Authors / metadata
DOI: 10.36205/trocar1.2020007
Abstract
Objective: to report three successful cases in 2017 using a method of intra-ovarian direct trocar penetration and drainage for access prior to laparoscopic surgery in the case of giant ovarian cyst.
Methods: We reported three case series of patients diagnosed with giant ovarian cysts who underwent direct trocar penetration to the cyst and drainage for access followed by laparoscopic cystectomy. All of these patients had no history of previous laparotomy. The size of the cysts was more than 25 cm in diameter each. To exclude malignancy, transabdominal and transvaginal ultrasounds using the International Ovarian Tumor Analysis (IOTA) criteria and laboratory test including tumor markers were performed prior to surgery. The intraovarian direct trocar penetration and drainage technique was performed by penetrating a 5-mm trocar at the Palmer point site directly into the cyst followed by fluid drainage. This procedure was then followed by laparoscopic cystectomy, partial oophorectomy and unilateral oophorectomy, respectively.
Results: In one case, the cyst’s fluid was found to be serous with approximately 3.100 ml in volume. In the other two cases, the cyst’s fluid was thick-dark brownish color as of an ovarian endometrioma with approximately 3.000ml and 3.250ml in volume respectively. There were no complications found following the procedure. After the surgery, all patients were hospitalized for two days. Histopathologic findings of the cysts were benign. In the outpatient clinic, the follow-up after the procedure showed patient’s complete recovery, pain free and were back to daily activity soon afterward.
Conclusion: Intraovarian direct trocar penetration and drainage for access prior to a laparoscopic cystectomy procedure in the case of giant ovarian cyst procures great benefits for the patients with less complications, less time required to full recovery and also less pain experienced. The procedure is safe, applicable, reliable and effective in the management of benign giant ovarian cyst in patients with no history of laparotomy.
Introduction
Ovarian neoplasms are a common clinical problem affecting women of all age groups. These are considered as a the fourth most common reason for gynecologic recoveries in the United States, and it has been estimated that approximately 10% of women in the United States will undergo a surgical procedure for a suspected ovarian neoplasm during their lifetime (1).
The definition of huge ovarian cysts is not well described in the literature. Some authors define large ovarian cysts as those that are more than 10 cm in diameter as measured by preoperative scans (2). Others define large ovarian cysts as those that are reaching above the umbilicus (3).
Laparoscopy is considered the gold standard approach to manage benign ovarian cysts. The benefits of laparoscopy include reduced postoperative analgesic requirement, earlier mobilization reducing chances of deep venous thrombosis (DVT), cosmetic advantages, earlier discharge from the hospital, and return to normal activity. A major factor that will make the gynecologic surgeon decide to perform a laparotomy is the size of the ovarian mass (4).
We propose and describe three cases of the technique of intra-ovarian direct trocar penetration and drainage straight into the giant ovarian cyst. The procedure were undertaken for the purpose of creating access prior to laparoscopic surgery. All of these procedures were performed during the period of January to May 2017. As far as our knowledge, this technical approach of direct trocar penetration and drainage straight in to the cysts have not been reported in the previous study.
Case report
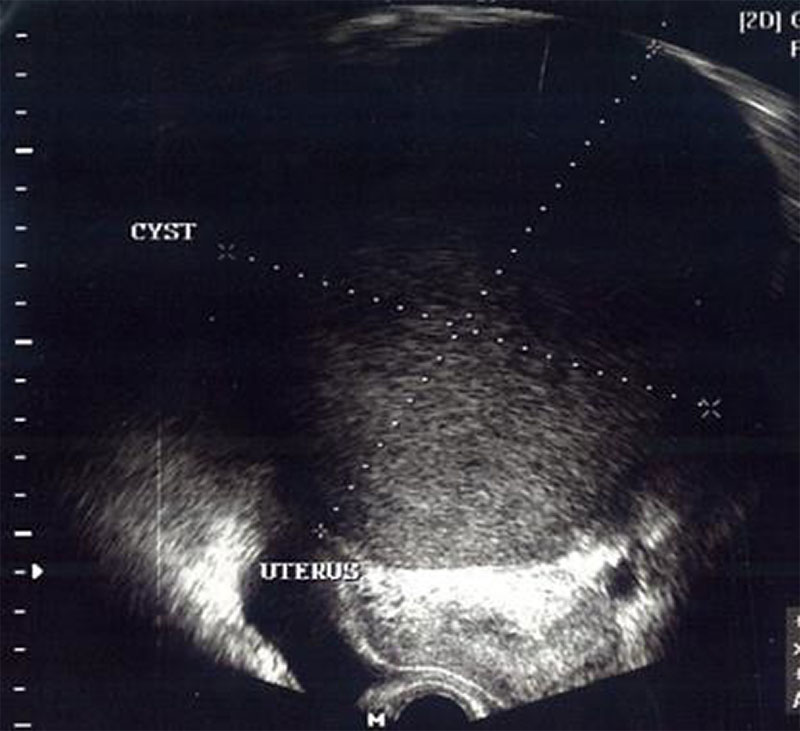
A 31-year old nulliparous woman came to the hospital due to a huge abdominal cystic mass extending from the symphysis pubis to the epigastric region (figure 1). The patient was also experiencing nine years of primary infertility. Pre-operative diagnostic examination was performed by abdominal ultrasound scanning and findings describe a giant cystic unilocular mass of 25x12x12x25cm with acoustic shadowing and no signs of blood flow on the color dopler examination. The diagnosis for this patient were right giant ovarian cyst and uterine fibroid.
