reliable ovarian reserve marker. This study was to compare the effect on AMH levels in endometrioma patients who underwent partial and stripping excision laparoscopic cystectomy.
Materials and Methods: This prospective analytic study with pre- and post- designs measured the changes of AMH levels on endometrioma patients before surgery, one month and three months after surgery between patients with partial and stripping excision group. The study was conducted at Bali Royal Hospital, Bali from January 2020 to December 2022. Independent Samples t-Test was used to analyse the significant differences.
Results: A total of 126 patients were included in this study and divided into two groups (partial and stripping excision cystectomy) and the site of endometriosis with mean of age 34.42 ± 7.07 years old. There was a significant difference on AMH levels between patients with partial excision and stripping excision on one month (1.36 ± 0.34 vs 0.91 ± 0.33) and three months (1.73 ± 0.45 vs 1.24 ± 0.36) after surgery (p<0.000 and p<0.000).
CONCLUSION: Partial excision cystectomy has lower effect on AMH levels than stripping excision cystectomy in endometrioma patient.
Using PAX1 and JAM3 gene methylation detection as a triage tool for cervical cancer screening in women: an analysis of a single-center prospective study. in China
- Huafeng SHOU1, Xiaojing WANG1, Linhua ZHOU1, Xiaoyan CHEN1, Wenjie ZENG1
Department of Gynecology, Zhejiang Provincial People’s Hospital, Hangzhou, China. Background and Objectives: Cervical cancer screening is a critical tool in the early diagnosis and treatment of cervical lesions. The primary aim is to detect precancerous or cancerous cervical lesions in women through various screening techniques. Currently, cervical cytology and HPV DNA testing are the most commonly used methods. However, the inherent advantages and limitations of these screening methods have led to more than 30% of CIN2, CIN3, and invasive cancers being indistinguishable through cytology, resulting in clinical overdiagnosis or overuse of colposcopy. Similarly, HPV testing, with its high sensitivity and limited specificity, still cannot differentiate between transient self- limiting infections and those with a risk of progressing to cervical cancer. Therefore, there is a pressing need to develop an objective, easily interpretable, highly sensitive, and specific early screening or adjunctive diagnostic strategy for cervical cancer. Furthermore, this strategy should incorporate new biomarkers and technologies that can be applied in the context of non-invasive or minimally invasive sampling and have the ability to manage the follow-up of CIN2/CIN3 development into invasive cancer. This study aims to investigate the utility of PAX1 and JAM3 gene methylation detection as a triage tool for cervical cancer screening in women through a prospective study.
Methods: A prospective study was conducted between 2019 and 2022 at the Zhejiang Provincial People’s Hospital in China to evaluate the feasibility of opportunistic cervical cancer screening in outpatient settings. A total of 549 participants were enrolled in this study. All participants underwent cervical brush sampling to collect cervical exfoliated cells, and these cells were analysed using liquid-based cytology, HPV testing, and PAX1-JAM3 gene methylation detection (CISPOLY, China) and compared with pathological results. The positivity rate, sensitivity, specificity, and accuracy of all tests were analysed using Epidata 3.1 for data collection and SPSS 18.0 for statistical analysis.
Results: A total of 549 participants were enrolled in this study. Based on histological diagnosis, the participants included benign abnormalities (n=31), benign/CIN1 (n=321), CIN2 (n=44), CIN3 (n=36), cervical cancer (n=26), postoperative cases (n=28), and other malignant tumours (n=20) across all age groups. Compared to HPV (94.68% and 9.95%) and LBC (89.62% and 45.5%), PAX1- JAM3 dual-gene methylation detection had a sensitivity and specificity of 92.45% and 95.16%, respectively, for CIN2 in all age groups. The methylation performance for CIN3 was 98.39% and 86.78%, respectively. In the population aged 50 years or older, the sensitivity and specificity of dual-gene methylation detection for CIN2 were 100% and 93.98%, respectively, while those of HPV (89.47% and 14.61%) and LBC (91.3% and 54.17%) were lower. The cancer misdiagnosis rates of PAX1-JAM3 dual-gene methylation detection, HPV testing, and LBC were 0%, 5%, and 7%, respectively, across all participants.
