Metadata
DOI: 10.36205/trocarAB.20232
Video Presentations
Vd Cornual Pregnancy on Ipsilateral Side After Right Salpingectomy per Laparoscopy Less Than 6 Months
- Ismail M., Ritonga Mulya NA. Prasetiyo, NE.
Division Fertilization and Endocrinology Reproduction, Department of Obstetrics and Gynecology, Medical Faculty of Padjadjaran University Objective: To report a patient with a natural pregnancy in the ipsilateral horn after a laparoscopic salpingectomy of less than 6 months prior.
Method: A woman with history of right laparoscopic salpingectomy for right tubal abortion, experienced an ectopic pregnancy less than 6 months later in the ipsilateral horn. The current pregnancy is a natural one. The ß-hCG value was 10,670 mIU/mL. Ultrasound examination found a gestational sac with a heart rate present in the right horn.
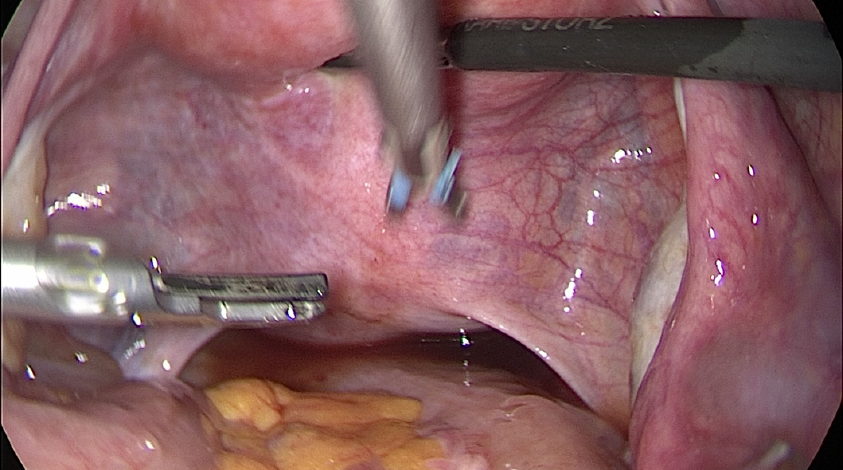
Results: Ectopic pregnancy may occur in the ipsilateral horn even after total salpingectomy. Possible pathophysiology in this case is the presence of risk factors for infertility and previous ectopic pregnancy. A 24-year-old woman with G2P0A1 5-6 weeks pregnant, referred to one private hospital in Bandung, was diagnosed with ectopic pregnancy and complained about right abdominal pain. Clinical examination of the patient showed blood pressure within normal limits, tachycardia, respiratory rate within normal limits, and body temperature within normal limits. Transvaginal ultrasound results showed that the gestational sac was in the right cornu. Laboratory examination were within normal limits. Wedge resection was performed laparoscopically.
Conclusion: It is important for clinicians to be able to recognize the location of an ectopic pregnancy by ultrasonography and to treat a cornual pregnancy using operative laparoscopy as an option.
VD Laparoscopic Myomectomy of a large Pedunculated Submucous Leiomyoma in an Unmarried Female – Case Report
- Renardiansyah T, Prasetyo NE.
Department of Obstetrics and Gynecology, Cibabat Regional General Hospital, Cimahi, West Java, Medical Faculty of Padjadjaran University. Indonesia Objective: The purpose of this case report is to report an unmarried patient with a pedunculated submucous leiomyoma that was removed by laparoscopic technique
Method: Patient with a history of recurrent vaginal bleeding who have had a leiomyoma found on ultrasonography and is planned for laparoscopic myomectomy.
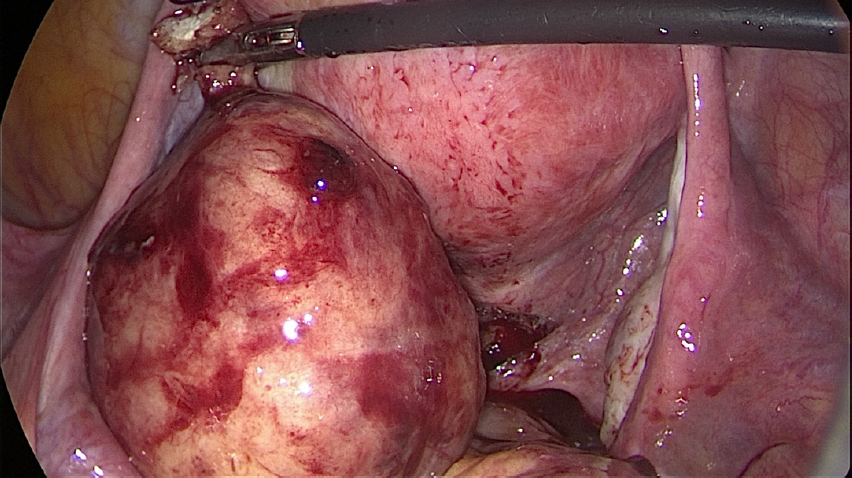
Result: A 40-year-old unmarried female with a history of recurrent vaginal bleeding since two year was diagnosed with a pedunculated submucous leiomyoma, because the patient wanted to preserve the hymen the operation was performed laparoscopically. The mass was pulled into abdominal cavity and the stalk of myoma was excised.
Conclusion: Laparoscopic myomectomy can be alternative approach for a case of pedunculated submucous leiomyoma in unmarried patient.
Introduction: Uterine leiomyomas are the most common benign pelvic tumour in females affecting up to 80% of women by the age of 50 (1). Nulliparity increases the risk. The most common symptoms are menstrual irregularity and pressure symptoms (2). The origin of the tertiary classification system is a design for sub- endometrial or submucosal leiomyomas that was originally submitted by Wamsteker et al. and subsequently adopted by the European Society for Human Reproduction and Embryology (ESHRE) (3). Some of the prolapsed pedunculated submucous myomas may belong to the FIGO type 1 or 2 classification, having an intramural component, and cause intraoperative haemorrhage. It is known that hysteroscopy has a high rate of success in controlling bleeding for submucosal myomectomy but the presence of a nascent myoma can make hysteroscopy challenging. There are several non-invasive methods to treat fibroids available now a days. In case recurrence of fibroids or multiple fibroids, the final options are myomectomy to (conserve the uterus for reproduction) or hysterectomy. To decrease the impact of surgery, laparoscopy has also been utilized. Major progress has been made with the introduction of laparoscopic techniques, as proven by randomized trials comparing the various approaches (4). Submucosal fibroids, in particular, lend themselves well to a hysteroscopic surgical approach. Clinicians must determine the location, number, percentage of the fibroids that is located in the uterine cavity, and marital status of the patient. The Wamsteker classification system, used by the European Society of Gynaecological Endoscopy (ESGE), can be helpful in determining the probability of successful removal of submucosal fibroids by hysteroscopic myomectomy (5). In this case report, we highlight the management for large pedunculated submucous fibroids in an unmarried nulliparous woman who wanted to conserve her fertility. She was managed by laparoscopic myomectomy.
