Authors / metadata
DOI: 10.36205/trocar6.2025016
Abstract
Introduction : Hysteroscopy is often hindered by impaired vision due to distension media leakage between the hysteroscope’s eyepiece and the camera head, causing fogging and blurring that necessitates frequent disassembly and cleaning. This prolongs surgical time and can increase surgeon frustration. This study evaluated the “GloveSeal” technique, a simple, cost-effective modification using a modified sterile surgical glove to create a watertight barrier, preventing this issue.
Methods: A prospective comparative study was performed on 40 patients undergoing complex hysteroscopic procedures. Patients were split into the standard assembly group (n=20) and the GloveSeal group (n=20). The primary outcome was visual quality during hysteroscopy.
Results: The GloveSeal group demonstrated a statistically significant improvement in mean visual quality score compared to the standard assembly group (1.45 vs. 0.75, P < 0.01). “Good quality” vision was maintained more often and vision deterioration requiring cleaning occurred significantly fewer times in the GloveSeal group (P < 0.05).
Conclusion: The GloveSeal technique provides a more consistent visual field during hysteroscopy and reduces the frequency of surgical interruptions, potentially leading to more efficient and effective procedures.
Introduction
Hysteroscopy is a technique to visualize the uterine cavity using a hysteroscope inserted through the cervical canal. The ability to identify and treat intrauterine pathology is dependent on clear and consistent visualization throughout the procedure provided by uterine distension by distension media. The hysteroscope is inserted and secured into a metallic sheath which may be diagnostic or operative and of different sizes. Modern diagnostic and operative sheaths feature isolated, dual ports that provide continuous laminar flow of the distending media, ensuring optimal irrigation and imaging of the uterine cavity. The sheath and scope together are assembled with the camera head (1). While impairment of vision in laparoscopic and robotic surgery occurs at the objective lens in the tip of the scope, due to temperature and humidity differences or contact with bodily fluids, the impairment of vision in hysteroscopic surgery occurs at the eyepiece (2).
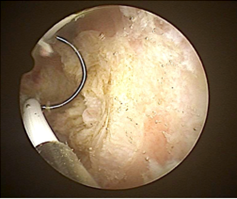
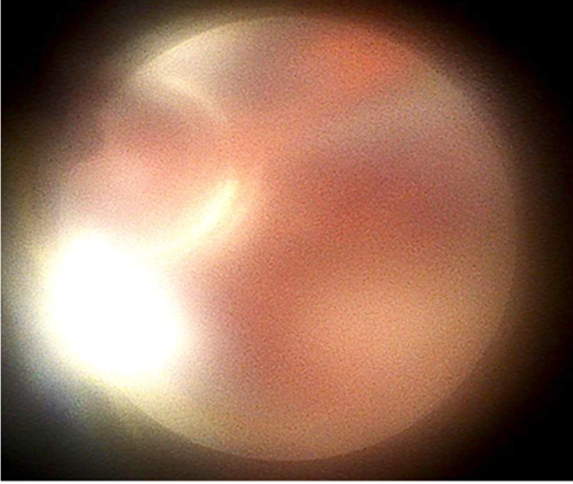
Fluid spilled from the cervix around the hysteroscopy sheath runs down the exterior of the sheath, down to the camera head. Here, the fluid insinuates between the parts of the assembly to collect between the head and the scope. As a result, there is fogging of the image on the monitor, blurring and “halo-like” distortion of light. The view is clear initially (Figure 1) but starts deteriorating as the surgery proceeds due to the moisture between the camera head and the telescope eyepiece, eventually causing complete fogging of vision (Figure 2).
Unlike the lens fogging during laparoscopic surgery, cleaning this fluid requires complete disassembly of the hysteroscope from the camera. This issue can recur leading to frequent interruptions in surgery to restore optimal vision, increasing overall procedure time and contributing to surgeon frustration. The problem is further complicated when a sterile plastic camera cover is used as fluid gets accumulated within it. It also occurs when the same camera unit is used for laparoscopy in the same sitting, as in diagnostic hystero -laparoscopy for infertility. We suggest the GloveSeal technique, a cost effective and technically simple modification of the standard hysteroscope assembly using a modified sterile surgical glove to “seal off” the camera head, forming a watertight barrier between the camera head and the hysteroscope. This reduces the problem of lens fogging leading to clearer vision and all but eliminating the need for disassembly and cleaning of the camera head. The efficacy of this technique was evaluated in a comparative study measuring the quality of vision with and without using the technique.
