Authors / metadata
DOI: 10.36205/trocar4.2022001
Abstract
Laparoscopic surgery has a significant role in surgical management of early gynecological cancers (ovarian, cervical and endometrial cancer). Laparoscopic surgery is associated with well known advantages over open surgery (less blood loss, shorter hospital stay, quicker recovery, less post operative complications). Regarding oncological outcomes, overall survival (OS), and disease-free survival (DFS) further randomized trials are required to confirm that these two surgical techniques have similar outcomes. Until that data are available, laparoscopic surgery in treating gynecological malignancies should be used with caution. Adequate training and equipment are paramount. Patients should be carefully selected. Results collected and audited, and patients properly counselled and consented. In this article we review published data on application, safety and results of laparoscopic surgery in the gynae-oncology field.
Introduction
Since the introduction of laparoscopic surgery in clinical practice during the 1980’s, the number of different operations and indications for laparoscopic surgery in gynecological oncology has been increasing steadily. This increase was driven by technological advances in the field of endoscopic surgery, the developing experience of individual surgeons and patient demands for shorter hospital stays, quicker recovery, and a better aesthetic result. In this article we critically appraise published results and make recommendations based upon the available evidence. We will address the application of laparoscopic surgery to the treatment of ovarian, cervical, and endometrial cancer.
Ovarian Cancer
Ovarian carcinoma is in some countries the most common malignant tumor in gynecology in the developed world (1). It is the most lethal gynecological malignancy with an overall survival of 46% (2,3)(3) and with a 5 year survival in advanced stage of between 30-40% (4). The main reason for the poor survival is that the majority of patients (70-80%) present with stage III or IV disease (5,6) because early-stage disease is essentially asymptomatic.
Laparoscopy in stage I ovarian carcinoma
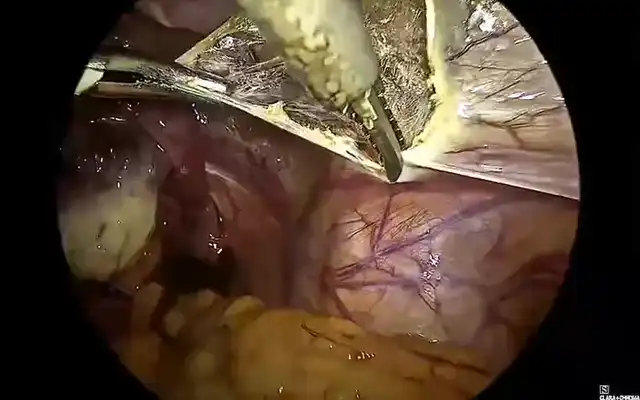
If a cancer is presumed to be stage I on imaging, the first line of treatment is surgery. This involves aspiration of ascites/peritoneal washings for cytology, hysterectomy with bilateral salpingo-oophorectomy, omentectomy, +/- pelvic and para-aortic lymphadenectomy (not universally recommended practice) (7,8) and biopsy of any suspicious areas for complete staging. Frozen sections during the operation are utilized in many centers for the intraoperative diagnosis of ovarian cancer. The importance of comprehensive staging is that patients with stage IA and IB, grade 1 and 2 tumors may avoid adjuvant chemotherapy, as there is no proven survival benefit (9). In grade 3 cancers adjuvant chemotherapy is recommended, hence the value of pelvic/para-aortic lymphadenectomy to select patients for adjuvant treatment is limited. For many decades the main approach for this surgery was by midline laparotomy. Conservative surgery can be considered in exceptional circumstances, in young patients with unilateral truly stage I ovarian carcinoma, who wish to preserve fertility or ovarian hormonal function.
During the 1990’s and the beginning of the 21st century a number of articles were published reporting surgical staging of stage I ovarian carcinoma utilizing a laparoscopic approach (7,10–14). Most studies reporting on the results of laparoscopic treatment of early ovarian carcinoma concluded that laparoscopic staging is a safe and technically feasible procedure (15–17). A significant number of cases were re-staging procedures as the diagnosis of ovarian carcinoma was only established from histology of the original oophorectomy or cystectomy. The original surgery was often performed by a non-gynecological oncology surgeon.