Conclusion: In this single-center prospective study, we investigated the application value of PAX1 and JAM3 gene methylation detection for opportunistic cervical cancer screening in outpatient settings. By comparing the differences in gene methylation expression, HPV testing, and cytology, our data suggests that gene methylation detection has the potential to play an important role in cervical cancer screening among the Chinese population, particularly for patients with CIN2 (or below). In the future, it could be used as an independent biomarker for clinical cervical cancer diagnosis and triage. Therefore, methylation detection, as a new non-invasive diagnostic method, could serve as a screening tool for cervical lesions in women and as a second triage step after initial screening to reduce overtreatment and avoid missing cancer cases without sacrificing the need for colposcopy.
Which is more accurate in the diagnosis of high-grade cervical lesions: JAM3/PAX1 methylation or TCT/HPV?
- Xingping Zhao1, Dan Sun1, Xiang Li1, Dabao Xu1
Department of Gynecology, Third Xiangya Hospital of Central South University, Changsha, China. Objective: Currently, traditional cervical cancer screening methods, such as HPV testing and TCT, still have limitations. In this study, we explored the clinical value of DNA methylation (ΔCtP:PAX1 and ΔCtJ:JAM3) detection in cervical exfoliated cells for the diagnosis of high-grade cervical lesions, and aimed to identify new diagnostic biomarkers to achieve the goal of “precision screening”.
Methods: A total of 276 patients who underwent gynecological examinations at the Department of Obstetrics and Gynecology at Xiangya Third Hospital of Central South University from August to November 2022 were retrospectively selected. Among them, 242 patients had non-high-grade cervical lesions (control group) and 34 patients had high-grade cervical lesions (study group). The variables studied included general information (age, BMI, menopause status), TCT, HPV, cervical tissue pathology, vaginal examination results, and the ΔCt values of JAM3 and PAX1 gene methylation. Univariate and multivariate logistic regression analyses were used to identify the factors affecting the diagnosis of high-grade cervical lesions, followed by correlation analysis and construction of a conditional inference tree model. The detection efficiency of gene methylation detection for high- grade cervical lesions was also analyzed.
Results: Univariate and multivariate logistic regression analysis showed that ∆CtP, ∆CtJ, ASCUS, and HPV16 infection were independent risk factors for high-grade cervical lesions (P<0.05). Correlation analysis revealed a negative correlation between cervical pathology results and ∆CtP (r=-0.447, P<0.001) and ∆CtJ (r=-0.532, P<0.001). The conditional inference tree showed that when ∆CtJ>11.66, 96.4% of patients had non-high-grade cervical lesions, while when ∆CtP>10.97, only 0.9% of patients had high-grade lesions. The combination of ∆CtP, TCT, and HPV had the highest sensitivity (91.2%), positive predictive value (50.0%), negative predictive value (98.6%), and AUC (93.2%) among the six schemes analysed. The detection specificity of this scheme was 87.2%, second only to the specificity of ∆CtJ (88%). The detection efficiency of ∆CtP/∆CtJ alone was better than that of TCT or HPV alone. The combination of ∆CtJ, TCT, and HPV improved the sensitivity (88.2% vs. 76.5%) and negative predictive value (98.1% vs. 96.4%) compared with ∆CtJ alone, but did not improve specificity (84.7% vs. 88.0%) or positive predictive value (44.8% vs. 47.3%).
Conclusion: In this single-center retrospective study, for women with HPV infection, the accuracy of cervical cell DNA methylation detection for high-grade cervical lesions was superior to that of traditional TCT and HPV screening methods. Therefore, it is recommended for use in economically underdeveloped areas or large- scale cervical cancer screening programs. The combination of ∆CtP, TCT, and HPV is the most accurate screening method, but may increase screening costs.