Authors / metadata
DOI: 10.36205/trocar2.2021002
Abstract
This article provides a Summary of ISGE Guidelines for the safety of trocar entry, one of the most dangerous steps in laparoscopic surgery.
Corresponding author: Dusan Djokovic, M.D. Ph.D; dusan.d.djokovic@nms.unl.pt
Introduction
The recommendations from the International Society for Gynaecology Endoscopy (ISGE) for safe laparoscopy entry were published in the European Journal of Obstetrics & Gynecology and Reproductive Biology in 2016 (1). This article aims to summarize these guidelines authored by the ISGE Task Force for Abdominal Entry (Dusan Djokovic, Janesh Gupta, Viju Thomas, Peter Maher, Artin Ternamian, George Vilos, Alessandro Loddo, Harry Reich, Ellis Downes, Ichnandy Arief Rachman, Lotte Clevin, Mauricio S. Abrao, Georg Keckstein, Michael Stark and Bruno J. van Herendael) and provide updates arising from posterior publications.
Materials and Methods
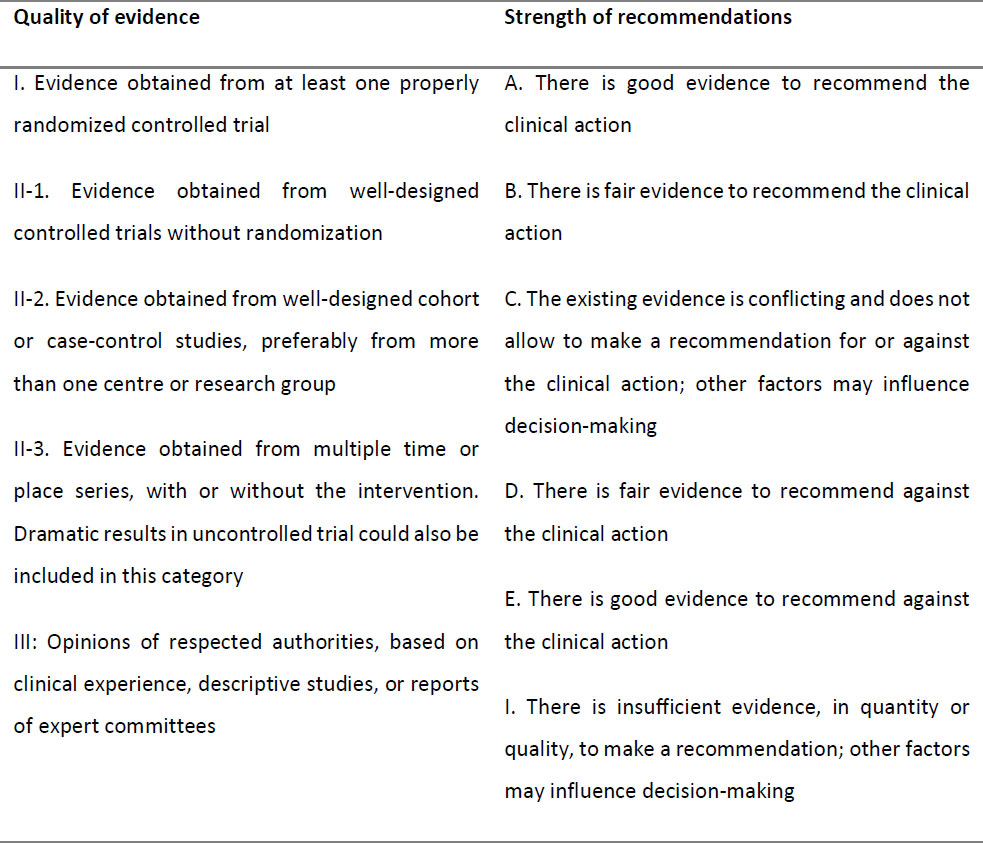
The ISGE Task Force for Abdominal Entry performed a broad literature search from Medline, PubMed, Cochrane Database as well as international and national guidelines and established evidence-based recommendations graded by the level of evidence, using the approach proposed by U.S. Preventive Services Task Force (Table 1). The same methodology was repeated in this paper preparation, in order to find the latest literature and guidelines on laparoscopic entry.