Second case reported is a 41- year old nulliparous woman admitted to our department on January of 2017 with as main complaint an enlargement of the abdominal circumference and a huge ovarian cystic mass (figure2). Patient was experiencing 11 years of primary infertility. Prior to the surgery the transvaginal ultrasound scanning revealed a giant unilocular cystic mass on the right ovary with the size of 25X12X25X12 cm with internal echo’s or ground glass appearance and no signs of blood flow in the mass. The laboratory work-up was normal including the tumor markers of CA-125 at 64. The diagnosis was established as right ovarian endometrioma with primary infertility of 11 years.
The third case is a 35-year old nulliparous woman who presented at our Fertility and Reproductive Endocrinology Division in the Department of Obstetrics and Gynecology with a giant abdominal cystic mass in May 2017. The patient has been married for ten years with primary infertility. The mass was measured from symphysis up to one cm above the procesus xiphoideus of about 27X14X27X14 cm. The ultrasound scanning showed a huge cystic unilocular mass on the left ovary with acoustic shadowing and no blood flow. The laboratory finding was within normal limits. The working diagnosis was giant left ovarian cyst with the primary infertility of ten years.
Methods
The patients were brought under general anesthesia, the procedure was started by performing the puncture at Palmer’s point site using a five mm trocar directly into and through the cyst’s wall. Followed by opening the “stopcock” and checking the flow of the drainage. The extraction of the trocar’s obturator was followed by an immediate fluid drainage. Some 3.100ml of serous fluid was drained from the cyst. Following this step, we proceeded to the standard operative laparoscopic procedure starting with Veress needle insertion intra-umbilically followed by drop test and installation of the pneumoperitoneum afterwards. A ten mm trocar was inserted through the umbilical incision as a main channel followed by the telescope. The procedure was continued by inserting one other five mm trocar laterally to the midclavicular line along side of the previous Palmer’s point used as the working channel for the operator. In the first case reported, we performed unilateral salpingo-oophorectomy, myomectomy followed by a chromotubation test showing that both right and left salpinges to be open. The histopathological finding showed nonpapillary serous cystadenoma as the postoperative diagnosis. The patient was discharged from the hospital 24 hour after the procedure.
In the second and third case, the procedures were initiated the same way as in the previous case reported. The procudre did start with the direct trocar penetration into the cyst. A thick brownish liquid drained out from the cysts at the amount of 3.000ml and 3.250ml respectively. The procedure was subsequently followed by the standard laparoscopic surgery as described previously. For the second case the laparoscopic procedure performed was unilateral partial oophorectomy while left salpingo oophorectomy and cystectomy was performed on the third patient. The histopathologic report in both cases revealed endometriosis. The length of stay of the patient in the hospital was two days. On the outpatient clinic follow-up, the patients showed a complete recovery.
Discussion
The largest ovarian tumor ever weighed 1.374 g and was removed intact in 1994 by O’Hanlan (5). In pediatric surgery we usually deal with much smaller abdominal masses. Ovarian cysts are labelled as large when they are over five cm and giant when they are over 15 cm (6). In children, however, it is better to compare the size of the cyst to the size of the peritoneal cavity. Some authors have defined giant ovarian cysts as those reaching above the level of the umbilicus (7). We strongly agree with this statement.
The detection of Ovarian cyst does cause considerable concerns for the women because of the fear for malignancy but it is an established fact that many ovarian tumors present as cysts, but all cysts are not tumors. Serous tumors are the most common cystic neoplasm of the ovary, 60% of which are benign, 25% are malignant, and 15% are borderline cases. Serous tumors usually present as large masses, up to 40 cm in diameter. The vast majority of mucinous tumors are benign (75%), 10% borderline, and 15% carcinomas. (8).