Material and Methods
Experimental Design: A prospective comparative study was performed on 40 patients undergoing hysteroscopy. The study included patients undergoing complex operative hysteroscopic procedures of ISGE Level IIa and above as well as patients undergoing diagnostic laparoscopy in the same session. Patients undergoing diagnostic hysteroscopy and simple operative procedures were excluded. from the study. The procedures were performed by a single surgeon. The standard hysteroscope assembly was used in 20 patients (Group 1, n = 20) and the GloveSeal assembly in 20 patients (Group 2, n = 20).
Instruments and Technique: A 2.9 mm 30° hysteroscope was the principal optical element connected to a three-chip HD camera control unit and monitor with an LED light source. A 5 mm Bettocchi-type operative sheath and 18 to 22 French resectoscopes were used as required. The standard assembly involved the scope assembled with its sheath and the entire assembly connected to the camera head with a sterile plastic cover around it. The GloveSeal technique involved the use of a sterile surgical glove as a seal between the scope and the camera head in addition to the sterile plastic cover.
The GloveSeal was assembled as follows:
- The hysteroscope was assembled with its sheath.
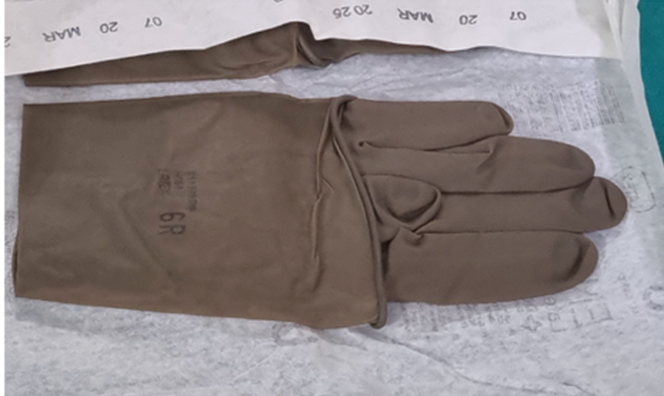
- A sterile surgical glove of size number 6 was taken (Figure 3).
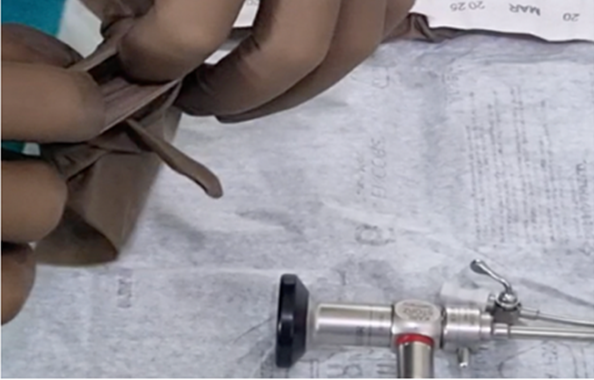
- The middle finger was cut at its tip (Figure 4).
- The cut tip of the middle finger was stretched over the hysteroscope eye piece (Figure 5, 6).
- The index and ring fingers were wrapped tightly around the scope and tied to form a knot or left loose at the surgeon’s discretion (Figure 7)
- The camera head was connected to the hysteroscope and the glove was dragged over the camera head (Figure 8, 9).
- The camera head was draped with a sterile plastic cover, over the glove.
- The glove with the plastic cover around it was secured with a wire tie, completing the GloveSeal (Figure 10, 11).
The inflow and outflow channels were connected as usual. The distension media used was 0.9% Normal Saline, infused with a HysteromatÒ (Karl Storz Se & Co KG Tuttlingen Germany). A Sims’ speculum was introduced into the vagina. The hysteroscope assembly was placed at the external os and advanced under visual guidance. The use of dilators and vulsellum for entry were permissible at the discretion of the surgeon. Instruments and electrosurgery were used as required.
