Authors / metadata
DOI: 10.36205/trocar6.2025012
Abstract
Intestinal endometriosis, characterized by the presence of endometrium-like tissue in a segment of the intestine, can present with intestinal disturbances. This case report: describes a 39-year-old woman who underwent a step-by-step laparoscopic surgical intervention for deep endometriosis involving the ileum, cecum, and appendix, after presenting with chronic pelvic pain associated with intestinal disorders. A segmental ileocecoappendiceal resection with latero-lateral anastomosis was performed, with favorable postoperative follow-up. This case highlights the relevance of surgical intervention in an ileocecoappendiceal condition due to multiple nodules in a considerable intestinal segment. Results: Surgical time was 187 minutes, the patient showed progressive resolution of bowel symptoms and significant improvement in quality of life at sex-month follow-up. Conclusion: The reverse laparoscopic technique for ileocecoappendiceal endometriosis provides safe anatomical dissection in our experience, reduces intraoperative risks.
Learning objective
The objective of this article is to demonstrate the step-by-step surgical technique when there is ileocecoappendiceal involvement, using the reverse surgical technique, thereby improving neurovascular and functional compromise in a complex case of deep endometriosis (DE).
Introduction
Deep endometriosis (DE) is defined as the invasion of endometrium-like tissue into structures such as the intestine, bladder, and pelvic fascia. The #ENZIAN FI classification describes additional lesions outside the main compartments (A, B, C). The “I” refers to lesions in the intestine in different segments, which can cause anatomical distortion depending on the involvement by the endometriotic lesion, as well as diverse intestinal symptoms. Therefore, the surgical approach requires reducing neurovascular risks and surgical time. Intestinal endometriosis is defined as the condition caused by the presence of endometrial glands and stroma similar to the endometrium towards at least the muscularis propria layer of the intestinal wall (1). Regarding the involvement by nodules, this can cause total or partial stenosis, and symptoms can range from intestinal occlusion to sub-occlusion. The surgical management of nodules varies in relation to the intestinal involvement, with the most commonly used techniques being discoid resection and segmental resection (2).
Case report
The present case is a 39-year-old woman with chronic pelvic pain, dyspareunia and dyschezia, abdominal distension, diarrhea, and constipation. Magnetic Resonance Imaging (MRI) mapping showed: #ENZIAN v2021: P0, O3/0, T2/3, A1, B1/1, C0, FA FI. FI: A three cm nodule adherent and causing anatomical distortion of intestinal loops in the ileocolonic region without possible identification of the appendix, possible reduction of the intestinal lumen, adjacent fibrosis was identified.
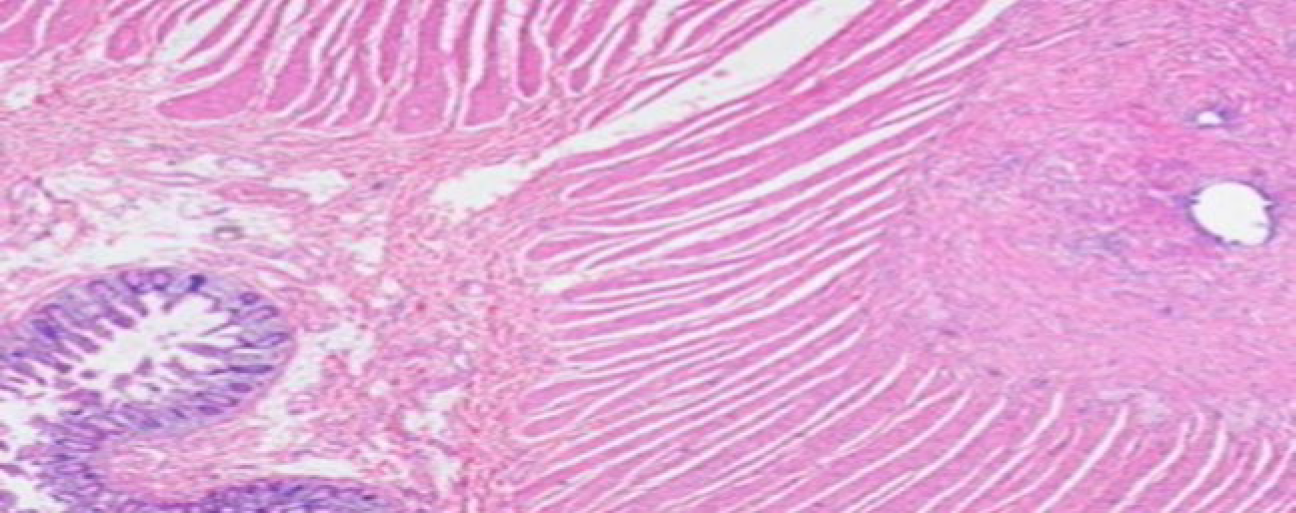
The present video article demonstrates the involvement of the ileocecal lesion and the step-by-step laparoscopic approach. Favorable postoperative evolution one month later with remission of intestinal symptoms. The pathology reported: in the small intestine, foci of endometrial glands with simple cuboidal epithelium. Cecal appendix: endometrial glands in the muscular wall.1 Ileum: lamina propria with foci of endometriosis.