The laparoscopic approach has all the advantages of reduced blood loss; faster recovery and shorter hospital stay; fewer post-operative complications; better visualization of tumor deposits; better aesthetic results and a quicker start to post-operative chemotherapy, when indicated. However, laparoscopy has been associated with a higher rate of intraoperative tumor rupture which may result in upstaging (18,19). It has been proposed that performance of para-aortic lymphadenectomy might be technically difficult in some patients and that operative time is longer as compared to laparotomy. Other potential considerations are of port site metastasis and the theory that CO2 lowers abdominal pH and activates enzymes which increase tumor cell mitoses and growth factors, potentially promoting metastasis (20,21).
Large systematic reviews (22–25) have identified more than 1000 records relating to this topic but after scrutinizing the sources the authors found no more than 11 studies which were eligible for meta-analysis. Furthermore, none of the studies were randomized, which introduces a high level of bias and patient selection.
Considering the published data and conclusions of the meta-analyses, the consensus is that laparoscopic management and staging of stage I ovarian carcinoma is feasible, but because of the lack of grade I evidence most national guidelines still recommend surgical management and staging to be performed via laparotomy (8). The German Gynaecological Oncology Group has included the laparoscopic procedure as an option in their guidelines. The caveat is that this approach is reserved for selected patients (with minimal risk of cyst rupture) and the surgery is to be performed by expert laparoscopic oncology surgeons (26). Overall survival (OS) and disease-free survival (DFS) data in published studies, comparing laparoscopy versus laparotomy for stage I ovarian carcinoma, are extremely limited and no clear evidence exist that survival data are either equivalent or in favor of a laparoscopic approach. However, some meta-analyses (23–25)concluded that no difference was observedbetween the two approaches in terms of overallsurvival (OS) and progression-free survival (PFS),but these were based on non-randomizedstudies.
There is no doubt that further high-quality studies, in particularly large, randomized trials, are required to give a clear answer to this question. In the meantime, laparoscopic management/restaging of stage I ovarian cancer should be limited to carefully selected patients and should be performed by expert laparoscopic oncology surgeons, without cyst spillage and with the specimen retrieved in a bag.
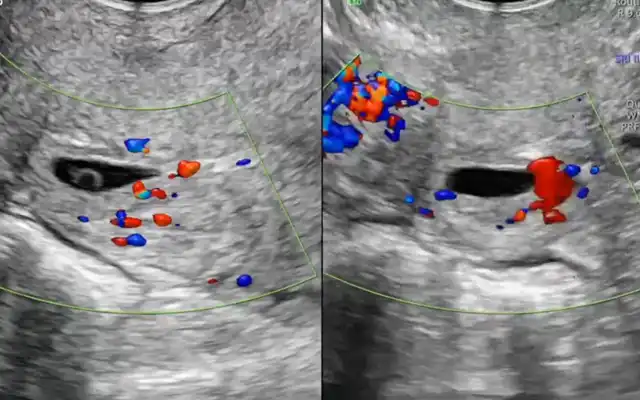
Laparoscopic assessment of operability for advanced ovarian carcinoma
The presence of residual disease after primary surgery for advanced ovarian cancer is a significant adverse prognostic factor. The aim of primary debulking surgery is to remove disease completely, leaving no visible disease after surgery. Some authors use a cut-off figure of <1cm of residual disease to define optimal surgical debulking. Depending upon reported results, up to 60% of the patients are left with disease up to 1cm and these patients would likely have benefitted from neoadjuvant chemotherapy (NACT) prior to debulking surgery. It is important to identify the subset of patients who would do better with NACT followed by surgery. Imaging techniques, including ultrasound (US), computerized tomography (CT), magnetic resonance imaging (MRI) and positron emission tomography (PET) do not have a satisfactory sensitivity to select these patients. As an alternative, preoperative laparoscopy with or without biopsy has been investigated to establish whether it can better predict resectability of disease over and above standard imaging protocols. The overall risk of injury for diagnostic laparoscopy used for this indication is 1% – 5% depending on the type of procedure and the patient population (27). A systematic Cochrane review analyzed 18 studies of diagnostic laparoscopy in this context of which one was a randomized controlled trial. Laparoscopic preoperative assessment predicted resectability to no visible residual disease in 54% to 96% of the cases and when the criterion of prediction of >1cm residual disease was used, the accuracy was between 69% and 100% in analyzed studies. Because of large heterogeneity, pooling of the data was not possible for meta-analysis (28). There is the limitation that in some studies laparotomy was only performed when laparoscopy suggested that debulking to <1 cm was possible but not for the other cases, hence introducing bias. Although it appears that laparoscopy improves the accuracy of prediction of resectability to no residual disease, some patients undergoing laparotomy