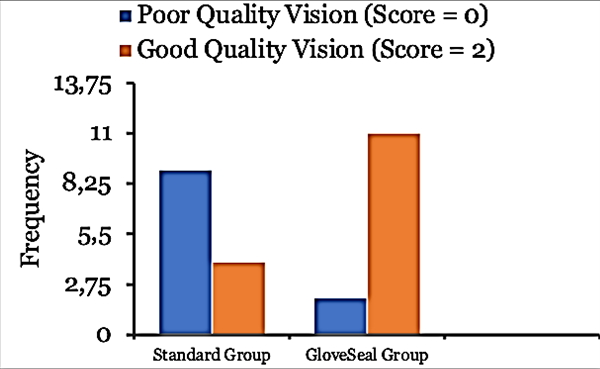
Outcome Measures: The primary outcome measure was the quality of hysteroscopic vision and was scored by the surgeon at the end of the procedure. Impact of fogging and blurring on the vision of the uterine cavity were measured by an arbitrary scoring system (0 = significant impairment of vision, requiring cleaning of the instrument, 1 = some impairment of vision and fogging, 2 = good quality vision). The details were recorded on a proforma.
Statistical Analysis: The data collected was tabulated and analyzed with JASP Team (2024). JASP (Version 0.19.3 computer software). Mann – Whitney test was used for comparison of ordinate variables. Two-tailed P-values <0.05 were considered significant. Fisher’s exact test was used for comparison of frequencies. Data represented as mean ± standard deviation unless mentioned otherwise.
Results
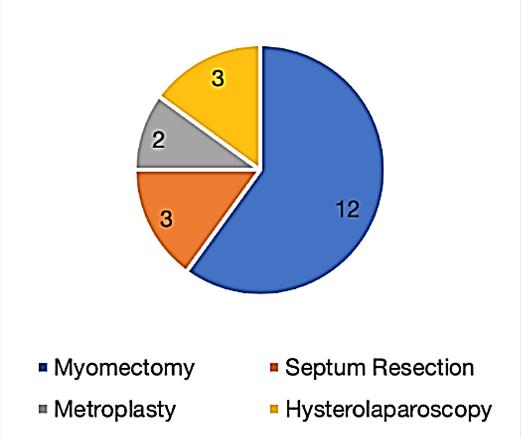
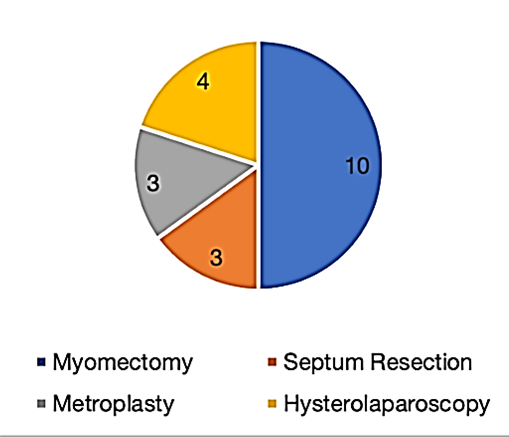
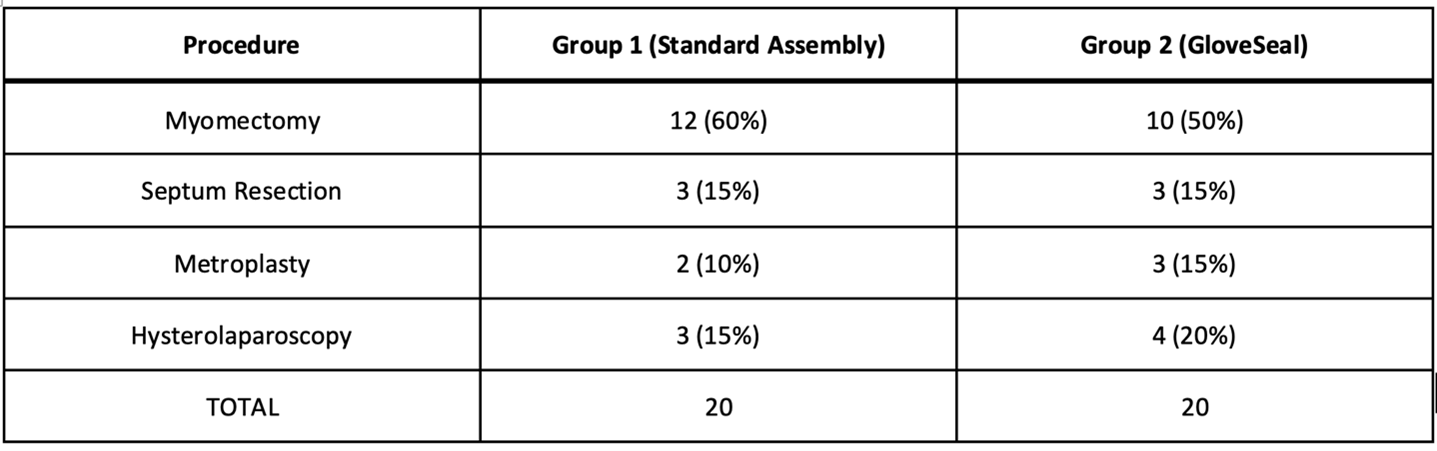
All patients included in the study, divided in the standard assembly group (group 1: n = 20) and the GloveSeal group (group 2: n = 20) were analyzed. The procedures performed across both groups were 22 hysteroscopic myomectomies (55%), six hysteroscopic septum resections (15%), five hysteroscopic metroplasties (12.5%) and seven diagnostic hystero laparoscopy procedures (17.5%). They were divided similarly in both groups, being myomectomy in 12 (60%) and ten (50%) cases, septum resection in three (15%) and three (15%) cases, metroplasty in two (10%) and three (15%) cases and hystero laparoscopy procedure in three (15%) and four (20%) cases respectively.
A statistically significant increase in mean visual quality score was noted for the GloveSeal group compared to the standard assembly group (1.45±0.686 versus 0.75±0.786, P < 0.01). ‘Good quality’ vision (visual quality score = 2) was maintained throughout the procedure significantly more often in the GloveSeal group (P < 0.05). Deterioration of vision to the point where cleaning was required (visual quality score = 0) occurred significantly fewer times in the GloveSeal group (P < 0.05). There were no complications in any case.
Discussion
