Authors / metadata
DOI: 10.36205/ trocar3.2022006
Abstract
Hysteroscopy is not yet widely used in developing countries leading to incorrect diagnosis and no proper treatment in some conditions. Office hysteroscopy favors the lowering of the global cost, and this is very interesting to boost its practice in developing countries, as for the same symptom, uterine findings can vary widely from a setting to another. The aim of the study was to describe the epidemiologic profile and hysteroscopic findings in patients who underwent an office hysteroscopy.
Methodology: A cross-sectional study was conducted on medical records of 1022 patients who underwent an office hysteroscopy at Clinic d’Or in Kinshasa, DR Congo from March 2018 to August 2022.
General characteristics of patients, indications of hysteroscopy, characteristics of the procedure and hysteroscopic diagnosis were analyzed. All hysteroscopies were practiced using a 5 mm total diameter Bettocchi Hysteroscope, with 5 FR operating channel and 2.9 mm, 30-degree scope in an office setting. Pain was evaluated using a simple numeric pain scale. Data were analyzed using SPSS 21.0 and descriptive statistics were computed. The test was statistically significant for a p value < 0.05.
Results: Patients’ age was 37.5 ± 7.6 years. Seventy-four percent of patients had university level and 79.4% of them were married. Sixty-two percent (61.7%) had at least either one abortion or one miscarriage. The infertility workup was the main indication of hysteroscopy (54.8%) followed by abnormal uterine bleeding (20.3%). The vaginoscopic approach was used almost in all cases (99.7%), and a half (51.8%) did not have pain. Fibroids, endometrial polyps and uterine adhesions were the most common conditions with respectively 15.7 %, 14.5 % and 14.3 %. Patients with history of abortion/miscarriage had more cervical stenosis and more intrauterine adhesions than others (p=0.000). Adhesiolysis for intrauterine adhesions (97.6% of all adhesions) and polypectomies (98.8% of all polyps) were performed.
Conclusion: Office hysteroscopy is performed mostly in patients who are at their thirtieth, with university level, non-menopausal and married. The main indications are infertility and abnormal uterine bleeding. A great number of the most common findings can be treated in the office setting in a “see and treat” approach. This could help in developing the practice of hysteroscopy in low resource settings.
Introduction
Hysteroscopy is a modern procedure that is not yet widely used in the developing world. Being an endoscopic technology, the limitation due to investment cost, training, and low access of patients because of the cost of the procedure, hampers its spread in low-income areas.
For decades, hysteroscopy has been qualified as a procedure “seeking indications”, but nowadays, it is being considered by many authors as a first line procedure in exploring and treating intrauterine pathologies (1, 2). This has been made possible by the development of instrumentation, energy sources and distension medium (3). Being practiced for many years exclusively in operating rooms (4), thanks to the development of instrumentation and experience of practitioners, the procedure has been brought to office setting without analgesia, without anesthesia, improving then its implementation. In fact, it is widely practiced in a routine basis mostly in developed countries and some Asian countries. In Romania, Stefanescu et al. (5) performed 3220 procedures, all indications, in one facility within a period of three years and half. Capmas et al (6), in France, reported 2402 diagnostic hysteroscopies within a period of four years. This routine practice facilitated the production in the literature of many studies addressing various aspects of hysteroscopy.
Despite the trend of developing the practice of hysteroscopy, the situation in many developing countries and particularly in Sub Saharan Africa has not substantially evolved. This fact induces an inaccurate evaluation of intrauterine conditions in these countries, leading to overtreatment in some cases or undertreatment in other cases. Otherwise, hysteroscopy being the gold standard in evaluating the uterine cavity pathologies, it should be the tool to guide their management.
It has been shown that hysteroscopic findings according to some complaints vary widely from an area to another depending on epidemiology of considered pathologies. These variations were reported by many authors. Ajayi et al. (7), comparing hysteroscopic findings between Nigerian and Indian infertile women, noted the predominance of submucous fibroid and intrauterine adhesions in Nigerian whereas there were more polyps and uterine septa in Indian. In Kenya, Parkar et al. (8), in a study on 463 hysteroscopies performed for all indications, reported that submucous fibroid and endometrial polyps were the predominant findings.