The patient gave consent for scientific publication of this video, contributing to the scientific literature and surgical advancement.
Surgical Technique Step by Step
Under anesthesia, the patient in Lloyd Davies position. An open trans umbilical incision is made for the insertion of a 10 mm trocar, and pneumoperitoneum is established at 12 mmHg. Four 5 mm accessory trocars are placed in the right iliac fossa, suprapubic, left iliac fossa and paraumbilical. Using a 30-degree optical endoscope, a panoramic inspection of the abdominopelvic cavity is performed.
- First Step: Identifying the Lesion. Findings in the large bowel: Endometriotic nodules with rather firm adhesions on the descending colon, caecum, and appendix, all found clumped together.
- Second Step: Dissecting the Ascending Colon. The descending colon is first mobilized by dissecting the paramesocolic fascia right up to the hepatocolic ligament. Following this, the ascending colon is exposed, and some nodules are spotted a couple of centimeters away from the ileocecal valve. Preparations are made for a segmental resection of the affected part. The dissection of the mesocolon is done with advanced bipolar energy (a 5 mm Ligasure device). Keeping the mesocolon dissection to a mere 5 mm helps to minimize any interference with the collateral blood flow, which will make sure the edges of the planned anastomosis are adequately perfused.
- Third Step: Vascular Control and Ligation. The anterior ileocolic branch is tied off using a size 1 Vicryl suture. Once it is ensured there is no bleeding (haemostasia confirmed), the distal vessels are snipped using advanced bipolar energy. And then it is mobilized for exteriorization of the bowel.
- Fourth Step: Exteriorization of the Bowel. The suprapubic port is was enlarged, and a flexible Alexis retractor is inserted. The segment of bowel with the endometriosis nodules is then brought extracorporeally.
- Fifth Step: Segmental Resection. A segmental resection is performed outside the body (extracorporeally), which includes the terminal ileum, the caecum, and the appendix.
- Sixth Step: Anastomosis. A side-to-side anastomosis of about 2.5 mm is made using a 60 mm linear stapler, and a pneumatic test is done to make sure the anastomosis is sound.
Discussion
Bowel endometriosis occurs in about 12% to 15% of cases, and how often different bits of the bowel are affected varies in the medical literature. It’s reported that the rectosigmoid colon (the bottom bit of the large intestine), the small intestine, the appendix, and the caecum are affected in roughly 50% to 90%, 2% to 16%, 3% to 18%, and 2% to 5% of cases respectively (4,5).
The step-by-step surgical technique demonstrated offers advantages in the management of endometriosis with ileocecoappendiceal involvement for surgeons performing endometriosis surgery, being reproducible with the learning curve. Regarding the reverse versus conventional technique, in our experience, it reduces potential damage to neurovascular structures compromised by the disease and also improves surgical visualization by delineating the depth and extent of the lesion, thereby increasing the surgical safety for the surgeon and the team. For a long time, the conventional surgical approach started with the lesion, which was reported to cause damage to the adjacent structures due to the anatomical distortion that occurs in endometriosis. (6,7,8,9,10).
