Authors / metadata
DOI: 10.36205/trocar6.2025024
Abstract
Heterotopic pregnancy (HP) is a rare form of pregnancy, defined by the coexistence of an ectopic and an intrauterine pregnancy as described by Reece et al in 1983 in a review of 589 cases, and is extremely rare (1). The diagnosis of heterotopic pregnancy remains one of the greatest challenges of the gynecological- obstetrical emergencies. HP is the coexistence of living or dead intrauterine pregnancy, single or multiple, and extrauterine pregnancy located in the fallopian tube, ovary, uterine cornu, cervix or peritoneal cavity. This condition is very rare (1:30000 pregnancies). Its occurrence after natural conception is scarcely documented in the literature. The case of a spontaneous HP in a 27 years old patient is presented with resolution of the ovarian pregnancy ending in a Cesarean delivery of the intrauterine twin pregnancy at term.
Key message: Heterotopic pregnancy can occur in natural conception irrespective of usage of ovulation induction. Routine early pregnancy ultrasound can promote early detection with prompt surgical intervention to mitigate its complications.
Introduction
Case Presentation:
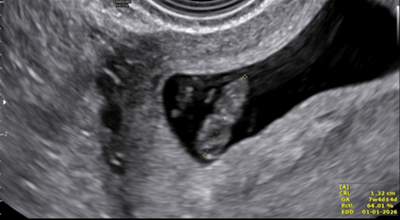
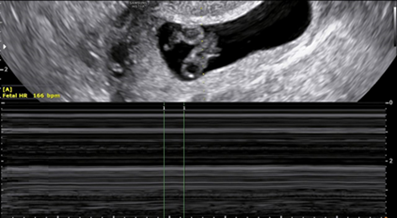
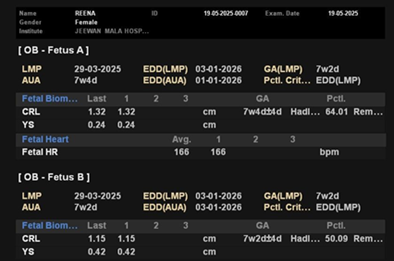
The case of a 27-year-old primiparous women who presented at 7 weeks with features of hyperemesis in a routine pregnancy follow up is presented. No previous ultrasonographic imaging was done. Current ultrasound scan showed a twin live intrauterine pregnancy with thick separating membrane giving a lambda sign. Crown Rump Length (CRL) of fetus A measured 1.32 mm with Fetal Heart Rate (FHR) at 166 Beats Per Minute (BPM) and the CRL of fetus B was 1.15 mm with FHR 154 BPM. It also showed a gestational sac with a fetal pole with CRL 10 mm in the right ovary complicated by a surrounding peri-ovarian hematoma forming a right adnexal mass measuring 57×35 mm. No cardiac activity was seen in this fetal pole (Figure 1 A/B).
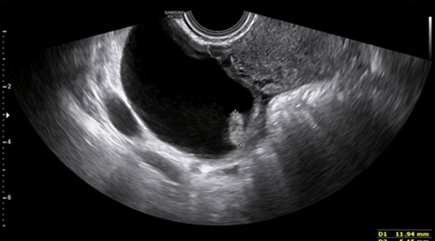
The left ovary showed a corpus luteal cyst (Figure 3). The findings were consistent with a twin intrauterine live dichorionic diamniotic pregnancy and a right ovarian pregnancy without cardiac activity.
On performing a physical examination her vitals were stable and no significant findings were noted except for an enlarged uterus corresponding to seven weeks pregnancy with right posterior forniceal fullness. Her beta-hCG performed at 4.5 weeks gestation was 3535 IU/ml. Since the patient had a normal intrauterine twin pregnancy and no fetal cardiac activity in the right ovarian gestation, the patient was kept under close follow up. There was a resolution of the right adnexal ovarian gestation with shrinkage of the cystic mass size to 30 mm and resolution of the peri-ovarian hematoma. She was later followed up to term and successfully delivered by elective Caesarean section.
A brief narrative of the challenges in the management, clinical presentation and limitation in the management is highlighted in the present case report. The diagnosis is possible only in cases when there is a high index of suspicion by the treating clinician. The adnexa must be inspected carefully in the confirmatory ultrasound. The early timely diagnosis gives a good maternal outcome and hence is crucial in the management.
Discussion
Heterotopic pregnancy (HP) refers to a dual coexistence of both extra-uterine and intrauterine pregnancy. It represents an extremely rare obstetric condition with distinct documented clinical presentations and complications. The documented occurrence rates are estimated to be 1 to 30000 deliveries with high occurrence (1 in 100) in women undergoing assisted reproductive techniques ART (2,3). The majority of the documented reports in the literature are ART-related cases with natural conceived HP reports being virtually non-existent (4–6). The presentation of ruptured HP constitutes a clinical challenge in diagnosis and optimal management. Its presentation in resource constrained setting poses additional intricacy in diagnosis, given the unavailability of high-resolution imaging and expertise to offer timely diagnosis and management. The most common site for ectopic in HP is ampullary similar to the isolated ectopic pregnancy. The clinical symptoms do vary: early first trimester abdominal pain, vaginal bleeding that occasionally results in abortion, which has been reported in the literature (5). A considerable proportion (60–70%) of the HP may proceed to term and deliver normally. Delayed diagnosis may result in significant maternal and fetal morbidity that can be fatal if unattended timely. Reece et al reported the condition first and it included cases conceived spontaneously (1). The condition is extremely rare. But in the millennium years with considerable development of infertility treatment, the incidence is showing a rising trend. The major risk factors for heterotopic pregnancy are chronic pelvic inflammatory disease, use of intrauterine disease, previous history of ectopic, previous tubal surgeries, assisted reproductive techniques. The causes attributed to an independent ectopic gestation are also considered as a risk factor for heterotopic pregnancy. The most frequent location are the fallopian tubes followed by the ovaries. There are many more case reports to show the locations in the cervix, the peritoneal cavity and the uterine cornua. There are also reported cases of tubal ectopic associated with pathological intrauterine pregnancy like blighted ovum or early intrauterine demise. Many case reports and studies have thrown light on this topic. But more systematic reviews are required to follow definite consensus for management. The transvaginal ultrasound for confirmation of pregnancy around 4-6 weeks period of gestation is the best tool for diagnosis. The adnexa should be imaged in the early ultrasound. The quantitative serum beta hCG values are the prime tool for managing an ectopic pregnancy as diagnostic and post treatment response indicator. But in case of an HP the beta hCG values cannot be trusted for diagnosis as there is presence of a viable intrauterine pregnancy. The monitoring of beta hCG post conservative measures also proves difficult in this case. The many conservative measures described by various authors are local methotrexate injection (a minimal of systemic absorption is noted as risk to the developing intrauterine fetus), local KCl injection (resulted in hematosalpinx), placing hemostatic sutures, prostaglandins (causes teratogenicity). Many other studies support conservative management with favorable outcomes.
Conclusion
The diagnosis is possible only in cases when there is a high index of suspicion by the treating clinician. The clinical presentation is like that of an ectopic pregnancy where the patient presents with abdominal pain and bleeding per vaginam. The adnexa must be inspected carefully in the confirmatory ultrasound. The early timely diagnosis gives a good maternal outcome and hence crucial in the management.
Acknowledgements: The authors thank Bruno J van Herendael for his positive criticism and help during the writing.