In the Democratic Republic of Congo, no study has been yet conducted on hysteroscopy. Results from such study will help to guide the management of intrauterine conditions based on local data. The objectives of the present study were to describe sociodemographic and clinical characteristics of patients, the hysteroscopic particularities and findings and to analyze association between patients’ characteristics and hysteroscopic findings.
Methods
We conducted a cross-sectional study collecting data of patients who underwent office hysteroscopy between March 2018 and August 2022 in “clinic d’Or”; a private clinic in Kinshasa, the Democratic Republic of Congo (DRC). Patients were coming from internal practice in the Clinic but also some were referred from colleagues in the City. In a routine basis, before each procedure, the history of patient is taken and is recorded on an appropriate sheet that is then referred to when elaborating the final report. Information on the procedure is provided to each patient and a written consent is signed. A nurse accompanies the patient during the exam and keeps her discussing as often as possible. Neither analgesia nor anesthesia is offered in a systematic approach and there is no use of prostaglandins for facilitating cervical navigation by the hysteroscope.
General characteristics of patients, indications of hysteroscopy, characteristics of the procedure and hysteroscopic diagnosis were analyzed. All hysteroscopies were practiced by two experienced practitioners using a 5 mm total diameter Bettocchi Hysteroscope, with 5 FR operating channel and 2.9 mm, 30-degree scope in an office setting. In few cases, the traditional approach was applied using a vaginal speculum and a Pozzi tenaculum allowing the insertion of the hysteroscope directly into the cervical canal. In the vaginoscopic approach, the hysteroscope is inserted into the lower vagina and under hydro-distension with the distension medium, the navigation begins at that point to reach the external cervical os. Once in the cervical canal, the navigation continues to allow for passage into the cervical canal and uterine cavity through gentle movements (9).
Pain was evaluated using a simple numeric scale (SNS). Patients were asked to evaluate pain using a scale from 0 to 10; 0 representing the absence of pain and 10 the most severe one. We established a score and categorized patients in groups: No pain (0), Mild pain (1 – 3), Moderate pain (4 – 6) and severe pain (7-10). Five patients were offered general anesthesia on their demand as they didn’t want to be lucid during the procedure. Gravidity was grouped in Nulligravida (no prior pregnant) paucigravida (1 to 3 pregnancies) and multigravida (from 4 pregnancies). Parity groups were: Nulliparous (no delivery yet), pauciparous (1 to 3 deliveries), multiparous (from 4 to 5 deliveries) and great multiparous (from 6 deliveries).
Data were analyzed using SPSS 21.0 and descriptive statistics were computed. Comparison of proportions between groups was achieved using Pearson Chi square test. The test was statistically significant for a p value < 0.05.
Results
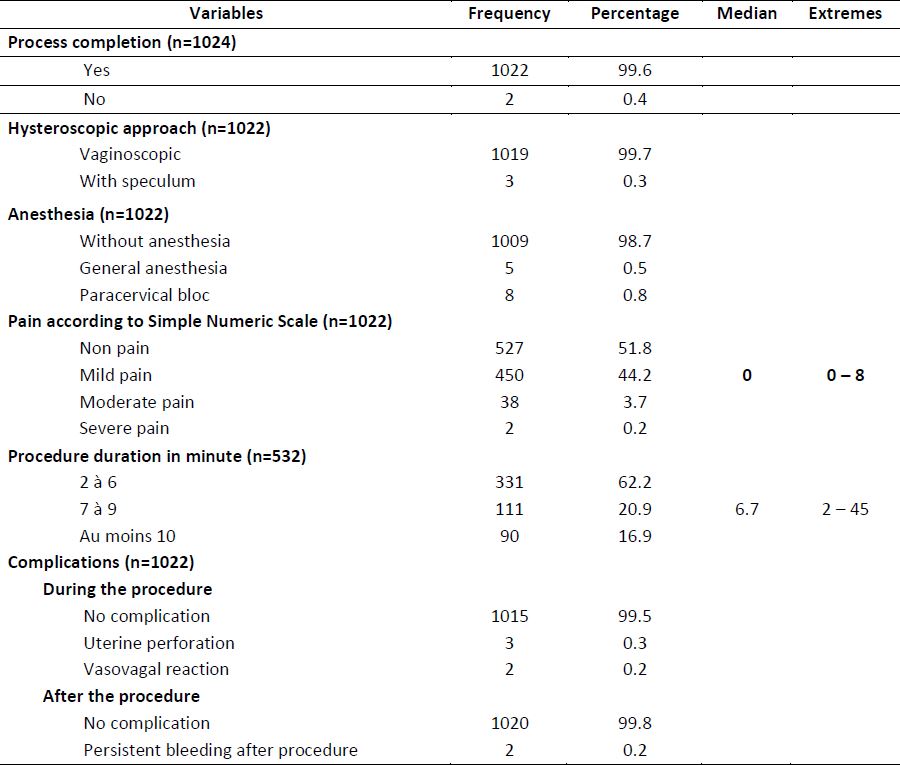
Overall, 1024 procedures in an office setting were practiced from March 2018 to August 2022. Two patients were excluded because of the uncompletion of the procedure (table 2) due to a highly fibrotic cervix, necessitating dilatation. Patients who experienced vasovagal reaction did undergo the procedure and were then included in the study.
