Authors / metadata
DOI: 10.36205/trocar6.2025014
Abstract
Presacral tumours are rare entities that may present with non-specific symptoms such as chronic pelvic pain, often mimicking endometriosis. Among these, cystic hamartomas are particularly uncommon and may remain undiagnosed for extended periods. Case Presentation: The case of a 35-year-old woman with chronic pelvic pain, tenesmus, and dyspareunia. MRI identified a wellcircumscribed presacral mass (4.4 × 5.1 × 3.5 cm) is reported. A laparoscopic approach was performed for complete excision. Intraoperative findings included a soft, well-demarcated lesion without evidence of invasion. Histopatholy confirmed a retrorectal cystic hamartoma. The patient’s postoperative course was uneventful, and she experienced complete resolution of symptoms within three months.
Surgical Approach: The procedure involved precise dissection of pelvic planes and identification of critical neurovascular structures, preserving the sacral nerve roots. Tumour retrieval was achieved via a containment bag to minimise the risk of spillage following inadvertent capsular rupture.
Conclusion: This case demonstrates that laparoscopic management of presacral cystic hamartomas is feasible and safe in experienced hands. It highlights the importance of differential diagnosis in chronic pelvic pain and supports the minimally invasive approach as an effective therapeutic option.
Introduction
Retrorectal tumours are an uncommon group of lesions that may be benign or malignant. Depending on their size, they may be asymptomatic or symptomatic. These lesions may originate from embryological remnants or result from malignant transformation of local elements (1,2). Surgical management requires complete tumour excision due to their location and symptomatic presentation. The differential diagnosis of presacral or retrorectal tumours includes neurogenic, congenital, osteogenic neoplasms, and inflammatory processes (3).
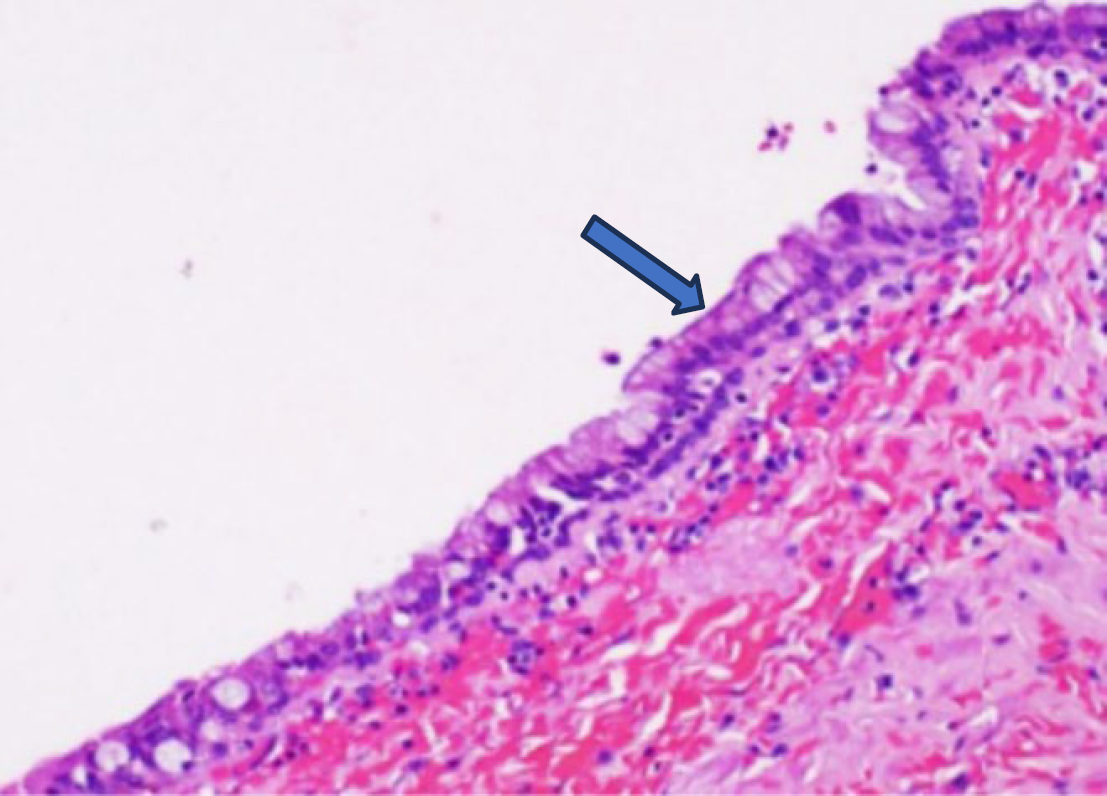
Anatomically, these tumours typically grow within a space bordered superiorly by the peritoneal reflection and inferiorly by the levator ani and coccygeal muscles. Cystic hamartomas may be multilocular or multiseptated and are frequently lined with various types of epithelia. Their walls often contain smooth muscle fibres (4).