Case Report: A 40-year-old Para 0 unmarried female was referred to Department of Obstetrics and Gynecology Cibabat Hospital with a history of abnormal uterine bleeding for two years. There were no complaints of nausea, vomiting, irregular bowel and bladder habits, decreased appetite, and weight reduction. Her age of menarche was 14 years followed by regular periods. There was no sexual activity and the patient was not currently taking oral contraceptives. there was no past medical history of diabetes, bronchial asthma or hypertension. Over the past year, the patient’s periods have become significantly heavier, with more and painful cramps, for which she has self-treated with NSAIDs. She went to three different gynaecologists and was given hormonal therapy to overcome her symptoms but she was not getting any better. She also was given three blood transfusions. On general examination she was in fair general condition, well-built and well-nourished with adequate hydration. There was no pallor, cyanosis, icterus or any significant lymphadenopathy. She had no pedal or sacral oedema. The vital signs were stable. The cardiovascular, respiratory and the central nervous systems were clinically within the normal. abdominal examination revealed no tenderness but there is palpable mass. The liver and the spleen were not palpable. A pelvic ultrasound done reported an anteverted uterus with a pedunculated fibroid measuring 6 x 5 cm. Both the ovaries were not seen. The haemoglobin was 11.6gms/dl and the urea and electrolytes were normal. Her blood group was B Rh positive. A diagnosis of a large pedunculated uterine fibroid was made and she opted for a laparoscopy with a possible laparotomy, after discussing all the available options.
Figure 1. Transvaginal ultrasound results in a patient. A routine pneumoperitoneum was created. At laparoscopy a good view was obtained. The liver and gall bladder appeared normal. Both the ovaries and fallopian tubes were normal. The ovarian fossa, pouch of Douglas and uterosacral ligaments were devoid of any endometriotic lesions. The uterus was normal, but there was a mass that filled the pouch of Douglas suggesting a pedunculated submucous fibroid.
Figure 2. Image of mass before excision
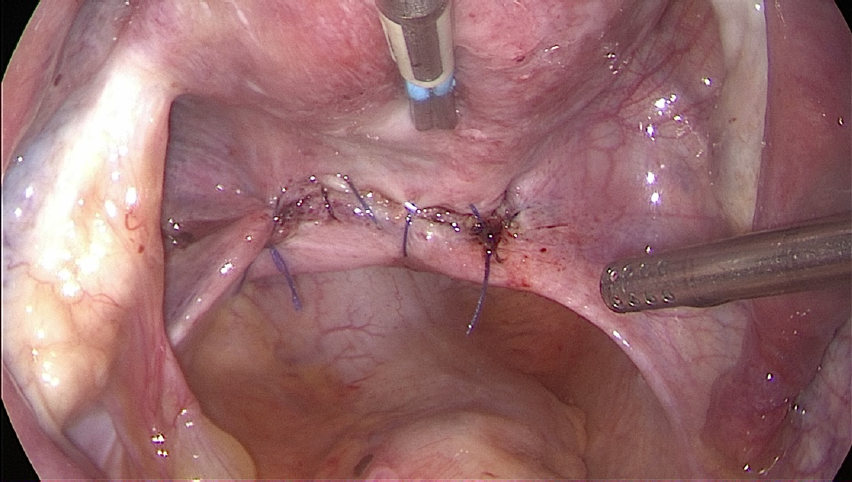
- Figure 3. Image of mass after excision. A needle is inserted into the abdominal cavity and fixed in the fundus of the uterus to keep the uterus in anteflexion. An incision was made in the pouch of Douglas to penetrate the vaginal cavity using a harmonic scalpel. Once the vaginal cavity opened, the mass was identified and fixed using a myoma screw and then pulled into the abdominal cavity. The stalk of the myoma is then identified and cut using the harmonic scalpel. The defect was closed in a single layer using intracorporeal sutures. The fibroid was delivered by morcellation. The estimated blood loss was 100 ml. Bilateral ureteric peristalsis was evident. The specimens were sent for histological evaluation, which confirmed a leiomyoma.
Figure 4. Post excision mass sutures
Discussion: Leiomyoma is a common uterine pathology, and it is the leading cause of hysterectomy in premenopausal women. Leiomyoma can be subserous, intramural, or submucous. Of all the myomas, 5% are submucous, of which 1.3%–2.5% are pedunculated and have the chance of prolapse. The degree of prolapse outside the uterine cavity is variable. It might be partially prolapsed in the cervix, completely in the vagina, or outside the vagina and the introitus (6). Although many submucosal myomas are operated on using hysteroscopic techniques, this patient is more special because the patient is not married and presents with an unperforated hymen (5). Laparoscopic myomectomy is a safe and feasible procedure in appropriately selected patients. it is already shown in a series of reports that pregnancy rates between 36 and 65% can be expected following myomectomy done via laparotomy, in infertile women (7). In most cases of large prolapsed fibroids, hysterectomy is a common planned intervention especially if it is a large myoma, and the patient has completed her family and is willing to lose her uterus. Hysterectomy can also be performed as an emergency lifesaving measure if associated with severe haemorrhage or sepsis (with or without uterine inversion), or if myomectomy failed. Our patient wanted to preserve her uterus, and hysterectomy was not acceptable to her unless it was required as an emergency procedure (5). Intraoperatively, an incision was made in the pouch of Douglas to penetrate the vaginal cavity using a harmonic scalpel. When it entered the vaginal canal, the mass was identified and fixed using a myoma screw then pulled into the abdominal cavity. The stalk of the myoma is then identified and cut using the harmonic scalpel. Challenges to this technique are the difficulty to grasp the myoma with an instrument, and resistance to rotation due to a thick pedicle or impaction. In our case, the myoma was dense enough to be fixed by myoma screw. In such large myomas, histopathological evaluation is important to exclude sarcomas that may mimic a benign leiomyoma in clinical behavior and macroscopic features (5).
Conclusion: Uterine fibroids are a significant health issue, negatively affecting a woman’s quality of life Because of their bulk and bleeding symptoms. Treatment options range from expectant management to alternative minimally invasive therapies to major surgery. Submucosal fibroids, in particular, lend themselves well to a hysteroscopic surgical approach, but in but in daily practice we have to look again at the status of each different patient. In patients who are unmarried and have a pedunculated submucous leiomyoma laparoscopic myomectomy may be an alternative therapy. Our case demonstrated an uneventful removal of a large submucosal leiomyoma using a laparoscopic myomectomy.
- References:
- Mauri F, Lambat Emery S, Dubuisson J. A hybrid technique for the removal of a large prolapsed pedunculated submucous leiomyoma. J Gynecol Obstet Hum Reprod [Internet]. 2022;51(5):102365. Available from: https://doi.org/10.1016/j.jogoh.2022.102365
- Pottala M, Jajoo SS. Multiple Uterine Fibroids in a Young Unmarried Woman. J Evol Med Dent Sci. 2020;9(13):1110–2.