Patients’ characteristics
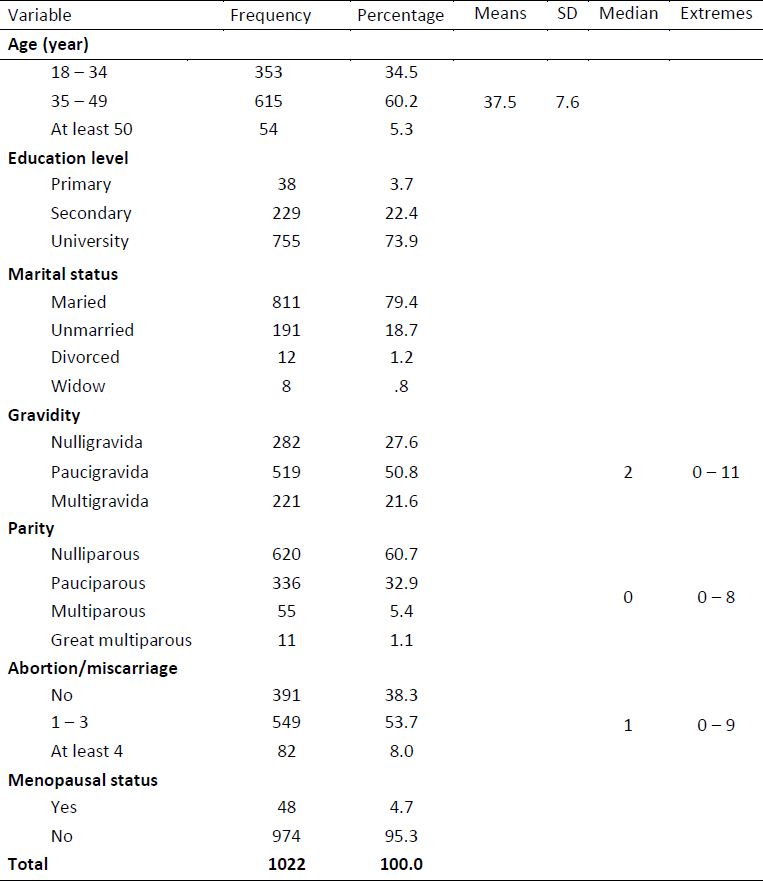
Patients’ age was 37.5 ± 7.6 years and 94.7% had from 18 to 49 years. Seventy-four percent of patients had university level and 79.4% of them were married. Regarding their history, 27.6% of patients were nulligravida with median gravidity of 2 and extremes from 0 to 11. Patients were nulliparous in 60.7% of cases with a median parity of 0 and extremes from 0 to 8. Sixty-two percent (61.7%) had at least either one abortion or one miscarriage with a median of 1 and extremes from 0 to 9 and 4.7% were menopausal (table 1).