The ISGE recommendations on safe laparoscopic entry
Several methods are used to access the peritoneal cavity during laparoscopic surgery. The most commonly engaged are the closed (classic or Veress needle) technique, the open (Hasson) technique and the direct trocar insertion method. Based on available evidence, none of these approaches appears superior over another and can be recommended as the gold standard technique (1, 2).
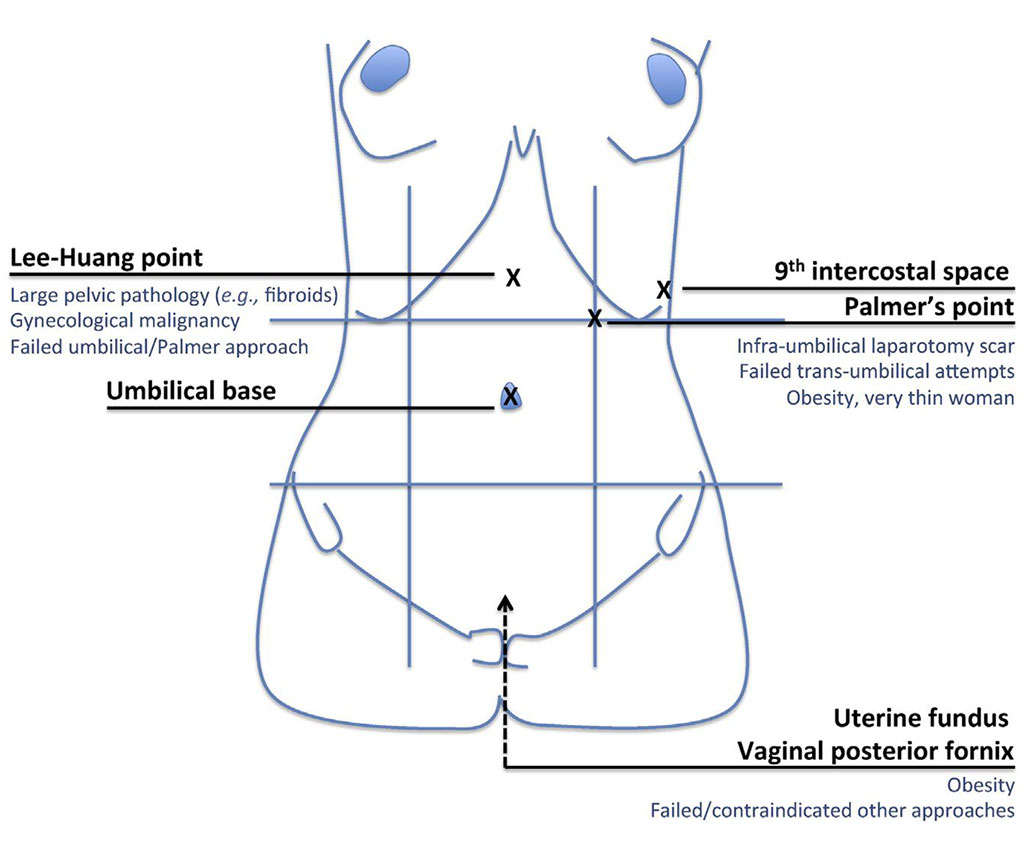
Regarding the closed technique, the most commons sites of entry are the umbilical base or the left upper quadrant (LUQ)/Palmer’s point which is recommended if trans-umbilical entry fails after three attempts or there are umbilical abnormalities such as a hernia or suspected/known adhesions that contra-indicate trans-umbilical entry (Grade II-2/A); alternative sites (e.g. Lee-Huang point, trans-uterine and posterior vaginal fornix; Figure 1.) should be considered if both umbilical and LUQ insertion fail (Grade I/A) or in obese women (1). The elevation of the lower anterior abdominal wall during the Veress needle trans-umbilical insertion is not recommended as a routine practice since it does not reduce the risk of iatrogenic injuries and increases failed entry rate, particularly in obese patients (Grade II-2/B). When inserting the Veress needle, the angle should be adjusted to the patient’s body mass index (BMI), from 45º in women with normal weight to 90º in obese patients (Grade II-2/B). To confirm the correct placement of the Veress needle, the only reliable indicator is Veress Intraperitoneal Pressure (VIP) below ≤ 8 mmHg. Other Veress placement tests (e.g. double-click or saline hanging-drop) are not required while swinging the needle is hazardous and must be avoided (Grade II-1/A). To ensure adequate pneumoperitoneum, transient high intraperitoneal pressure entry of 25 mmHg in healthy women with immediate intraperitoneal pressure, reduction to 12-16 mmHg upon completion of all trocar insertions, is suggested (Grade II-1/A). Primary trocar should be inserted in a controlled, two-handed manner, in the same direction as the Veress needle while secondary trocars should be placed under direct vision, at a 90° angle (perpendicular) to the abdominal wall, in a controlled, screwing manner.