- Munro MG, Critchley HOD, Broder MS, Fraser IS. FIGO classification system (PALM-COEIN) for causes of abnormal uterine bleeding in nongravid women of reproductive age. Int J Gynecol Obstet [Internet]. 2011;113(1):3–13. Available from: http://dx.doi.org/10.1016/j.ijgo.2010.11.011
- Farris M, Bastianelli C, Rosato E, Brosens I, Benagiano G. Uterine fibroids: An update on current and emerging medical treatment options. Ther Clin Risk Manag. 2019; 15:157–78.
- Guo XC, Segars JH. The Impact and Management of Fibroids for Fertility. An Evidence-Based Approach. Obstet Gynecol Clin North Am. 2012;39(4):521–33.
- Al-Shukri M, Al-Ghafri W, Al-Dhuhli H, Gowri V. Vaginal myomectomy for prolapsed submucous fibroid: It is not only about size. Oman Med J. 2019;34(6):556– 9.
- Parkar RB, Chudasama A, Chudasama M. Laparoscopic myomectomy of a large pedunculated fibroid: Case report. East Afr Med J. 2008;85(7):362–4.
VD Laparoscopic Resection of Caesarean Scar Ectopic Pregnancy Following Failed Methotrexate.
- Inge Putri
Objective: The incidence of a scar ectopic pregnancy is ~ 1:2000, rising to about 6% amongst women who have had a previous caesarean section, and the incidence is rising (1)
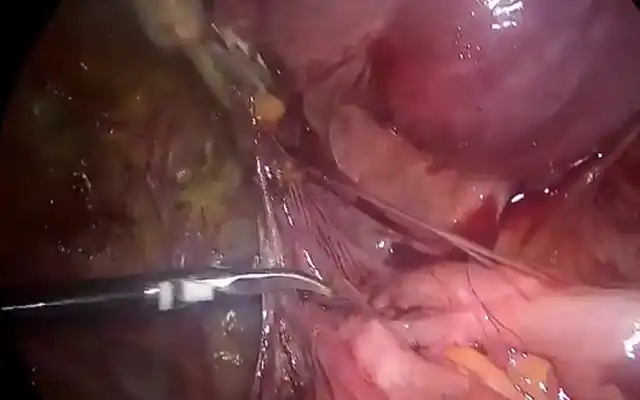
Methods and Results: We describe a case report of a 25yo with 2 previous caesarean sections and 2 suction evacuation of retained products with an ultrasound finding of scar ectopic pregnancy, she had B-hCG 104,220, she received intra gestational sac as well as IM methotrexate. Over the next 2 months, her B-hCG was negative, however, she had ongoing PV spotting. She had a repeat ultrasound which showed a 2×2 cm, hypoechoic lesion around C/S scar site. She underwent a laparoscopic excision of scar ectopic pregnancy. The video highlights key strategies to minimize blood loss:
- Temporary ligature of the uterine arteries with Liga clips
- Temporary ligature of the Infundibulo Pelvic ligament with Liga clips
- Injection of vasopressin into surrounding myometrium
Intraoperatively, a large scar ectopic measuring 4cm was found, wedge resection was performed to minimize myometrial excision, extremely adherent products of conception was removed. Hysterotomy was closed with 2 layers of 2-0 Vloc sutures. A foley’s catheter was placed intrauterine and patient placed on oestrogen 4mg daily to encourage healing and prevent adhesions. The patient was discharged home day two following surgery.
Conclusion: The management of scar ectopic pregnancies remains an ongoing challenge, the administration of methotrexate has a 50% chance of requiring further additional intervention. In this video, we describe steps of a safe excision of scar ectopic pregnancy whilst conserving fertility (2).
References:
- Caesarean scar pregnancy, Up to date, retrieved from https://www.uptodate.com/contents/cesarean-scar-pregnancy on 14th Jan 2023
- CM Pickett, N Minalt, OM Higgins, et al. laparoscopic approach to Cesarean scar ectopic pregnancy, American Journal of Obstetrics and Gynecology, Volume 226, Issue 3, 2022, Pages 417-419, https://doi.org/10.1016/j.ajog.2021.11.021.
VDO Fitz-Hugh-Curtis Syndrome: Release or Not?
- IGNB Surya Udayana1, Dian Tjahyadi 2, Tono Djuwantono 2
1 Fertility Trainee, Padjajaran University, Hasan Sadikin Hospital, Bandung, West Java, Indonesia Indonesian Gynecologic Endoscopy Society Member
2 Fertility Consultant, Hasan Sadikin Hospital, Bandung, West Java, Indonesia Email : igustingurah.iges@gmail.com / drsuryaspog@gmail.com Hp:082146555339 Objective: Fitz-Hugh-Curtis syndrome (FHCS) is defined by the presence of perihepatic inflammation associated with pelvic inflammatory disease (PID) (1,2). Upper right abdominal pain and tenderness are the most common symptoms that makes patients go to the emergency center (1,3). About 39 million (11% of the global estimate) cases of Sexually Transmitted Infections (STI) and PID occur in South-East Asia in 2012 (4). The treatment of FHCS coincides with PID treatment. Some cases need surgical intervention to release the adhesions (3). Therefore, the authors would like to investigate and discuss this further in order to give some perspective about the FHCS.
Methods: To achieve a comprehensive review from numerous studies regarding the topic discussed in this review, the authors have explored many resources by using both general web search engines and scientific search engines such as PubMed, ScienceDirect, and other online medical journal search engines. All the articles used in this review have been collected using the keywords “Fitz Hugh Curtis syndrome”, “Perihepatic Adhesion”, “Pelvic Inflammatory Disease”, and “Perihepatic Inflammation’.
Results: After a comprehensive review, the authors have identified 28 articles five of these were excluded due to confounding and eligibility issues. At the end, the authors reviewed the 23 articles obtained. Fitz- Hugh-Curtis syndrome or FHCS is an inflammation of the liver capsule with adhesion formation resulting in abdominal pain in the right upper quadrant. FHCS Often occurs in women of childbearing age, it’s an uncommon disease. FHCS is the chronic manifestation of pelvic inflammatory disease (PID). The adhesion formation doesn’t involve the liver parenchyma (3,4). Adhesion formation between anterior liver capsule and anterior abdominal wall or diaphragm is described as ‘violin string’ adhesion (5,6). This syndrome was first introduced in 1920 by Carlos Stajano. Curtis (1930) associated the syndrome with PID caused by Neisseria gonorrhoeae and Fitz-Hugh, Jr. (1934) correlated it with acute gonococci peritonitis compromising in abdomen (3,7). Although Neisseria gonorrhoeae has been considered as a causative microorganism, in recent years Chlamydia trachomatis is considered the most frequent cause of FHCS (8). The microorganisms associated with PID spread through either one of three ways: 1) Spontaneous ascending infection where microorganisms from cervix or vagina migrate to the endometrium, then through the fallopian tubes into the peritoneal cavity, 1.Lymphatic spread such as infection of the parametrium from an intrauterine device (IUD), or 2. Hematogenous spread such as tuberculosis infection (3,4,7).