In our study, we used the criteria of consensus of the International Ovarian Tumor Analysis (IOTA) group (2000) to define terms, definitions, measurements on the sonographic features of adnexal tumors. The categories defining the adnexal mass, to be evaluated in the procedure, were the form of the lesion, its morphological features- qualitative and quantitative – and in the end to come to morphologic endpoints by B-mode imaging and end-points of vascularity and blood flow by color Doppler imaging (9).
As described in the IOTA group consensus, the five simple rules to predict malignancy (M-rules) were applied. For the ultrasound investigation of benign tumors, five simple rules were also suggested. By using these criteria, the IOTA group reported a sensitivity of 93%, a specificity of 90%, a positive likelihood ratio (LR+) of 9.45 and a negative likelihood ratio (LR−) of 0.08 (9).
Table 1. IOTA Group ultrasound rules to classify masses as benign (B-rules) or malignant (M-rules)
| B-rules | M-rules |
|---|---|
| Unilocular cysts | Irregular solid tumor |
| Presence of solid components where the largest solid component <7mm | ascites |
| Presence of acoustic shadowing | At least four papillary structures |
| Smooth multilocular tumor with a largest diameter<100mm | Irregular multilocular solid tumor with largest diameter>100mm |
| No blood flow | Very strong blood flow |
Rule 1: If one or more M features are present in absence of B feature, mass is classified as malignant.
Rule 2: If one or more B features are present in absence of M feature, mass is classified as benign.
Rule 3: If both M features and B features are present, or if no B or M features are present, result is inconclusive and second stage test is recommended.
As far as the tumor marker examination is concerned our literature study concluded that the serum of CA-125 assay has not to be undertaken in all premenopausal women when an ultrasonographic of simple ovarian cyst has been made. Lactate dehydrogenase (LDH), α-FP and hCG should be measured in all women under age of 40 with the complex ovarian mass because the possibility of germ cell tumors (10).
Table 2. Tumor markers test in correlation with ovarian neoplasms
| Tumor markers | Histopathological findings |
|---|---|
| CA-125 | Epithelial ovarian tumor |
| CA-19-9 | Mucinous epithelial ovarian tumor |
| LDH | Dysgerminoma |
| AFP | Endodermal sinus tumor |
| hCG, hPL | Choriocarcinoma, PSTT |
| Inhibin A | Granulosa cell tumor |
CA-125 is elevated :
| 1% healthy individuals | Liver disease | Hypothyroidism |
| Myomas | Endometriosis | PID |
| Adenomyosis | Peritonitis | Normal pregnancy |
| Benign ovarian tumors | Pleural effusion |
* Royal College of Obstetrics and Gynaecologists; RCOG/BSGE Joint Guideline I: RCOG; 2011
Our study suggests that the technique of intra-ovarian direct trocar penetration and drainage for access prior to laparoscopic surgery for giant ovarian cyst is effective. This novel procedure provides shorter operation time, less complication and less spillage of the cyst’s liquid in the intraabdominal cavity.
The length of stay in the hospital after the procedure was one day in all three cases reported. As best of our knowledge this recent technique has never been reported in the literature.
Table 3. Cases resume of direct trocar penetration and drainage of giant ovarian cysts
| No. | Age | Preoperative diagnosis | IOTA criteria | Histopathological finding | Laparoscopic surgery | Operation time (minutes) | Hospital discharge |
|---|---|---|---|---|---|---|---|
| 1 | 31 | right giant ovarian cyst and uterine fibroid | benign | non-papillary serous cystadenoma | unilateral salpingoophore ctomymyomectomy chromotubation | 78 | 2 days |
| 2 | 41 | right ovarian endometrioma | benign | endometriosis | unilateral partial oophorectomy | 65 | 2 days |
| 3 | 35 | giant left ovarian cyst | benign | endometriosis | left salpingoophore ctomy | 70 | 2 days |
Conclusion
The intra-ovarian direct trocar penetration and drainage technique prior to laparoscopic surgery for giant ovarian cysts as a novel approach did show great benefits for the patients with less complications, less pain and shorter hospital stay. The procedure is safe, applicable, reliable and effective in the management of benign giant ovarian cysts in patients with no history of previous laparotomy . The technique could be used as one alternative new approach in the management of giant benign ovarian neoplasms. However more of future studies are needed applying this procedure to enrich the safe, effective and efficient operative laparoscopy with the aim to provide better clinical care for the patients.