nevertheless end up with residual disease of >1 cm. Again, the effectiveness of this procedure depends upon the experience of the surgeon performing the laparoscopy and primary debulking surgery. Published studies have included very different designs and patient cohorts (29–34). The most important parameter with regards to diagnostic laparoscopy relates to the proportion of women falsely predicted to have no residual disease after primary debulking surgery as such cases would undergo unnecessary, unsuccessful debulking surgery. Vergote 2010 (35); and Kehoe 2015 (36) showed that treatment with NACT was associated with no worse prognosis in advanced ovarian carcinoma as compared to primary debulking surgery. In analyzed studies negative predictive values (NPV) ranged from 0.54 to 0.96 for microscopic complete debulking which means that of 100 women referred for primary debulking surgery, after laparoscopic assessment, between 4 and 46 would be left with visible residual disease. All studies report on the added value of preoperative diagnostic laparoscopy, without an increased risk of complications. It seems that diagnostic laparoscopy to assess optimal resectability in advanced ovarian carcinoma has its place in clinical practice, but future research should focus on selection criteria of women who might benefit from this procedure.
Laparoscopic surgery in patients post NACT
After it was demonstrated that the safety and benefit of interval debulking surgery post NACT compared favourably with primary debulking surgery in advanced ovarian carcinoma, there has been increasing interest in performing this surgery laparoscopically in patients with a complete radiological response (37–42). Published studies have shown the feasibility of this approach, benefiting approximately 15% of the patients, but evidence of a favourable outcome is still not clear. There are certainly well-known benefits to patients if this surgery is performed laparoscopically, but there is no strong evidence that outcome in terms of DFS and OS is comparable or better than for laparotomy. Further studies are necessary to support this approach. Currently laparoscopic interval debulking can be offered to patients with a complete radiological response in the setting of a study, until further evidence emerges as to for which subgroups of patients this approach performs in a manner equal to or better than laparotomy.
Cervical Cancer
Cervical cancer is still a significant health problem with an estimated 604,000 new cancer cases worldwide and 342,000 deaths in 2020 (43). In countries with no access to cervical cancer screening the incidence is 17.8 cases per 100,000 women with a mortality rate of 9.8 per 100,000 (44). In developed countries, due to vaccination and screening programs there has been a 75% decrease in incidence and mortality of cervical cancer over the past 50 years (45). In those countries with screening there has been an apparent stage shift at the time of diagnosis towards early-stage disease, with a significant number of cases now diagnosed at stage I disease. For patients who do not wish to preserve fertility, radical hysterectomy (RH) with surgical assessment of pelvic +/- para-aortic lymph nodal status is recommended as a standard treatment for early-stage cervical cancer: stage IB1-IIA as defined by the International Federation of Gynecology and Obstetrics (FIGO).
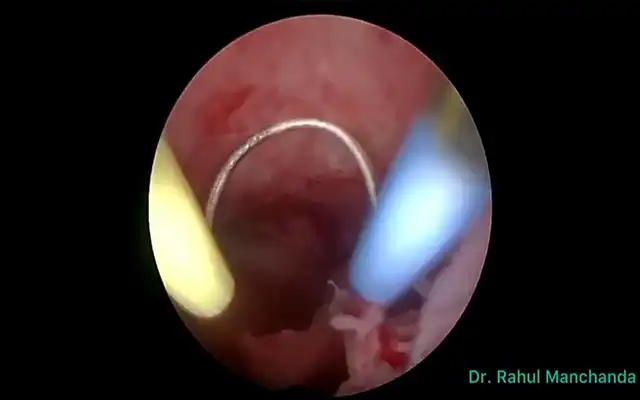
For more than a century open radical hysterectomy (ORH) was the procedure of choice in the management of early cervical carcinoma. This operation was first described by E. Wertheim in 1898, and the alternative was radical vaginal hysterectomy described by his contemporary F. Schauta (46,47) Lymph nodal metastasis is the most important prognostic factor and Meigs introduced pelvic lymphadenectomy as a standard addition to RH in the management of early cervical carcinoma (48–51). In 1992 Nezhat described laparoscopic radical hysterectomy (LRH) with pelvic lymphadenectomy. Bilateral pelvic node dissection is used to assess nodal status and the complications of this procedure include lymphocyst formation, leg lymphoedema and less commonly, vessel and nerve injury (52,53). Alternatively, sentinel lymph node biopsy (SLNB) can be performed with a similar, if not superior detection rate of involved nodes, with reduced postoperative side effects (54–60). The majority of the published data on SLN in cervical carcinoma including recent systematic reviews suggests that this method is accurate in detecting metastasis to the pelvic and para-aortic lymph nodes, with a promising low false negative rate (56). There are no randomized controlled studies confirming this hypothesis. Currently the SENTICOL III randomized trial is underway to provide further grade I evidence.