FHCS usually presents as pain in the right upper quadrant (RUQ) of abdomen (9). Its symptoms are also associated symptoms of PID such as fever, lower abdominal pain and vaginal discharge. The quality of RUQ pain is typically sharp, pleuritic and aggravated by movements and frequently referred to the right shoulder or inside of the right arm. The RUQ pain is due to adhesions between the anterior surface of liver and abdominal wall (peritoneum). Symptoms like nausea, vomiting, hiccupping, night sweats, headache, malaise may also be experienced following the RUQ pain, and in rare case with upper left abdominal pain (1,5,10,11).
Diagnosing FHCS may be challenging since its presentation is similar to many diseases with other right upper quadrant abdominal pain (8). It should be diagnosed early and treated empirically to prevent unwanted complications such as infertility and ectopic pregnancy. Physician who suspects FHCS should give more attention on high-risk behaviours and symptoms in the appropriate populations. Some risk factors to consider include age less than 25 years old, first sexual intercourse at age under 15 years, a history of PID, the use of IUD, recent IUD insertions, and vaginal douching. Patient’s history such as exposure to a new sexual partner or symptomatic sex partners can give a significant clue (3,12). When RUQ pain occurs in women of childbearing age, clinicians should consider perihepatitis or FHCS (11,13). Although RUQ pain is not always heavy, the intraabdominal disease process is already in progress. The most important criteria in preoperative FHCS are RUQ pain, the presence of PID, and perihepatitis with no involvement of liver parenchyma (8).Physical examination may find abdominal tenderness and the presence of cervical motion tenderness and vaginal discharge can be helpful for patient suspected with PID (14,15). Murphy’s sign may be positive in FHCS patient (16). A friction rub can be heard along the right anterior costal margin in FHCS, described as ‘beautiful new snow creaking friction’ (10). Physicians should think of the likelihood of PID if the patient that presents any the following symptoms: fever (>38.3oC), abnormal cervical mucopurulent discharge, elevated erythrocyte sedimentation, leucocytosis on saline microscopy of vaginal fluid, elevated C-reactive protein, and laboratory documentation of cervical infection with Neisseria gonorrhoeae or Chlamydia trachomatis (12,17). Perihepatitis can be distinguished from other causes of RUQ pain by direct visualizing by laparotomy or laparoscopy
(1). Visualization of violin-string-like adhesions by laparoscopy is the gold standard for diagnosing FHCS. Diagnostic imaging equipment including ultrasonography (USG), computed tomography (CT) is also being used (14). USG is used to evaluate the gallbladder and the liver, excluding cholelithiasis and cholecystitis, and also to assess tubo-ovarian abnormality as a sign of PID. CT scan with arterial and portal phases can be performed. CT can show the thickening of hepatic capsule and the accumulation of subcapsular fluid (10,18,19). FHCS degrees of adhesion formation include grade I adhesions consisting of violin adhesions which are fragile and friable and can easily be broken at laparoscopy either by the insufflation of CO2 or by instruments. Grade II adhesions are white fibrous plaques ang very small haemorrhagic spots on the diaphragm and liver surface and grade III are densely fibrotic and vascular adhesions with “Hanging Liver” feature. The presence of these adhesions may or may not be accompanied with laparoscopic evidence of PID (15). The therapy of FHCS consist of treating the PID infection, since FHCS emerges from PID. The goals are to relieve the symptoms, eradicate the infection, and minimize or prevent long-term sequelae. In order to clarify the treatment and clinical progress of FHCS, the disease is defined into three groups acute asymptomatic, acute symptomatic, and chronic asymptomatic, then a decision is made concerning the appropriate treatment. Active treatment like adhesion release or adhesiolysis and adequate antibiotics must be used in the acute asymptomatic phase patients who present unclear symptoms and patients with acute symptomatic FHCS accompanied by PID (8). Parenteral or oral regimens both have similar efficacy in treating woman with PID. The gold standard seems to be cefotetan two grams IV every 12 hours or cefoxitin two grams IV every 6 hours with doxycycline 100 mg orally or IV every 12 hours for parenteral treatment, and ceftriaxone 250 mg IM single dose with doxycycline 100 mg orally twice a day for 14 days, with or without metronidazole 500 mg orally twice a day for 14 days oral treatment. Perihepatic adhesion should be lysed by laparoscopy, especially in the acute phase to confirm the diagnosis and relieve RUQ pain secondary to adhesions (6,10,20).
Although there have been no direct reports, we found some complications that can occur when releasing adhesions, including peritoneal injury, liver injury, subcapsular liver haemorrhage due to retraction on a release or overly aggressive technique of adhesiolysis. The best technique to avoid these complications, is the use of sharp on-point dissection, not to perform excessive manoeuvres and retractions, and to prioritize mild adhesions (Grade I-II). In the case patients do complain of RUQ or severe adhesions, adhesiolysis can be carried out in collaboration with digestive surgeons (15).
In a study from Faré (2018), a 23-year-old woman was diagnosed FHCS based on the symptoms and the urine polymerase chain reaction (PCR) test which was positive for Neisseria gonorrhoeae and Chlamydia trachomatis. The patient was treated with doxycycline and single dose of ceftriaxone with rapid improvement and no relapses at follow-up (21). A different case from Cugliari (2022), a 15-year-old female came to the emergency department with nausea and vomiting for three days and diffuse abdominal pain for two days. The patient was sexually active with two male partners. Laboratory findings were positive for leucocytosis and elevated platelets. At laparoscopic appendectomy, chronic thickening of appendix was seen and confirmed as appendicitis. Small bowel obstruction with multiple bands on the right side of pelvis were released. Adhesions were noted on the right and left lobe of the liver to the abdominal wall and the ileal portion of the small bowel. Adhesions were released and antibiotics cefoxitin, doxycycline, and metronidazole were used postoperatively (22). A study from Hmaidan (2022) reported two patients with FHCS. One patient (FHCS with PID) underwent laparoscopy and the other (FHCS without any pelvic disease) underwent robotic surgery. Both of them did experience the disappearance of the pain by releasing perihepatic adhesions (23). Saurabh (2012) presented FHCS in a 29-year-old African American male. The patient came with history of diarrhoea, right side abdominal pain and abdominal distention. CT scan showed free fluid in pelvis. After the conservative treatment (IV fluid and pain medication), his symptoms remained unchanged. A second CT scan showed mild increase of the free fluid in pelvis. The patient underwent laparoscopic surgery, there were extensive adhesions between liver and anterior abdominal wall. Adhesions were release by electrocautery and Endo Shears. Patient reported complete disappearance of his symptoms (18). A Study from Hong et al. (2010) reported ten cases of FHCS with CT and 101 cases of violin string appearance between the liver surface and the anterior peritoneal wall suggesting perihepatitis at laparoscopy out of 3674 laparoscopies. Among 101 cases, 23 cases were detected during laparoscopy for endometriosis, 16 for gynecological malignant tumours, 16 for benign adnexal disease, 13 for uterine leiomyoma, 7 for PID, 2 for peritoneal tuberculosis and 21 for other gynecological diseases (8). A case report from Abul-Khoudoud (2001) reports a 51-year-old woman with RUQ and epigastric pain, diagnosed with FHCS. Exploration through laparoscopy revealed distention of proximal two-thirds of small bowel and multiple adhesions between the right lobe of liver and the anterior abdominal wall. Mechanical small bowel obstruction did occur secondary to a suprahepatic adhesion at the liver. The adhesions were lysed sharply through five mm right upper quadrant trocar (6).- Conclusion: Fitz-Hugh-Curtis syndrome (FHCS) is chronic manifestation of pelvic inflammatory disease (PID), which presents right upper quadrant (RUQ) abdominal pain as a result of perihepatic adhesion formation between the anterior surface of the liver and the abdominal wall. Neisseria gonorrhoeae and Chlamydia trachomatis are the most causative bacteria for PID that leads to FHCS. The treatment of FHCS goes parallel with PID. When FHCS diagnosis is confirmed by laparoscopy, surgeon should decide to release the adhesions or not and then initiate empiric antibiotic treatment. Adhesiolysis or releasing perihepatic adhesions is performed by done by laparoscopic surgery. Whenever feasible, we can consider to perform adhesiolysis especially when the patient is complaining of RUQ pain, the adhesion is mild (FHCS grade I-II), and the surgeon is confident in her/his skills to release the adhesion. But when the risk outweighs the benefit, in case the adhesion is severe and a high probability of complication like liver subcapsular haemorrhage exists, we can reconsider to release the adhesion or plan a collaboration with the digestive surgeon. There is a need for more reports about FHCS to decide on adhesiolysis. Still, releasing the adhesion and appropriate antibiotic therapy are needed to prevent recurrent adhesion and complications in the future.
