Authors / metadata
DOI: 10.36205/trocar6.2025023
Abstract
Obstetric haemorrhage remains a leading cause of maternal morbidity and mortality worldwide. Selective ligation of the hypogastric (internal iliac) artery is an established surgical option for pelvic haemorrhage control, with the potential to preserve the uterus and ongoing pregnancy. Laparoscopic approaches offer additional benefits in terms of reduced invasiveness and faster recovery. The case of a 40-year- old woman, gravida 4 para 3, at 17.2 weeks of gestation, admitted with profuse vaginal bleeding and signs of hypovolemic shock secondary to spontaneous bleeding from a cervical mass under investigation is reported. Emergency laparoscopic surgery was performed with selective ligation of the right hypogastric artery. The anterior division was identified and ligated with 4-0 chromic suture, achieving haemostasis without complications. Literature supports the use of hypogastric artery ligation for severe obstetric bleeding, whether postpartum or during pregnancy, showing efficacy in reducing blood loss and avoiding more radical procedures. Laparoscopic selective hypogastric artery ligation is a safe and effective option for managing complex obstetric haemorrhage during pregnancy. In experienced hands, it allows rapid haemostatic control, preservation of pregnancy, and minimizes surgical morbidity, representing a valuable tool in conservative obstetric surgery.
Introduction
Internal iliac (hypogastric) artery ligation is a vital surgical procedure for the control of severe obstetric and gynecological haemorrhage. Although less invasive alternatives, such as selective arterial embolization or temporary balloon occlusion, are currently available, these options present limitations related to resource availability, the need for specialized personnel, and the time required for implementation, which restricts their usefulness in scenarios of massive and unexpected haemorrhage. In this context, several studies have indicated that the prophylactic application of hypogastric ligation during high-risk procedures, such as hysterectomy for placenta accreta, can significantly reduce blood loss and the need for transfusions without increasing complications. A retrospective study conducted in Turkey evaluated the effect of prophylactic ligation of the hypogastric arteries in patients with placenta accreta undergoing hysterectomy. The results showed that this technique significantly reduced intraoperative bleeding, postoperative drainage, and transfusion requirements, without increasing the complication rate or mortality (1). A randomized clinical trial evaluated the efficacy of prophylactic hypogastric (internal iliac artery) ligation before Cesarean hysterectomy in 64 women with abnormal bleeding per partum. Patients who underwent hypogastric ligation had less intraoperative blood loss, less visceral trauma, and reduced surgical and hospital stay times (2). Kostov et al. (2024) review in detail the surgical anatomy of the internal iliac artery, its pelvic anastomoses, and the step-by-step ligation technique, highlighting its therapeutic and prophylactic role in situations such as placenta accreta, uterine rupture, cervical lesions, or bleeding due to advanced gynecological cancer (3). Prajapati et al. (2022) present a retrospective review of 58 cases treated at a tertiary hospital in India over a 20-year period. 53 of these cases were for obstetric reasons and 5 for gynecological reasons. The procedure did control bleeding in 90% of cases of atonic per partum haemorrhages, avoiding hysterectomy in most cases and allowing subsequent pregnancies in 27.3% of women. Complications were rare, including febrile morbidity (6.9%) and superficial vascular lesions (1.7%) (4). Chou et al. (2002) reported the first documented case of laparoscopic uterine artery ligation using bipolar coagulation to treat delayed postpartum haemorrhage secondary to placental remnants. The procedure effectively controlled bleeding, reduced hospital stays, avoided hysterectomy, and preserved reproductive function, supporting the potential of laparoscopic techniques as safe, minimally invasive alternatives in selected cases (5). A case report of a 29-year-old woman describes how, three days after an uncomplicated vaginal delivery, she presented with massive hemoperitoneum of no apparent cause. Laparoscopic examination identified bleeding from the left uterine artery, which was controlled by laparoscopic ligation of the internal iliac artery. This case highlights the importance of timely diagnosis and treatment and suggests that laparoscopy is a feasible and minimally invasive option for managing this condition, promoting a faster recovery (6). Although open hypogastric artery ligation has been widely used for severe obstetric haemorrhage – including placenta accreta, uterine rupture, and traumatic cervical injuries – and there are isolated reports of laparoscopic approaches to uterine artery ligation for bleeding control, no documented cases of laparoscopic hypogastric artery ligation to treat spontaneous haemorrhage secondary to a cervical mass in a pregnant patient have been identified in the literature. This fact gives this case report unique value, as it provides evidence of the feasibility and efficacy of a minimally invasive approach in an exceptional clinical situation, where bleeding was controlled, uterine integrity was preserved, and major complications were avoided. To date, no reports have been found in the literature on laparoscopic ligation of the hypogastric artery during pregnancy, which emphasizes the novelty and relevance of the present case.
Case report
The case of a 40-year-old woman, Gravida 4, Para 3, with a 17.2-week pregnancy, under follow-up for a cervical tumor is reported. No significant pathological, surgical, nor obstetric personal history. She presented to the emergency department due to abundant transvaginal bleeding, accompanied by clinical signs of hypovolemia. On physical examination, active bleeding from the cervical mass was confirmed (Figure 1). Given the magnitude of the bleeding and her hemodynamic condition, an urgent surgical intervention was decided for selective vascular control.