Lymph nodes are routinely processed in paraffin embedded blocks with one haematoxylin and eosin (H and E) stained slide per node. All SLNs should be processed initially with an H and E section and if this section is benign, then ultrastaged as described previously (53,54). Some centers perform frozen section assessment of lymph nodes if they are reported as possibly involved on preoperative imaging. In these cases, if a lymph node is found to be positive intraoperatively, the surgical operation is abandoned, and patients are offered radical chemoradiotherapy instead. According to international criteria, metastatic disease in lymph nodes is classified by size as macrometastatic (>2mm), micrometastatic (>0.2-2mm) or as isolated tumor cells (≤ 0.2mm).
Total laparoscopic hysterectomy (TLH) is accepted treatment for stage IA1 and low risk IA2 cervical carcinoma, for patients who do not wish to preserve fertility. Radical hysterectomy has been the main treatment for early cervical carcinoma of high-risk stage IA2 to IIA for more than a century. Open radical hysterectomy with pelvic lymphadenectomy was the surgical gold standard until 1992, when laparoscopic radical hysterectomy (LRH) was described (61). In subsequent years Minimally Invasive Surgery (MIS), gained significant popularity as surgical treatment of early cervical carcinoma. These surgical techniques were associated with less intraoperative blood loss; fewer postoperative complications (infections, deep venous thrombosis); less analgesic needed for postoperative pain; a shorter hospital stay; quicker recovery and better aesthetic results (62–64). These procedures quickly became the favored approach for both patients and many surgeons. Initial publications suggested a similar oncological outcome as compared with classical open radical hysterectomy. However, none of these early studies were randomized trials (65–70). With respect to oncological outcome such as DFS and OS, the majority of published studies did not find a significant difference between open and laparoscopic approaches for early cervical cancer (62–70). However, these data were not from randomized controlled trials.
The Laparoscopic Approach for Cervical Cancer (LACC) was the first randomized controlled, multicenter trial comparing MIS with open surgery, published in 2018. This trial raised concerns that MIS had an inferior oncological outcome when compared with the open approach in the management of early cervical carcinoma. Minimally Invasive Surgery (laparoscopic and robotic radical hysterectomy) had a 4.5-year DFS of 86.0% compared with 96.5% for open radical hysterectomy (10.5% difference between the groups 95% CI: -16.4 to – 4.7; p=0.87 for non-inferiority). The 3 year OS rates were 93.8% for the MIS arm and 99.0% for the open approach (HR for death from any cause, 6.00; 95% CI: 1.77 to 20.30) (71). This publication was the first randomized trial comparing MIS and the traditional open technique and it had a major impact on clinical practice around the world. As a result of this publication, some societies (ESGO, NCCN, BGCS) changed their recommendations with respect to MIS in the management of early cervical carcinoma. Many institutions and individual surgeons stopped preforming LRH or changed their indications for MIS in early cervical cancer. Although the results from the LACC trial made a major contribution to clinical practice in the surgical management of early cervical cancer, criticisms have been raised regarding the trial and there remain a number of valid unanswered questions.
Several renowned centers, with significant experiences and with published data on LRH and RRH, did not take part in this trial. Some clinicians raised concerns regarding the low level of surgical experience (previous experience of 20 cases of LRH) as the entry criterion to the LACC trial. This is a low number of cases to gain proficiency in this difficult surgical procedure which is associated with a long learning curve.
In addition, with participation of 33 centers in total, some of the centers recruited fewer than 10 patients each which also raises questions regarding the experience of these centers with RLH. Results shown in the open arm were also far superior than ever published previously.