- References:
- Ekabe CJ, Kehbila J, Njim T, Kadia BM, Tendonge CN, Monekosso GL. Chlamydia trachomatis-induced Fitz-Hugh–Curtis syndrome: a case report. BMC Research Notes. 2017 Dec;10(1):1-4.
- Nakagawa H, Miyata Y. Pain on Lying in the Supine Position Due to Fitz-Hugh-Curtis Syndrome. Internal Medicine. 2022:8990-21.
- Basit H, Pop A, Malik A, Sharma S. Fitz-Hugh-Curtis Syndrome. InStatPearls [Internet] 2021 May 7. StatPearls Publishing.
- Moving ahead on elimination of sexually transmitted infections (STIs) in WHO South-East Asia Region – progress and challenge. New Delhi: World Health Organization, Regional Office for South-East Asia; 2018. Available from: https://apps.who.int/iris/handle/10665/330031
- Nardini P, Compri M, Marangoni A, D’Antuono A, Bellavista S, Calvanese C, et al. Acute Fitz-Hugh-Curtis syndrome in a man due to gonococcal infection. The Journal of Emergency Medicine. 2015 Mar 1;48(3):e59-62.
- Newson DL. Fitz-Hugh Curtis Syndrome. FHC syndrome information. patient [Internet]. Patient.info. 2015 [cited 2023Jan8]. Available from: https://patient.info/doctor/fitz-hugh-curtis-syndrome.
- Abul-Khoudoud OR, Khabbaz AY, Butcher CH, Farha MJ. Mechanical partial small bowel obstruction in a patient with Fitz-Hugh-Curtis syndrome. Journal of Laparoendoscopic & Advanced Surgical Techniques. 2001 Apr 1;11(2):111-4.
- Ricci P, Lema R, Solá V, Fernández C, Fabres C, Fernández E, et al. Fitz-Hugh–Curtis syndrome: Three cases of incidental diagnosis during laparoscopy: Asymptomatic Fitz- Hugh–Curtis syndrome. Journal of Obstetrics and Gynaecology. 2008 Jan 1;28(3):352- 4.
- Hong DG, Choi MH, Chong GO, Yi JH, Seong WJ, Lee YS, et al. Fitz-Hugh–Curtis Syndrome: Single centre experiences. Journal of Obstetrics and Gynaecology. 2010 Apr 1;30(3):277-80.
- Uwagbale E, Samuel O, Agbroko S, Samuel G. Fitz Hugh Curtis Syndrome: The Zebra Amongst the Horses With Right Upper Quadrant Abdominal Pain. The American Journal of Gastroenterology. 2022 Oct;117(supp):S1936-37.
- Theofanakis CP, Kyriakidis AV. Fitz-Hugh–Curtis syndrome. Gynecological Surgery. 2011 May;8(2):129-34.
- Greydanus DE, Cabral MD, Patel DR. Pelvic inflammatory disease in the adolescent and young adult: An update. Disease-a-Month. 2022 Mar 1;68(3):101287.
- Lin L, Tirado A, Mateer E, Galwankar S, Tucci V. Ultrasound killed the pelvic examination: Over-reliance on ultrasound resulted in delayed diagnosis of Fitz-Hugh– Curtis syndrome and potential loss of fertility in a young female patient. Journal of Emergencies, Trauma, and Shock. 2022 Jul 1;15(3):146-8.
- Matsuura H, Kishida M, Shimizu W. Right Upper Quadrant Pain With Positive Murphy’s Sign in a 19-Year-Old Woman. Gastroenterology. 2020 Apr 1;158(5):e3-4.
- Bolaji I, Sze K Y. An odyssey through Fitz-Hugh Curtis syndrome. Journal of Reproduction and Contraception. 2015 26(3): 173-186.
- Vicini S, Bellini D, Panvini N, Rengo M, Carbone I. Hepatic pseudo-lesion as an unusual presentation of Fitz-Hugh-Curtis syndrome. Radiology Case Reports. 2021 Oct 1;16(10):3060-3.
- Shikino K, Ikusaka M. Fitz-Hugh-Curtis syndrome. BMJ Case Reports. 2019;12(2).
- Yamaguchi T. Hiccups Caused by Fitz-Hugh-Curtis Syndrome. Balkan Medical Journal. 2022 Jul 1;39(4):299-300.
- Di Rocco G, Giannotti D, Collalti M, Mele R, Pontone S, Frezzotti F, et al. Acute abdominal pain in a 24-year-old woman: Fitz-Hugh-Curtis syndrome associated with pyelonephritis. Clinics. 2012;67:1493-5.
- Saurabh S, Unger E, Pavlides C. Fitz-Hugh-Curtis syndrome in a male patient: a case report and literature review. Case Reports in Surgery. 2012 Jan 1;2012.
- Muschart X. A case report with Fitz–Hugh–Curtis syndrome, what does it mean?. Acta Clinica Belgica. 2015 Sep 3;70(5):357-8.
- You JS, Kim MJ, Chung HS, Chung YE, Park I, Chung SP, et al. Clinical features of Fitz- Hugh-Curtis Syndrome in the emergency department. Yonsei medical journal. 2012 Jul 1;53(4):753-8.
- Faré PB, Allio I, Monotti R, Foieni F. Fitz-Hugh-Curtis syndrome: a diagnosis to consider in a woman with right upper quadrant abdominal pain without gallstones. European Journal of Case Reports in Internal Medicine. 2018;5(2).