Under general anesthesia, laparoscopic approach was initiated. Abdominal insufflation was performed through the insertion of a Veress needle at Palmer ‘s point (Figure 2), followed by the placement of an umbilical trocar as the main port and two accessory trocars.
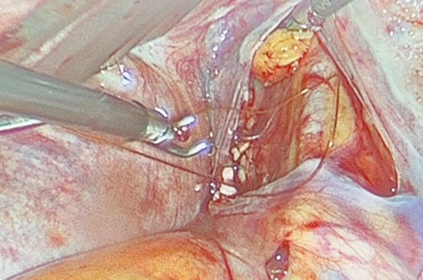
During the exploration, the right hypogastric artery was identified, locating its anterior division. Ligature was performed with 4-0 chromic suture, with no intraoperative incidents or associated injuries (Figure 3). The total estimated blood loss was 50 ml. Prior to the procedure, the fetal heart rate was 130 beats per minute; at the end, it was recorded at 140 beats per minute. The patient was transferred to the recovery area with stable vital signs, no active bleeding, and adequate peripheral perfusion.
Discussion
In the presented case, a 40-year-old female patient, G4P3, at 17.2 weeks’ gestation and with a cervical mass under investigation, was admitted with profuse vaginal bleeding and signs of hypovolemia. Haemostatic control was achieved with selective laparoscopic ligation of the right hypogastric artery, resulting in minimal blood loss and preservation of the pregnancy, with no intraoperative complications. The pregnancy ended in a successful delivery at 38 weeks without complications, and the cervical mass was ultimately diagnosed as a cervical polyp. The available evidence supports hypogastric artery ligation as an effective procedure for the management of severe obstetric haemorrhage, as it preserves the uterus and, in many cases, preserves fertility. However, Tokgöz Çakır et al. (2024) identified that, although this technique does not increase the risk of spontaneous abortion or compromise reproductive capacity, it may be associated with a higher rate of premature birth and low neonatal weight in subsequent pregnancies, which underlines the need for close obstetric follow-up in patients with a history of this procedure, even when performed unilaterally and during ongoing pregnancy (7). Regarding alternatives, several conservative strategies have been described. Paredes-Contreras et al. (2023) reported a case of increased myometrial vascularity in pregnancy treated with bilateral laparoscopic temporary ligation of the uterine arteries, followed by uterine aspiration, which allowed effective control of bleeding, preservation of the uterus, and recovery of vascularisation of the uterus . This option is presented as a useful alternative when embolization is not possible and the objective is to maintain reproductive potential (8). Similarly, Bai et al. (2023) evaluated the efficacy of uterine and internal iliac artery ligation in 199 patients with placenta previa, finding that prophylactic ligation of the internal iliac artery significantly reduced intraoperative bleeding, transfusion needs, and ICU admission rate compared to therapeutic ligation. Furthermore, uterine artery ligation was associated with a lower hysterectomy rate and shorter surgical times, particularly in cases without deep placental invasion. The authors conclude that the choice of technique should be individualized according to the degree of placental invasion and the experience of the surgical team, prioritizing uterine ligation in less invasive scenarios and internal iliac ligation in cases of penetrating implants or bladder invasion (9). Likewise, previous reports reinforce the relevance of this type of approach. Pezzuto et al. (2009) described a spontaneous hemoperitoneum at 15 weeks of gestation, successfully treated laparoscopically in a 40- year-old patient (10). The bleeding, originating from uterine vessels of the broad ligament, was controlled with diathermic coagulation, achieving evacuation of 4.5 L of blood and preserving the pregnancy, which culminated in a Cesarean delivery of a healthy newborn at 38 weeks. This report shares similarities with the current case, in which severe obstetric bleeding in the second trimester was treated with selective laparoscopic ligation of the hypogastric artery, achieving effective haemostatic control and preserving the pregnancy. Both cases reinforce the idea that, in expert hands, laparoscopy represents a safe and effective tool for the management of severe pelvic haemorrhage in early or intermediate stages of pregnancy, avoiding more invasive procedures and improving the maternal-fetal prognosis.
Conclusion
Laparoscopic hypogastric artery ligation during pregnancy represents an innovative surgical alternative for the management of severe obstetric haemorrhage. In the case presented, this technique allowed effective haemorrhage control with minimal blood loss, a low risk of complications, and preservation of pregnancy, demonstrating its feasibility and safety in expert hands. Unlike other procedures such as selective arterial embolization or balloon occlusion, whose availability and applicability may be limited in emergency settings, the laparoscopic approach offers additional advantages by being minimally invasive, promoting faster recovery, and reducing postoperative morbidity. The absence of previous reports in the literature on the performance of this procedure during pregnancy underscores the uniqueness of this case and reinforces the need for future studies and clinical series to support its efficacy, safety, and applicability in different obstetric settings.