Case Report
A 35-year-old nulligravid woman presented with chronic pelvic pain, rectal tenesmus, defecatory difficulties, dysmenorrhoea, and dyspareunia. On rectal examination, a soft, tender mass was palpated, expanding to the right hemipelvis. MRI revealed a 4.4 × 5.1 × 3.5 cm hypointense mass on T1-weighted images, displacing the sacrum posterolateral on the right. The patient was discharged 48 hours postoperatively without complications. Follow-up evaluations at one, three, and six months confirmed complete symptom resolution. She also completed 21 sessions of pelvic floor physiotherapy. Informed consent for academic publication, including surgical video material, was obtained.
Surgical Technique
Under general anaesthesia, the patient was placed in the Lloyd-Davies position. An open entry via the umbilicus was followed by insertion of 5 mm ancillary trocars in the right and left iliac fossae and suprapubic region.
•Step 1: Dissection of the sigmoid Todt’s fascia using ultrasonic energy and blunt dissection.
•Step 2: Dissection of pelvic fascia at the promontory towards the right uterosacral ligament with ultrasonic energy, allowing entry into the right Okabayashi space. Dissecting and spreading manoeuvres revealed ipsilateral inferior hypogastric plexus fibers. The same approach was performed contralaterally.
•Step 3: Avascular space dissection continued to identify the inferior hypogastric plexus.
•Step 4: Dissection proceeded to the retro cervical area and Denonvillier’s’ fascia to mobilize the rectum and expose the bilateral presacral space.
•Step 5: Dissection of the rectovaginal septum allowed further mobilisation of the rectum and access to the retrorectal space.
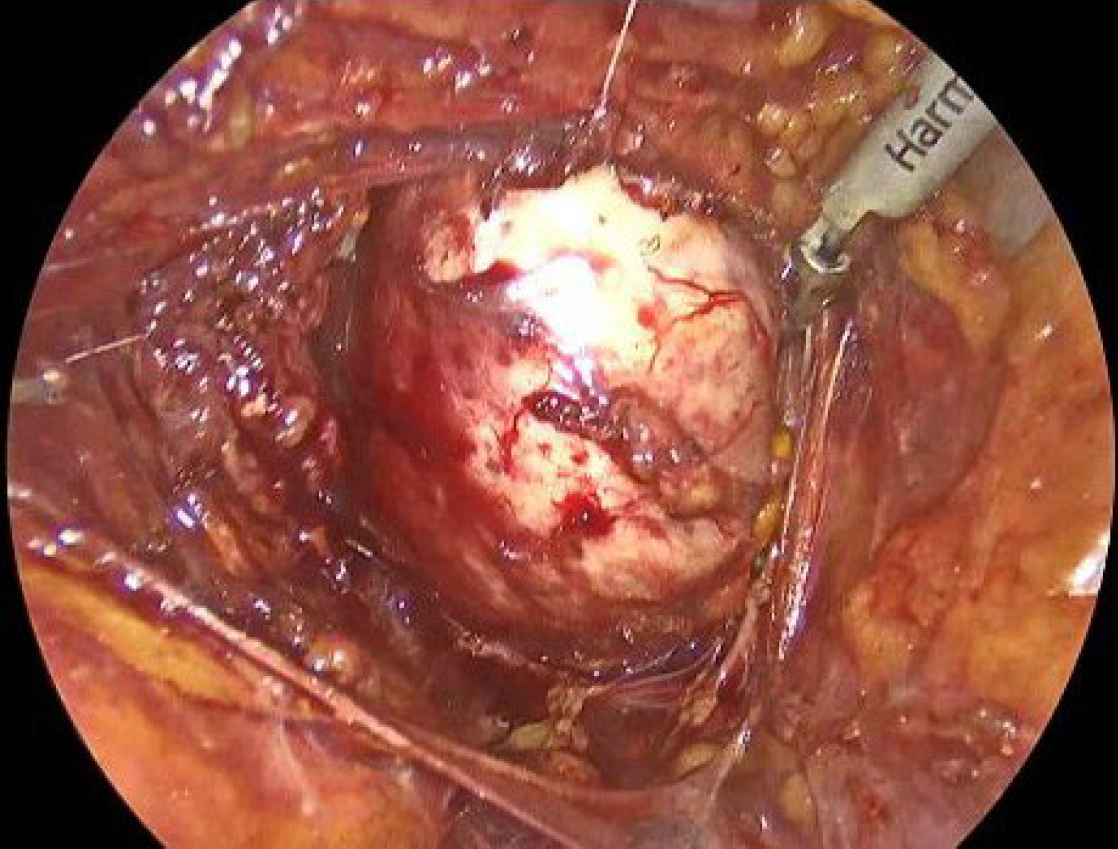
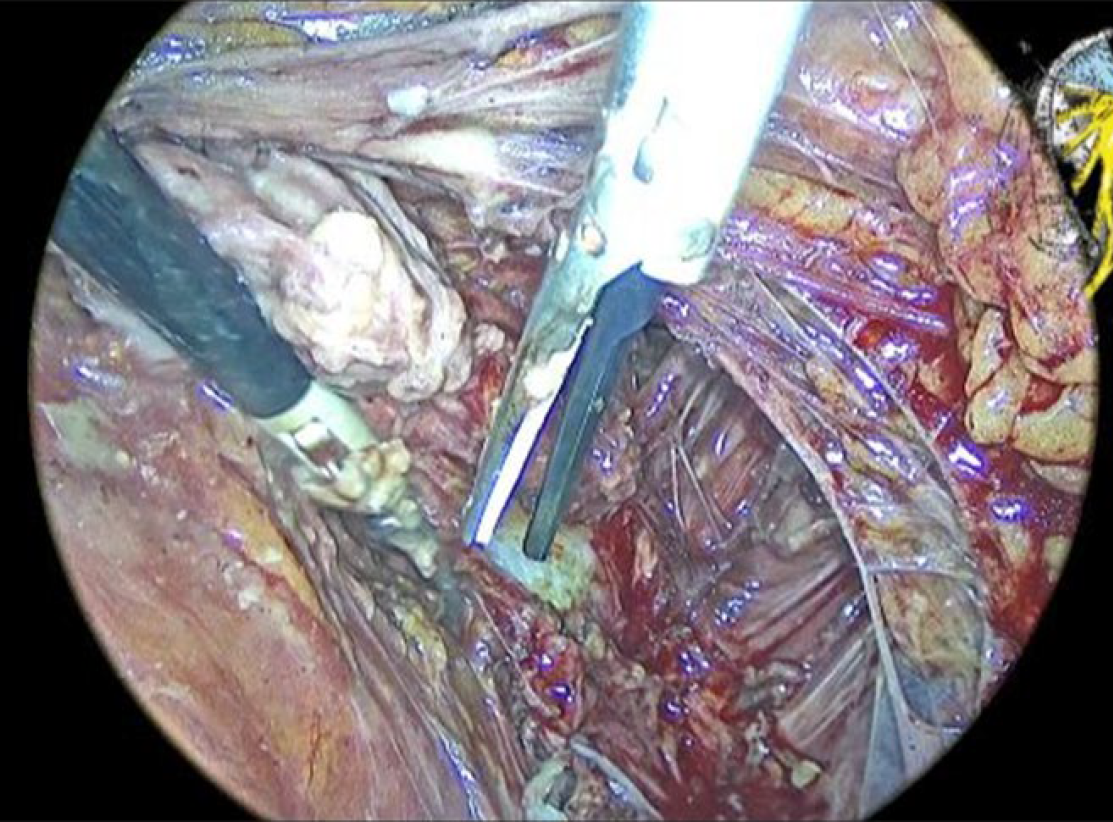
• Step 6: Dissection of the pararectal space and suspension of the right ovary with Monocryl 00. A soft, well-defined tumour (4 × 5 cm) was identified without invasion of bony or visceral structures. Dissection continued until Waldeyer’s fascia was exposed, with the coccygeus and levator ani muscles defining the lateral and caudal limits. Presacral nerve roots at S3 were visualised and preserved during tumour excision (Figure 1–2). Inadvertent rupture of the capsule occurred, and the contents were aspirated immediately.