Our own data over 15 years, for 100 patients that underwent a LRH performed for tumors > 2cm in diameter, in terms of DFS and OS are almost identical when compared to the open arm of the LACC trial, with a minimum of 5 years of follow up. In our cohort of patients, 13% required adjuvant treatment compared with 33% in the LACC trial.
Our study with RLH and SLNB only in the management of early cervical carcinoma as compared to the LACC trial, does not appear to be associated with any higher recurrence rate or mortality in the selected group of patients with cervical cancer <2 cm in size (55,60).
It has been suggested that the increased recurrence rate in the vagina and pelvis in the MIS arms of the LACC and SUCCOR (72) studies may be due to uterine manipulation during laparoscopic surgery. In our practice we used a McCartney tube (which does not have intrauterine component) to manipulate the uterus and outline the vaginal vault and we did not observe an increase in vaginal vault or central pelvic recurrences. The other suggested technique, to reduce vaginal vault recurrences, is to perform RLH without a manipulator and with closure of vagina vault which is done as the first step of the operation.
Conclusion
After publication of the LACC trial in 2018 many institutions have abandoned RLH in the management of early cervical carcinoma. However, our experience over 15 years and non-randomized studies published prior to 2018 demonstrate the safety of LRH in the management of FIGO 2018 high risk stage IA2 and stage IB1 and IB2 cervical carcinoma.
There is a clear need for another randomized controlled trial to provide evidence for the place of RLH in the management of early cervical carcinoma. There is a need to clearly identify the cohort of patients who would benefit from a laparoscopic approach to define the safest technique and to define the radicality of the surgery. Currently If RLH is considered for the management of cervical carcinoma of stage IA2 – IB2 all patients require informed consent with an explanation of the results from both the LACC trial as well as the results of the individual center treating that patient. All results, DFS, OS, and complications, should be prospectively recorded and reported at clinical governance meetings and monitored by the institution. Patients with bulky lymph nodes identified on preoperative imaging or intraoperatively should be excluded from the SLN only procedure and treated as per center protocol for possible positive lymph nodes. Unilateral SLN detection requires a full contralateral pelvic node dissection. Pathological ultrastaging should be standard procedure in the assessment of the SLN. Further data are required regarding the clinical significance of ultrastage-detected micrometastasis and isolated tumor cells to guide appropriate management.
Endometrial Cancer
Worldwide, endometrial cancer is the sixth most commonly diagnosed malignancy in women and the most commonly diagnosed gynecological malignancy in the developed world (4).
-The incidence in the United Kingdom hasincreased by around 55% since the 1990s (73)and this is thought mainly due to increasing ratesof obesity and life expectancy (74). Obesity (75),nulliparity and the presence of Lynch Syndromeare risk factors of the most significance (76). Thedisease is predominantly a condition ofpostmenopausal women. Seventy-one percentof cases are stage I at presentation which carriesan excellent prognosis; 90% of women aredisease-free five years following surgery (77).
Laparoscopy for the management of early stage endometrial cancer
The current standard of treatment for FIGO stage I endometrial cancer (78) involves removal of the uterus, tubes and ovaries +/- lymphadenectomy, without vaginal cuff and nor parametrectomy (79). For stage II disease, total hysterectomy and bilateral salpingo-oophorectomy is adequate, unless a radical hysterectomy is required to achieve macroscopic disease-free margins. A meta-analysis in 2019 suggested that there was no significant benefit in terms of overall survival or progression free survival from radical hysterectomy (80) for stage II disease. Patients with stage III/IV disease are often referred for adjuvant treatments such as external beam radiotherapy and/or chemotherapy to reduce disease burden. A meta-analysis by Barlin et al. suggested that there is a 9.3 month increase in survival associated with each 10% increase of cytoreduction towards no gross evidence of disease (81). There is very limited evidence for the role of laparoscopic surgery as treatment for endometrial cancer greater than stage I.
