Authors / metadata
Introduction
At our reference centre of hysteroscopy in Constantine Algeria we perform more than a thousand hysteroscopies per a year most of these are office procedures.
The complication rate for all the procedures is about 05 per thousand failures and 15 per thousand incomplete diagnosis and operative procedures, 04 cases of vagal reactions had to be managed, 59 per thousand have had a painful hysteroscopy up to a score of 07/10 (Analogue Visual score 1 – 10 where the patients rate there pain) no premedication nor analgesics were used, the local vocal was the sole method applied (1).
All the procedures were performed by vaginoscopy (2) using 05 mm and 04mm Bettocchi hysteroscopes a Gubbini 14.5 French resectoscope and 05 French bipolar needle, also hardly ever a resectoscope of 18,5 was used when the cervix allowed an easy passage.
Case report
A very rare complication is described as a case report.
A woman aged 41, married with a story of one caesarean section four years ago and one year later she had an incomplete abortion followed by a curettage, a false route was made accidently during the curettage as described in her operatory protocol.
From that time the patient had probably developed synechia because her symptoms of hypo and oligomenorrhea. An hysterosalpingography was performed one year ago and failed because of the possible passage in the old false route. Her ultrasound showed a normal shaped uterus where the endometrial lining is seen. She was referred to the centre in order to treat the possible synechia (3).
At first, on day nine of her cycle, an office hysteroscopy was performed and the scar of the cervical false passage was clearly visible. However, a successful passage into the uterine cavity through the cervical canal averred to be possible. The endometrium was clearly seen and the uterine cavity did look tunnel shaped without seeing the two ostia possibly covered by the evident fibrotic tissue. The procedure was stopped when the patient started to feel some pain when a trial to cut this fibrotic tissue was started.
Four months later (because of Covid-19 pandemic) she was scheduled for hysteroscopy under spinal anaesthesia.
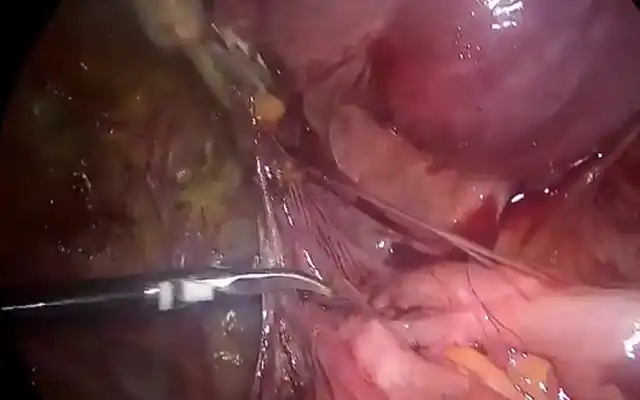
At the theatre a Bettocchi five mm hysteroscope was used and after getting into the cervical canal the scope did pass directly into and through the false passage to finish outside the uterus into the peritoneal cavity as witnessed by the intra pelvic fatty tissue clearly visible (4).
The procedure was stopped immediately and the patient was followed for 24 hours and she was discharged home in a very good clinical condition.
Seven days later the patient came back with an abnormal vaginal bleeding, vaginal and pelvic ultrasound did show a big hematoma in the broad ligament measuring some 15cm over 10 cm. the patient was hospitalized for a close follow up, her Haemoglobin (Hb) was at 11mg/dl at intake. She was placed under tow different antibiotics (cefalexin and metronidazole) since her first hysteroscopy.
One day later early in the morning the team was called in for an important vaginal bleeding and a low blood pressure, her Hb was 07mg/dl and the clotting tests were normal. The abdominal and vaginal ultrasound revealed no hematoma at all, so a decision to go to the OR and open the patient (the centre does not allow to perform laparoscopy when the blood pressure is down) was made. through the ancient Pfannenstiel the patient was opened and after adhesiolysis the peritoneum of the left broad ligament has just a bluish colour with the same findings behind the bladder. A bilateral uterine artery ligation was performed and an unusual cervical cerclage with Vicryl 1 in order to close the possible false route, the uterus had a normal aspect and a clear opening of the perforation couldn’t be found, a drain was brought in. A transfusion by three units of blood was made.
The follow up was normal for three days, and the patient was discharged home in a satisfactory clinical condition. A vaginal ultrasound was done three and five days after the second surgery and the situation did remain normal.
Aknowledgments: The author does thank Bruno van Herendael for his critical advise.