Authors / metadata
DOI: 10.36205/trocar6.vid25015
Abstract
Introduction: Isthmocele, a Cesarean scar defect, represents an anechoic pouch-like indentation at the lower uterine segment, often associated with abnormal uterine bleeding, pelvic pain, and secondary infertility. Hysteroscopic repair is the preferred approach for symptomatic women with adequate residual myometrial thickness (RMT). However, bladder perforation (2%) is a known but rare complication, particularly in cases with dense vesicouterine adhesions.
Case: A 38-year-old woman with previous two cesarean deliveries and a failed laparoscopic isthmocele repair presented with irregular bleeding. Transvaginal ultrasound revealed a 6 × 7.8 × 6 mm triangular niche with an RMT of 5.9 mm. During hysteroscopic resection of fibrotic tissue, a 2–3 mm posterior bladder wall perforation occurred due to dense adhesions. Immediate laparoscopic conversion was performed, with adhesiolysis, double-layer bladder repair, and omental interposition.
Outcome: The postoperative course was uneventful. Follow-up imaging confirmed complete uterine contour restoration and bladder healing. The patient remained asymptomatic and was scheduled for assisted reproduction.
Conclusion: Bladder injury is a recognized complication of hysteroscopic isthmocele repair, particularly in large or bladder-adherent niches. Careful intraoperative vigilance, prompt recognition, and timely laparoscopic management with omental interposition are critical to achieving optimal outcomes. A multidisciplinary and individualized approach ensures anatomical restoration, prevents recurrence, and preserves fertility potential.
Introduction
An isthmocele, also termed a Cesarean scar defect or niche, represents an anechoic, pouch-like indentation at the site of a previous Cesarean section, typically located in the lower uterine segment. The most widely accepted sonographic definition describes it as a triangular or semicircular defect with a depth of ≥2 mm at the Cesarean scar site (1). The reported prevalence of isthmocele varies widely between 19% and 88%, depending on diagnostic criteria, imaging modality, and the number of prior Cesarean deliveries (1–3). Approximately one-third to half of affected women develop symptoms, most commonly postmenstrual spotting, chronic pelvic pain, dyspareunia, and secondary infertility due to intracavitary fluid accumulation interfering with implantation (2,3). Several factors contribute to the development of the isthmocele, including incomplete myometrial healing, excessive incision width, low uterine incision, and technical aspects of uterine closure (1,4). Recognition of this entity has increased with routine use of transvaginal ultrasound (TVS) and saline infusion sonohysterography, which improve diagnostic accuracy (1). Management is determined by symptom severity, reproductive plans, and residual myometrial thickness (RMT). Hysteroscopic repair is generally recommended for symptomatic women with an RMT ≥2.5–3 mm, whereas laparoscopic or vaginal repair is preferred when the myometrial thickness is less than 2.5 mm or in the presence of extensive adhesions (1,4,5). Surgical correction aims to restore normal uterine anatomy, improve bleeding symptoms, and enhance fertility outcomes Despite its safety, bladder perforation (+/- 2%) remains a rare but serious complication (2). We present this case to highlight the importance of prompt recognition and effective management of this complication, which, to the best of our knowledge, is the first of its kind reported in the literature.
Case report
A 38-year-old woman (G2P2) with two previous Cesarean sections presented with irregular uterine bleeding and discharge per vaginam. She underwent a previous laparoscopic repair of isthmocele (failed) with myomectomy. She was desirous of conception and was unable to conceive on her own. She had a failed IVF in the past and was awaiting next embryo transfer. There was no other relevant medical or surgical history.
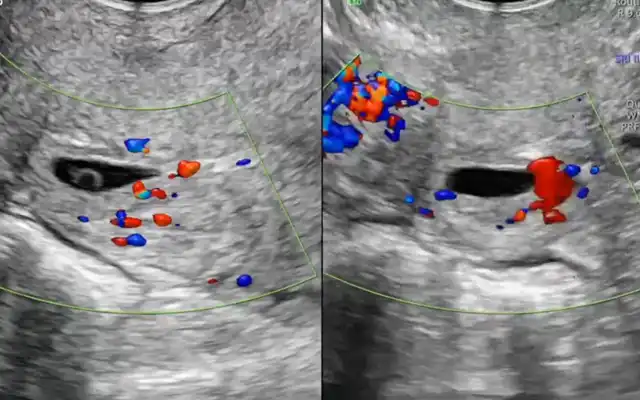
Ultrasound Findings:
Transvaginal ultrasound (October 2024) revealed a triangular anechoic niche measuring 6 × 7.8 × 6 mm, located 30 mm above the external os, with a residual myometrial thickness of 5.9 mm (53% of adjacent myometrium). The right ovary was adherent to the uterus; the left ovary contained a simple follicular cyst. Mild adenomyosis was noted in the fundus.