Results
The total surgical time was 115 minutes, with minimal blood loss (120 cc). No intraoperative or postoperative complications were recorded. The patient was discharged 48 hours post- procedure and remained symptom-free during follow-up. The laparoscopic approach resulted in rapid symptom resolution, despite the tumour’s deep presacral location.
Discussion
Presacral hamartomas are exceedingly rare, with few published cases. Most patients present with pelvic pain suggestive of endometriosis. However, deep peritoneal endometriosis is less frequently implicated in such symptoms. The laparoscopic approach offers minimal invasiveness and improved visualisation, enhancing surgical safety. The surgical team’s anatomical expertise was critical. Inadvertent rupture of the tumour during dissection necessitated prompt aspiration to minimise the risk of tumour spread, and the retrieval bag ensured safe specimen removal (5). Histopathological analysis confirmed a cystic hamartoma in the retrorectal/presacral space (Figure 3). In the limited literature, most excisions have been performed via open or perineal routes, particularly the laterosacral approach. Laparoscopy remains underutilised due to technical complexity and anatomical constraints. However, expert pelvic surgeons can safely navigate deep spaces such as S3, achieving complete tumour excision with low morbidity. This case illustrates the importance of considering rare causes of pelvic pain. The tumour’s cyclical symptomatology mimicked endometriosis, likely due to compressive effects on adjacent nerve structures. Although typically benign, cystic hamartomas warrant complete excision due to their potential for malignant transformation (6,7).
Complete surgical resection is the traditional treatment of choice, eliminating the potential of recurrence, haemorrhage, infection,
compression, and malignant changes (8,9)
Conclusion
Laparoscopic management of presacral tumours offers high effectiveness and minimal invasiveness. Nonetheless, it demands a thorough understanding of pelvic anatomy and expert surgical skills.