- Cugliari MK, Pandit T, Pandit R. Small Bowel Obstruction and Appendicitis in Patient With Fitz-Hughes-Curtis Syndrome. Journal of Medical Cases. 2022 Jul;13(7):335.
- Hmaidan S, Mutter O, Muldoon O, Moawad G, Yunker A. Laparoscopic and robotic management of perihepatic adhesions. American Journal of Obstetrics & Gynecology. 2022 Mar 1;226(3):S1358-9.
VDO Hysteroscopic Release of Intrauterine Adhesion and Amniotic Membrane Transplantation in a Patient with Recurrent Amenorrhea due to Intra Uterine Adhesion (IUA).
- Lestari Kartika
Nunukan Hospital, North Kalimantan, Indonesia Objective: To describe a case of amenorrhea due to Intra Uterine Adhesion (IUA) that already underwent two times an operative hysteroscopy, the last hysteroscopy was in conjunction with amniotic membrane transplantation technique to improve endometrial growth.
Method: Report of one case
Result: Mrs. K, 33 years old, with primary infertility eight years, the main complaint was secondary amenorrhea for three years. The patient first came to visit in 2021 due to an amenorrhea of one year, a history of curettage, three years before the visit, due to suspected endometrial hyperplasia (no pathology report). In 2021 the patient underwent a diagnostic hysteroscopy, there was a cervical stenosis and uterine synechiae, a transcervical resection of the endometrial adhesion (TCRA) was performed using Hegar dilators under ultrasonic guidance, after that, we took an endometrial biopsy and an intrauterine device (IUD) was placed, patient was given cycloprogynova for three months, the pathology report was chronic endocervititis. The patient was lost to follow up, until 2023. She came again due to an amenorrhea of six months. She told that in 2021, three months after taking cycloprogynova, she did visit another gynaecologist, the IUD was removed and she was given oral contraception/OCP, and she did experience spotted menstruation, but when she stopped the OCP, she no longer had menstrual periods. In 2023, a hysteroscopy was performed, the uterine cavity was opened, the endometrial layer was thin, and there were filmy adhesions at the fundus, and some endometrial polyp at the cornu. A polypectomy was performed and the synechia was released in conjunction with an amniotic membrane transplantation. Patient was advised to take progynova 2×2 mg this regimen did cause scanty menstruations, then cycloprogynova was prescribed. A diagnostic hysteroscopy was planned three months after the last one.
Conclusion: The current traditional management of severe intrauterine adhesions (IUA) is hysteroscopic adhesiolysis with application of either an intrauterine contraceptive device or a Foley catheter balloon with reported recurrence in up to 50% of cases. Recently, there are some study discussing the use of amniotic membrane graft after hysteroscopic lysis of severe IUA, and some study reported the significant improvement in the volume of menstruation, and the severity of intrauterine adhesions. The amnion seems to supress the endometrial adhesion formation and to promote endometrial regeneration.
VDO The Use of Epinephrine During Laparoscopic Myomectomy, Is It Safe?
- Lestari Kartika
Nunukan Hospital, North Kalimantan, Indonesia. Objective: To describe a case of laparoscopic myomectomy using Epinephrine as vasoconstrictor in order to reduce blood loss, there was an increase in blood pressure, soon after the injection, but fortunately this was managed by anesthesiologist without any complications.
Method: Report of one case
Result: Mrs S, 33 years old, primary infertility of one and a half year, as main complaint and lower abdominal discomfort. Physical examination, BMI 22 kg/m2, no history of operations. On vaginal examination, the uterus was slightly enlarged, a myoma was palpated at the left the uterine corpus. Transvaginal ultrasound revealed a 4,5 cm x 4,3 cm fibroid at the left anterior side of the uterus. I performed a laparoscopic myomectomy, using a uterine manipulator and three accessory trocar ports, epinephrine was used as haemostatic agent. 1 cc epinephrine was diluted in 200cc NaCl 0.9%, 40 cc of solution was injected in the myoma capsule. Apart from being a hemostatic agent, this solution also useful as a hydro dissection that separates the myoma tissue from the normal myometrial tissue. Soon after the injection an increased blood pressure was observed, immediately treated by the anesthesiologist in less than 5 minutes. After the injection, I could perform the enucleation of the myoma easily, total blood loss was 50 cc, and the duration of the operation was shortened.
Conclusion: There are several ways to reduce the amount of bleeding during a laparoscopic myomectomy. These include tourniquets, the use of vasoconstrictor agents, and a temporary uterine artery ligation. The most preferred vasoconstrictor agent is vasopressin, apart from its more local action, it also has a shorter half-life than epinephrine. However, in some remote areas, vasopressin is difficult to obtain, so the use of epinephrine is an option. Based on this case, the use of intramyometrial application of epinephrine seems to be safe but leads to significant alterations of the hemodynamic parameters, whereas the use of a tourniquet requires high skills, risk of hematoma and longer duration of surgery. So, a good teamwork, especially with anesthesiology is the main key to overcome the hemodynamic disturbances from epinephrine.
VDO Variations of the Shoelace Knot Laparoscopic Technique Bilateral Uterine Arteries in Miomas Covering the Pelvic Cavity
- dr. Arry Soryadharma, Sp.OG
dr. Nogi Eko Prasetyo., Sp.OG., Subsp F.E.R
Not available in English. - Study Objective: The purpose of this case report is to report a case of laparoscopic myomectomy with the method of preventing bleeding using the shoelace knot method in myoma covering the pelvic cavity.
Study Design: Video demonstration
Place: Cibabat Regional General Hospital
Methods: Reporting video recordings of laparoscopic myomectomy in a case of solitary intramural uterine leiomyoma measuring 15 cm (covering the pelvic cavity) at Cibabat Cimahi Hospital, using the shoelace knot bleeding prevention method.
Intervention: Bilateral uterine arteries can be seen after dissection of the peritoneum above the triangle formed by the round ligament, infundibulopelvic ligament, and pelvic sidewall. 30 cm PGA 2-0 suture with a knot at one end, around the exposed uterine artery, make a loop at the other end, then tie it by taking the end of the knotted thread. In this case the left uterine artery was exposed with a posterior approach, namely opening the peritoneum from the lateral side of the left infundibulopelvic ligament, however, due to the position of the tumor covering the right lateral and anterior, the right uterine artery used a medial approach, namely opening the peritoneum from the medial right infundibulopelvic ligament. Then, the right uterine artery is tied in the same way. Laparoscopic myomectomy was performed. After the procedure is completed, the knot is released by pulling on the free end, restoring the blood supply to the uterus.
Conclusion: For gynecological laparoscopic practitioners, learning different approaches in stripping the uterine arteries dan ureter is very important, so that in the case of tumors covering the pelvic cavity, different safest approaches can be used.
Keywords: Shoelace knot, myomectomy, myoma uteri, posterior approach, medial approach
VDO Removal of Myomas Through the Vagina in Laparoscopic Surgery: A Case report.