While many studies describe the impact of fogging and operative vision disruption during laparoscopic and robotic surgery, to our knowledge no previous studies have explored this impact in hysteroscopic surgery. Frequent interruptions in the surgical procedure due to operative vision disruption contribute to prolonged operative time, surgeon workload, cognitive burden and impaired patient safety (2-6). This study aimed to evaluate the efficacy of the GloveSeal technique to prevent operative vision compromise. The GloveSeal technique was developed in an effort to reduce the burden of repetitive cleaning of the hysteroscope while performing surgery, while being simple to implement and only using readily available materials. The latex surgical glove size number 6 was selected as it is the smallest glove size available in most operation theatres that also fits securely around the hysteroscope eye piece and because of its trivial cost. The authors used a size 6 glove (Encore® Latex Micro, Ansell, India) because of its powder free nature and good elasticity but any sterile, powder free latex surgical glove of size 6 or 6.5 from any manufacturer may be used. Stretching the cut end of the glove finger over the eyepiece is easier than negotiating the entire scope through the wrist cuff. The final GloveSeal assembly provides a watertight barrier around the eyepiece for additional security against leakage. Clear visualization of the uterine cavity is important for the safe and effective execution of hysteroscopic procedures. The GloveSeal technique maintains a more consistent and superior visual field. Poor visualization necessitates frequent withdrawal of the hysteroscope for cleaning. In addition to the time lost in disassembling and cleaning the hysteroscope, further time is required to reestablish optimal vision inside the uterine cavity which is frequently stained with blood clots in the interim. This prolongs operative time, potentially increasing patient discomfort and risk of complications. The advantage of the GloveSeal technique lies in its ability to prevent vision deterioration to the critical point where cleaning is required more often, leading to a smoother procedure. As all procedures in this study were performed by a single surgeon, further research with a larger cohort of multiple operators would be beneficial to validate the findings and assess the technique’s generalizability across different operating scenarios.
Conclusion
This study demonstrates the impact of distension media leakage on visual quality and presents a cost-effective solution that provides a statistically significant improvement in visual quality and reduction in frequency of surgical interruption. Its simplicity and wide applicability can potentially lead to more efficient and effective procedures.