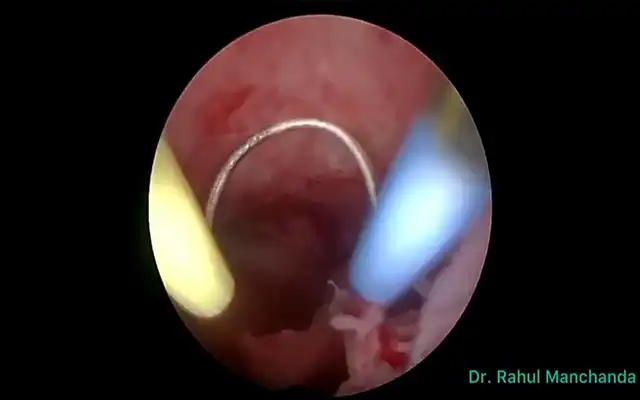
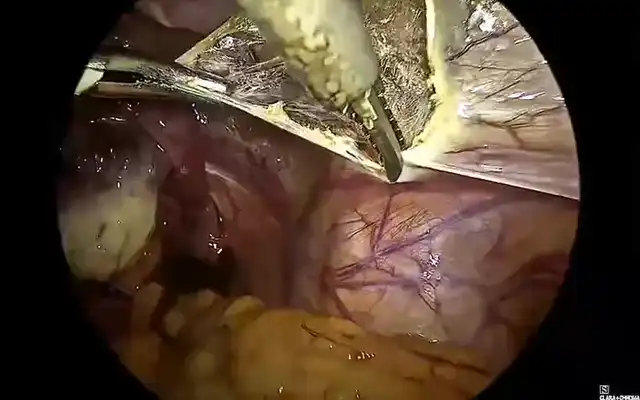
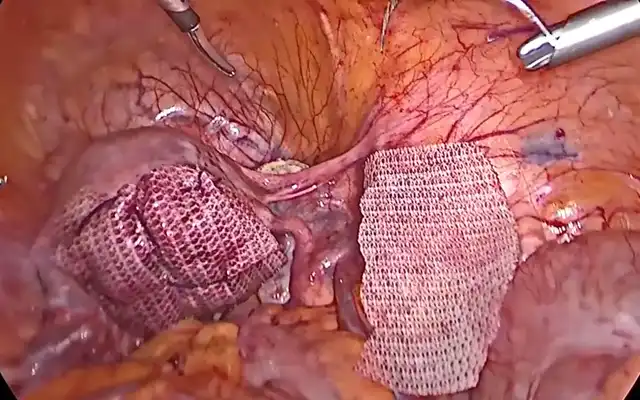
Operative Details:
Under general anesthesia, diagnostic hysteroscopy confirmed a large anterior niche. During resection of fibrotic tissue, a 2–3 mm perforation occurred into the posterior bladder wall. Cystoscopy was immediately performed, confirming the bladder defect. A ureteric stent was gently passed through the defect and was visualized traversing the isthmocele and exiting through the cervical canal, thereby delineating the tract of perforation. Laparoscopy was subsequently undertaken, using the stent as a guide to precisely localize the site of injury—an effort similar to finding a needle in a haystack. Dense vesicouterine adhesions were carefully lysed, freeing the bladder from the cervix and lower uterine segment. The bladder defect was then repaired in two layers with interrupted sutures, and an omental flap was interposed between the bladder and uterus to prevent recurrence and re-adhesion. Final cystoscopic inspection confirmed watertight closure and bilateral ureteric efflux.
Outcome:
Hemostasis was achieved, and the postoperative course was uneventful. A Foley catheter was retained for 10 days. Follow-up ultrasound demonstrated complete restoration of uterine contour and no residual niche. The residual myometrial thickness at point of the lower segment Cesarean scar was 4.8 mm. The patient was asymptomatic on subsequent follow up and was planned for assisted reproduction therapy.
Discussion
Surgical correction of an isthmocele has been shown to relieve symptoms, improve endometrial receptivity, and enhance fertility potential (6,7). The choice of the surgical route depends primarily on RMT and the extent of the bladder adhesion. Hysteroscopic resection offers excellent results in cases with adequate myometrial thickness (≥3 mm) by removing the fibrotic ridge and restoring normal uterine outflow (8). However, in cases with thin residual myometrium (<3 mm) or where the bladder is closely adherent, laparoscopic or combined repair is considered safer and more effective (7). In this case, hysteroscopic resection led to a 2–3 mm bladder perforation due to dense vesicouterine adhesions and close proximity of the niche to the bladder wall – an uncommon but recognized complication. Bladder injury, though uncommon, remains a notable risk during hysteroscopic isthmocele correction, especially with distorted anatomy from prior Cesarean sections (5,10). A systematic review reported bladder lacerations and perforations during laparoscopic isthmocele repairs in isolated cases, often related to severe adhesions or inadvertent extension during dissection (5). Early recognition, immediate laparoscopic conversion, and primary repair with double-layer suturing, as performed in this case, are the recommended management steps (9,10). The use of an omental interposition flap further prevents postoperative adhesion formation and fistula development (9). Postoperative follow-up with transvaginal ultrasound is essential to confirm anatomical restoration and adequate RMT before resuming fertility treatments. Expert consensus recommends delaying conception for at least 3 months post-repair and advocate for elective Cesarean delivery at 37–38 weeks in subsequent pregnancies to prevent scar rupture (1,4,11). This case underscores the importance of careful preoperative planning, intraoperative vigilance, and a multidisciplinary approach in managing complex isthmocele cases. Awareness of possible complications and readiness for prompt surgical conversion are vital for optimal outcomes.
Video
Conclusion
Bladder perforation is a recognized complication of hysteroscopic isthmocele repair, particularly in cases with dense vesicouterine adhesions or large anterior defects. This case highlights the importance of careful intraoperative vigilance, prompt recognition of injury, and timely surgical management to prevent morbidity and preserve fertility. Meticulous bladder repair and omental interposition ensure optimal healing and anatomical restoration. An individualized, multidisciplinary approach guided by preoperative assessment and surgical expertise remains essential for achieving favorable reproductive and functional outcomes in women undergoing isthmocele repair.