Several randomized controlled trials examining laparoscopy versus laparotomy for the treatment of early stage endometrial cancer including Walker’s study of 2016 patients (82) and Janda’s ‘LACE’ trial (83) have shown no significant difference in overall survival and disease free survival between either type of surgery (84). This was demonstrated by a Cochrane review of 2018 with the same research question examining 9 randomized controlled trials. Six of the studies examined survival and found no significant difference (with moderate evidence levels) between women who underwent laparoscopic surgery and women who underwent laparotomy (n = 3993) (HR 1.04, 95% 0.86 to 1.25) (85). Five of the studies included showed no difference in the probability of disease recurrence. Notably, there was no difference in rates of perioperative death or bladder, ureteric or bowel injury. On average, postoperative hospital stay was significantly shorter in the laparoscopy group (86). The literature is almost unanimous to the effect that recommendations from governing bodies strongly recommend removal of the uterus, cervix and tubes without morcellation or dissection, to reduce the risk of cancer cell seeding.
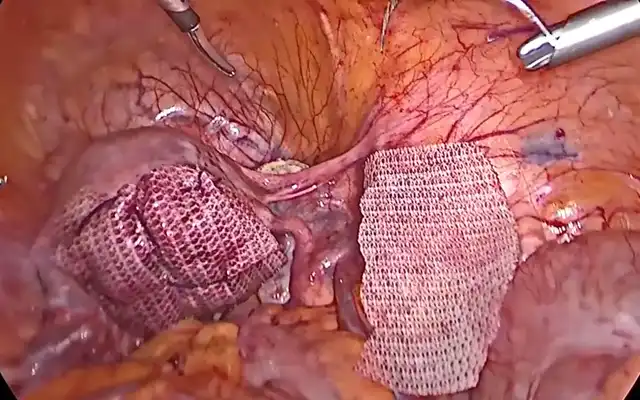
Laparoscopy in the role of lymph node staging
Lymphadenectomy is considered a staging procedure by the British Gynaecological Cancer Society (BGCS) (79) and the European Society of Gynaecological Oncology (ESGO) (86) to assess the extent of disease and therefore provide information to guide adjuvant treatment decisions. These recommendations are following evidence from two randomised trials that suggested systematic lymph node staging has no therapeutic benefit (87,88). Although formally staged histologically, the stage and grade of endometrial cancer is often established prior to surgery by MRI and endometrial biopsies. Following Vargas’ analysis of 19,329 women included in Surveillance Epidemiology and End Results (SEER) data published in 2014, low risk endometrial cancer (stage 1A, grade 1-2, tumour size <2cm) has a 1.4% probability of lymph node metastasis (89). Therefore, the BGCS does not recommend lymphadenectomy for non-bulky nodes, especially for low-risk endometrial cancers (79). This is in light of the known increased risk of lower limb lymphoedema, highlighted by one study to increase by 6% for every lymph node surgically removed (90). However, our unpublished results and a few other studies, demonstrated a higher percentage of involved lymph nodes, especially in stage IB, of up to 15% of cases. Another problem in making a decision to perform lymphadenectomy in patients with a G1 tumor on biopsy is that after final histology on the hysterectomy there is upgrading in up to 20 – 30 % of cases. For higher risk endometrial cancers (>stage IA, grade 3, tumor size >2cm) in which up to 6% – 30% of patients might have lymph node metastases [93], sentinel lymph node biopsy is recommended by the BGCS (79) and ESGO (86) as a way of reducing post-operative morbidity yet obtaining staging information to guide adjuvant treatment. This guidance follows the “FIRES” study in 2017 (91) and separate studies on both low risk, early stage endometrial cancers (92) and patients with high grade disease (93).
Indocyanine green dye (ICG) has been found to be superior to methylene blue dye in a recent randomized controlled trial (94) and in a separate study, technetium 99 in combination with ICG did not improve detection rates when compared to ICG alone (95). In order to facilitate the detection of ICG uptake in sentinel lymph nodes, laparoscopic and robotic assisted surgical approaches are recommended as part of a number of recommendations included in a BGCS consensus statement on sentinel lymph node technology (32).
Conclusion
Laparoscopic surgery has a significant role in the management of gynecological malignancies (ovary, cervix, endometrium). However, most evidence is not from randomized trials and needs further grade 1 evidence studies before the specific role for this type of surgery is clear. Till then, it is paramount that results related to individual surgeons/ institutions are recorded and regularly audited. Surgeons need to be adequately trained to perform this type of surgery and patients appropriately selected. Complexity of these operations require up-to-date laparoscopic equipment. Patients need to be informed of published results as well as of individual surgeons/institution results. Informed consent for laparoscopic procedure needs to be obtained.