- Caesar Kurniawan1, Yuli Trisetiyono1
1Department of Obstetrics and Gynecology, Faculty of Medicine, Diponegoro University, Kariadi General Hospital, Semarang, Indonesia. Introduction: A 36-year-old woman with as main complaint secondary infertility for six years, currently the patient still menstruates regularly every month but accompanied by pain. The patient changes pads 2-3 times every day during menstruation. Gynaecological examination and transabdominal ultrasound show a uterine myoma with a diameter of 6.9 x 2.8 x 4.8 cm and ultrasound shows a whorl like, spiral shape, pattern with a ring of fire. The patient is planned for laparoscopic myomectomy.
Surgical Technique: A total of 4 incisions were made for the insertion of one primary trocar and three secondary trocars. The manipulator was installed and then CO2 gas insufflated into the abdominal cavity. All of the trocars were put in directly into the abdominal cavity. After the myoma was identified, vasopressin infiltration of 1:100,000 IU around the lump was performed. Once the correct plane was entered, the myoma was dissected out of the uterus with the harmonic scalpel. The uterus bed was closed in single layers with barbed sutures and the myoma then removed through an incision of the posterior fornix. The largest spark plug guides are installed vaginally and pushed to make the posterior fornix protrude. The vagina is opened slowly from the abdominal side using harmonic scalpel until the opening is wide enough. The myoma is then pushed through this opening and identified through the vagina then pulled slowly using a Kocher or a tenaculum. The vaginal mucosa is sutured with an absorbable thread 2.0 laparoscopically.
Conclusion: The morcellator is indeed an instrument that greatly facilitates the removal of myomas from the abdominal cavity. However, this instrument has a disadvantage. The procedure cannot deal with blood vessels thus makes it difficult in cases of vascular cauterization and techniques are limited to Type II myoma. This procedure has a risk of spreading cancer cells in the peritoneal cavity. The morcellator is still an option in cases of large myoma (larger than duck’s egg) and cases of attachment to the pouch of Douglas. Another variation of the technique to minimize the spread of cancer cells is a vaginal hysterectomy. This method removes myomas by opening the posterior fornix into the birth canal. This method has the advantage of an leaving an unseen scar and minimizing the spread of cancer cells.
VDO Total Laparoscopy Retrograde Hysterectomy on Frozen Pelvis due to Severe Endometriosis: is it feasible and safe?
- Putera AR, Setiawan ME, Satria ML
Obstetrics and Gynecology, Fertility and Reproductive Endocrinology Department, Endometriosis Center Fatmawati Hospital, South Jakarta, Indonesia Objective: This study aims to evaluate the feasibility and safety of total laparoscopy retrograde hysterectomy on frozen pelvis due to severe endometriosis.
Material and Methods: This study was conducted retrospectively with a case-series observational study design. Sixteen endometriosis patients with grade IV classified based on revised-American Society for Reproductive Medicine classification who underwent total laparoscopic retrograde hysterectomy at Fatmawati Hospital-Jakarta from 2019 to 2022 were included in this study. Physical examination and transvaginal ultrasound were performed on all patients before surgery. Symptoms, a transvaginal ultrasound examination, and postoperative pathology results confirmed the diagnosis of endometriosis. Some data were collected, such as patient characteristics, history of symptoms, previous surgery, intraoperative and postoperative results.
Results: Sixteen patients with severe endometriosis at Fatmawati Hospital-Jakarta were included in this study. The mean age of the patients in this study was 42.75 (± 4.2) years. In this study, four patients had a history of one surgery (25%), two patients had a history two surgeries (12.5%), and ten patients (62.5%) had no history of previous surgery. Some of operations that patients in this study had undergone were caesarean section (12.5%), cystectomy (18.8%), and salpingo-oophorectomy (6.3%). Most patients experienced dysmenorrhea (93.8%), and only a small proportion experienced abnormal uterine bleeding (18.8%), dyspareunia (12.5%), and chronic pelvic pain (12.5%). Eleven patients (68.8%) had endometriotic cysts accompanied by deep infiltrating endometriosis (DE), two patients (12.5%) had only an endometroid cyst, and three patients (18.7%) had DE, the average size of endometrioma was 5.8 cm (± 2.96 cm). Besides endometrioma lesions, the patients had other abnormal findings, thirteen patients (81.3%) with adenomyosis with an average size of 4.29 cm (± 2.72 cm), three patients (18.8%) with hydrosalpinx, two patients (12.5%) with uterine fibroids, two patients with hydronephrosis (12.5%), one patient with a combination of cholelithiasis (6.3%) and nephrolithiasis (6.3%). Total laparoscopic retrograde hysterectomy was performed in all sixteen patients with frozen pelvis due to severe endometriosis, and concomitantly performed were bilateral salpingo-oophorectomy in thirteen patients (81.3%), unilateral salpingo-oophorectomy in two patients (12.5%), DIE resection in six patients (37.5%), ureterolysis in three patients (18.8%), and ureteroscopy with DJ stent insertion in one patient (6.3%). The average operating time was 4.27 hours (± 1.09), and the average length of stay was five days (± 3.25 days). The average estimated blood loss was 180 (80-500) cc, with two patients (12.5%) requiring blood transfusions. There were no conversions to laparotomy. Perioperative complications occurred in one patient (6.3%), having an ureterovaginal fistula. One patient (6.3%) was observed postoperatively in the intensive care unit for one day.
Conclusion: From this study, total laparoscopic retrograde hysterectomy with adhesiolysis is a safe and feasible surgical technique for severe endometriosis with severe adhesions. This is due to the low intraoperative bleeding rate, laparotomy conversion rate, intraoperative and postoperative complication rates.
VDO Immersion Procedure in Laparoscopic Surgery for Endometrioma Cystectomy new cystectomy technique to make it easier and no bleeding.
- Hary Tjahjanto
Reproductive Fertility Endocrinology Division-Obstetric Gynecology Department Kariadi Hospital/Medical Faculty-Diponegoro University, Indonesia .
e-mail = hary_tj@yahoo.com, harytjahjanto@gmail.com phone = +62-8122810945 Objective: Efforts that are always carried out in endoscopic surgery, especially endometrioma cystectomy, are looking for ways to exfoliate the walls of endometrioma cysts to cause minimal bleeding or no bleeding at all. Because the hilus area is formed by connective tissue it is difficult to separate the layers of the cyst wall, it is often necessary to cut the cyst wall around the hilus to reduce the risk of bleeding from the hilus.
Materials and Methods: The basis of the endometrioma immersion procedure is to allow osmosis to occur in the ovarian tissue and endometrioma wall. The process of osmosis refers to the movement of H2O molecules and is a passive process because it does not require energy and occurs automatically. In the process of osmosis, H2O molecules move from areas or tissues with a lower concentration (hypotonic) to tissues with a higher concentration (hypertonic) through a semipermeable membrane until an equilibrium is reached or approaches the osmotic pressure balance in each layer. The liquid used as irrigation can be in the form of sterile aqua or 0.9% NaCl, both of which contain H2O molecules. This fluid acts as an extracellular environment that has a low/hypotonic osmolarity. Endometrioma wall cells and ovarian tissue cells (stromal and cortex) that surround them act as a semi-permeable membrane and have a higher osmotic pressure. Immersion or soaking is done for 15 to 20 minutes. During this time period, osmosis is expected to occur. During the process of osmosis, H2O molecules from irrigation fluid will enter the cells in all layers of ovarian tissue and endometrioma wall, then these cells will swell and cause the bonds between tissues to become looser.