The involvement of the ileocecal portion due to the anatomical relationship with the pelvis and the abdominal cavity are frequent findings; however, rectal involvement is greater than ileocecal involvement. Studies describe that these regions of the intestine are affected by the neuro-vasculature and irrigation; however, this remains more of a theory. The preoperative clinical presentation guides us to intestinal involvement, as the endometriosis mapping is operator-dependent; the intestinal part, due to the distance and partial obstruction, was not visible on the study (13,14). There are few reports of ileocecal endometriosis; some reports exist due to the fact that colon carcinoma was suspected because of the diffuse clinical presentation of intestinal obstruction, and the pathology report demonstrated endometriosis (3). The segmental ileo-cecoappendiceal resection performed is mostly done in lesions of large circumference or when there are multiple endometriotic nodules in the same segment of the intestine, as in our case among other possible option is the NOSE (Natural Orifice Specimen Extraction) technique; however, due to the distal location of the nodule in the present case, it was not accessible for NOSE (11). In the case at hand due to the location, the exteriorization of the specimen by expanding the suprapubic trocar is the better method for performing the anastomosis. The reverse technique described step-by-step, addressing the lesion from healthy tissue, is performed to avoid neurovascular compromise caused by endometriosis nodules, in addition to leaving adjacent tissues free of tension. (5) The surgical approach used in this case, compared to single-incision laparoscopic surgery, offers significant advantages such as reduced postoperative pain at the incision site, which does not exceed eight centimeters. Furthermore, the use of 12 mm ports allows for a minimally invasive access while preserving the aesthetic and functional benefits inherent to laparoscopy (12).
The preoperative assessment of intestinal involvement by endometriosis uses magnetic resonance imaging as a second-line alternative. Among the less common involvements, one- third of cases involve the cecum, appendix, and small intestine. There is a recommendation to use MRI as a triage test in the diagnosis of rectosigmoid colon endometriosis (14). In the portion of small intestine, the cecum, and the appendix that was examined, there were collections of immune cells (lymphoid aggregates). It therefore showed spots of endometrial glands, which are made up of simple, cube-shaped cells, surrounded by spindle-shaped cells with a bluish cytoplasm (Fig 1, Fig 2) Macroscopic piece image showing a nodule in the ileum, appendix, and caecum.
The impact of this surgical technique, compared to those previously described, remains uncertain due to the limited number of studies available for objective comparison. Nevertheless, excision of the nodule in proximity to the ileocecal valve within a single surgical session, as opposed to techniques involving osteomas or staged procedures, appears to offer greater advantages for the patient. However, these benefits are largely dependent on the surgeon’s level of experience, with an inverse relationship between surgical risk and surgical expertise. Functional outcomes are comparable across the different techniques. It is worth noting that, in terms of recurrence, a higher rate has been documented following shaving procedures compared to discoid excision or segmental resection. (15)
Results
Among the main results offered by this surgical technique are the preservation of critical anatomical structures and the resolution of intestinal symptoms. As well as step-by-step teaching of the surgical technique to improve the learning curve of pelvic surgeons who are starting. The surgical time was 187 minutes, during which intraoperative risks were reduced, as well as exposure to anaesthetic risks. Postoperative follow-up was carried out for up to six months after the procedure. At the Doyenne Institute, we follow a structured protocol that includes standardized questionnaires, laboratory tests, and weekly and monthly clinical assessments, which progressively evaluate the improvement of postoperative pain and the evolution of symptoms present prior to surgery. The patient showed progressive improvement; however, during the initial months following the intervention, she experienced recurrent episodes of diarrhea. Thanks to a comprehensive approach that included nutritional support and pelvic floor rehabilitation, the patient’s quality of life improved significantly by the six-month mark.
Video
Conclusion
In our experience, laparoscopic surgical management of endometriosis involving multiple organs is safe. However, we emphasize the importance of the surgical team’s expertise in order to minimize the risk of neurovascular injury and to optimize operative time.