The open technique is a mini-laparotomy performed at the umbilical level that permits the insertion of a cannula, CO2 insufflation and a laparoscope placement in a direct manner. It may be considered as an alternative to the closed technique, especially in patients with a history of previous surgeries or after other entry techniques fail. It is associated with a reduced rate of failed abdominal entry without a significant difference in visceral or vascular injury rates (Grade II-2/C). Factors that may limit the use of this technique include its relative complexity, patient obesity and struggle to maintain pneumoperitoneum.
An alternative method is the direct abdominal trocar entry, which provides a quick abdominal access and results in fewer extra-peritoneal insufflations and failed entries in comparison with the Veress needle entry (Grade I/A). Its general use cannot be recommended until more reliable evidence is available (2).
Concerning the optical trocar (direct vision) entry, which approaches the peritoneal cavity under direct monitor view, it presents risk of iatrogenic injuries similar to the conventional open (Veress needle) or closed (Hasson) entry techniques (Grade II-2/B). Based on available evidence, published data, expert opinion and FDA assertion, the threaded visual cannula entry systems appears to be a safe alternative for laparoscopic entry (Grade II-2/B).
In the particular case of a pregnant patient, laparoscopic interventions can be safely performed in any trimester of pregnancy, but the entry point should be adapted to the height of the uterine fundus and previous incisions, particularly in second or third trimester pregnancy (Grade III/C). Any entry technique may be performed, but if the closed entry is chosen primary entry via the Palmer’s point is recommended. The open technique and the closed entry via Palmer’s point are preferred in the patients with BMI <18 kg/m2 while the closed technique and visual entry via the umbilicus or Palmer’s point are preferred in the obese patients with BMI >40 kg/m2 (Grade III/D).
Discussion and Conclusions
Laparoscopy is currently the preferred approach for diagnostic or therapeutic interventions in gynaecology when compared to open abdominal surgery as it reduces hospital stay, is less disabling, presents lower risk of minor complications and is more cost effective (3). Approximately half of the laparoscopic complications occur during the abdominal entry (1). It is essential to engage a methodical approach when entering the abdomen, choosing an appropriate location for the initial entry as well as the preferred entry technique. There are no gold-standard methods for the entry, though the most commonly used entry site and method are, respectively, the umbilical base and the Veress needle/classic entry (4).
Last decade’s clinical practice and research provided evidence for the ISGE to establish safety-promoting criteria that allow the conducting of common alternatives for laparoscopic abdominal entry. Nevertheless, the majority of trials present low quality evidence, being inadequately powered (small sample sizes and very low event rates) to detect statistically significant differences between the available techniques (1, 2). Publications posterior to the ISGE guidelines, including the last (2019) Cochrane systematic review, have not added any new updates that should redirect the recommendations established by the ISGE Task Force. The ISGE document published in 2016 remains valid and is one of the most comprehensive sets of guidelines on this topic. Considering that current evidence is insufficient to praise one entry method over the others, the choice of one technique, entry position and type of instrumentation with which the gynaecological surgeon feels comfortable for most procedures represents a safe and effective practice. Nonetheless, the surgeon should be well versed to use an alternative technique if the prior approach presents major risk of complications or fails (1). Future well-designed studies, with larger samples and less bias, might provide new insights in this issue.
Sources / references
Table 1: Evidence quality grading and classification of recommendations (in accordance with the system adopted by the U.S. Preventive Services Task Force) (reproduced with permission from Djokovic et al. (1))
Abbreviations: ISGE – International Society for Gynaecology Endoscopy; LUQ – left upper quadrant; VIP – Veress Intraperitoneal Pressure
Figure 2: Umbilical and alternative Veress needle insertion sites with respective indications (reproduced with permission from Djokovic et al. (1)).