Immersion procedure: The surgeon performs an incision in the wall of the endometrioma using a harmonic scalpel on a thin, avascular wall section. Endometrioma fluid is suctioned until the endometrioma is empty or the suction is completed. The irrigation fluid is brought into the now empty cyst, until it is filled at capacity, and also into the pouch of Douglas. The endometrioma now contains irrigation fluid and is submerged in irrigation fluid in the pouch of Douglas. The cyst is left soaking for 15 – 20 minutes. The duration of immersion depends on the thickness of the cystic wall and the ovarian tissue that covers the cyst, and depends on how soft and hard the cyst wall is. After the osmosis process (15-20 minutes), the irrigation fluid is aspirated. Followed by exfoliating the cyst wall/stripping. This procedure makes the peeling process easier because the two layers of connective tissue are looser, there is very little bleeding, often there is no bleeding at all, and the cyst wall can be removed up to the hilus area.
Results: We have performed cystectomy with immersion procedure since 2017 at Kariadi Hospital (Semarang-Indonesia). Of the 60 endometrioma cases that underwent cystectomy with this immersion technique, approximately 90% did not have a bleeding that required cautery or ligation and in almost all of the subjects the cystic wall was taken out up to the hilus. There was no observed bleeding from the hilus or cyst bed.
VDO The effect of temporary uterine artery ligation with Endo clip on laparoscopic myomectomy to reduce intraoperative blood loss.
- Kezia Marsilina, Yuli Trisetiyono
Department of Obstetrics and Gynecology, Faculty of Medicine, Diponegoro University, Kariadi General Hospital, Semarang, Indonesia Introduction: A 31-year-old P2A0 woman came to the hospital with heavy menstrual bleeding, referred with a uterine myoma. She denied any weight loss or any changes in defecating and urinating. The transabdominal ultrasonography showed uterus with a spiral like pattern tumour measuring 4.6 × 2.65 cm, and a ring of fire was found. The patient underwent laparoscopic myomectomy where Endo clips were used to temporary ligate the uterine artery to reduce intraoperative blood loss.
Surgical Technique: An umbilical trocar and three lower abdomen trocars were placed in the abdomen. Two litters of CO2 gas was entered, and the abdominal and pelvic cavities were observed. The uterus was seen to be enlarged, with normal adnexae. The retroperitoneal trigonum (external iliac artery- infundibulo pelvic ligament- round ligament) was identified and opened. The uterine artery was identified guided by the obliterated umbilical artery, the latter is located at the distal end of hypogastric artery. The uterine artery is then clipped with titanium Endo clip. The same procedure is performed contralaterally. Myomectomy is then completed by dissecting the mass after opening the posterior wall of the uterus using a Harmonic scalpel. The reconstruction of the uterus was done using barbed sutures (v-lock), finally the fibroid is morcellated. The clips are then removed using a forceps. The total operation time is 50 minutes, total bleeding 50 cc, no active bleeding was seen. The incisions were closed layer by layer by sutures.
Conclusion: Temporary ligation of uterine artery using Endo clips is a simple technique and could be an option to reduce intraoperative blood loss volume on laparoscopic myomectomy. A uterine myoma enucleating by laparoscopy using Endo clips temporary artery ligation technique can reduce the operative time, lower risk of injury to the surrounding tissues and it is easy and quick to perform the application of the Endo clips on uterine artery.
Secondary Amenorrhea due to Female Genital Tuberculosis.
- Ritonga MA, Ismail M, Prasetyo NE, Parwati Ida, Djuwantono T. Reproductive and Endocrinology Fertility Division
Department of Obstetrics and Gynecology Faculty of Medicine Universitas Padjadjaran Bandung, West Java, Indonesia Objective: To Report a case of secondary amenorrhea related or caused by female genital tuberculosis and a minimal invasive surgery protocol for diagnosis and therapy.
Method: This is a video case presentation of 24 years old woman who experienced two years of infertility and three years of amenorrhea. The subject has also a history of abdominal tuberculosis 10 years before admission with incomplete tuberculosis therapy. Because there is a suspicion of recurrent abdominal tuberculosis, the Interferon Gamma (IGRA) examination was performed to exclude tuberculosis.
Results: Female genital tuberculosis is a secondary disease resulting from a primary tuberculosis Infection. The spread of tuberculosis can be hematogenous or lymphogenous. The disease itself is often hard to diagnose. The biomolecular testing also has a low sensitivity and specificity for the diagnosis of female genital tuberculosis. In the case at hand a diagnostic hysteroscopy and laparoscopy were performed. Surgical finding included a pale endometrium and intrauterine adhesions at hysteroscopy and at laparoscopy a Hugh-Fitz-Curtis syndrome and Sharma’s hanging gallbladder sign. The patient then had a bilateral salpingectomy and intrauterine adhesiolysis. Histopathological results did reveal endometrial tuberculosis and bilateral non-specific chronic salpingitis.
Conclusion: Thorough anamnesis and examination should be performed in diagnosing female genital tuberculosis because many variables are low in sensitivity and specificity.
Direct Insertion and Digital Dilation: A Novel Entry Technique in SILS.
- Herbert Situmorang 1, Yessy Adhi Utami 2, Vinanda Maria Alexandra Limbong 2
1Reproductive Health Division, Department of Obstetrics and Gynecology, Faculty of Medicine Universitas Indonesia,
2Dr. Cipto Mangunkusumo National Hospital Background: Since the introduction laparoscopy, Single Incision Laparoscopic Surgery (SILS) has gained its popularity as the least invasive treatment for gynecologic conditions. In recent times, a multichannel port is placed in the umbilicus for instrument access. This port is inserted using the open technique, where the multiple layers of abdominal wall are incised and dissected. Although open technique is commonly used for its safety, it requires many surgical instruments and takes a longer time than any other entry method.
Aim: This study aims to create a newer technique that overcome the complexity from previous entry techniques.
Method: This is a descriptive study with a video showing the Novel Entry Technique step-by-step.
Discussion: Our entry technique starts making a 15-20 mm skin-deep incision made at the inferior border of the umbilicus, extending laterally. A 12-mm trocar is then inserted through the direct entry method. After ensuring that the trocar has reached the peritoneal cavity, gas insufflation is performed to establish a pneumoperitoneum. The initial trocar is then removed whereafter a digital blunt dissection is performed. The multichannel port is then gently inserted in place. The time lapse from initial skin incision to port entry was approximately 4 to 6 minutes, utilizing a minimum of surgical equipment.
Conclusion: Compared to the conventional open technique, this method provides faster time from skin incision to port entry and requires less surgical instruments with a smaller incision site – making it a more efficient technique of multichannel port insertion.