Procedure description
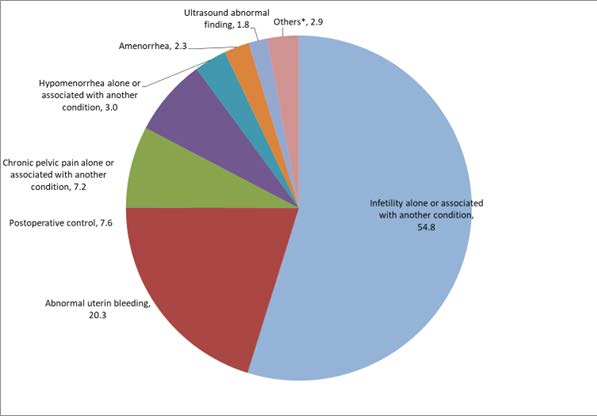
Hysteroscopy was performed for infertility in 54.8%, for abnormal uterine bleeding in 20.3% and as a postoperative uterine cavity control procedure in 7.6 % of cases (figure 1). Considering the procedure characteristics, almost all hysteroscopies (99.7%) were performed using a vaginoscopic approach (without speculum, without tenaculum), 98.7% were conducted without anesthesia and less than 1 % (0.5 %) of patients benefited from general anesthesia because they didn’t want to be lucid during the procedure. Patients reported no pain in 51.8 % and mild pain in 44.2 %. The median pain score was 0 with extremes from 0 to 8 according to simple numeric scale. The median duration of the procedure was 6.7 minutes varying from 2 to 45 minutes and 83.1 % of procedures varied from 2 to 9 minutes (table 2).
In all, complications were noted in seven patients (0,7%). Five patients had complications during the procedure, and this has been dominated by uterine perforation (0.3%) which occurred during adhaesiolysis.
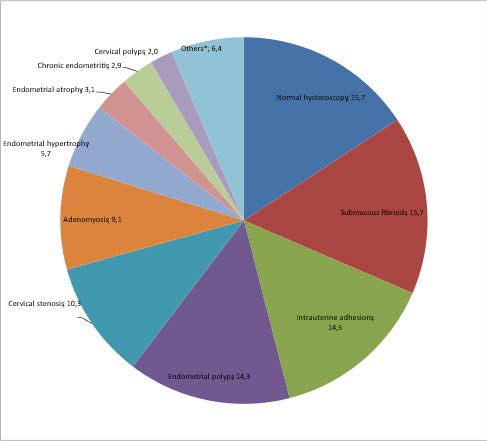
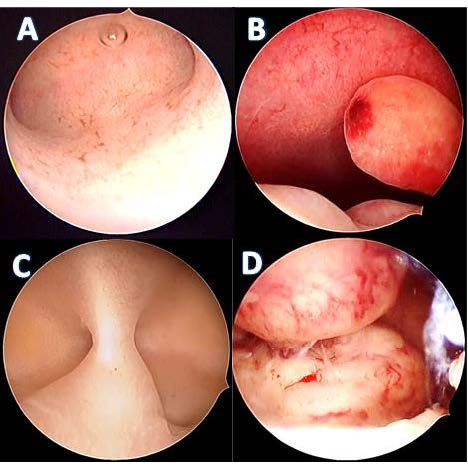
The hysteroscopy showed a pathology in 84.3% and the five main hysteroscopic findings were submucous fibroids (15.7%), intrauterine adhesions (14.5%), endometrial polyps (14.3%), cervical stenosis (10.3%) and adenomyosis (9.1%) (figure 2 and 3).
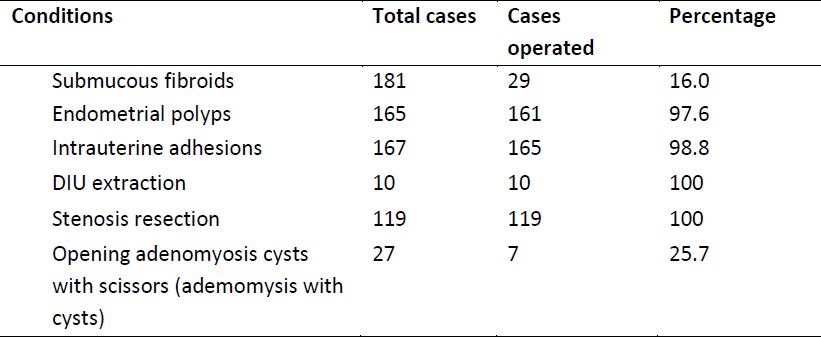
Operative procedures during office hysteroscopy
During this period, 29 myomectomies (16%), 161 polypectomies (97.9%) and 165 intrauterine adhesiolyses (98.8%) were performed (table 4) in a “see and treat” approach. These operative procedures were conducted using mechanical instruments (hysteroscopic 5 FR scissors and/or biopsy/grasper forceps) (table 4).
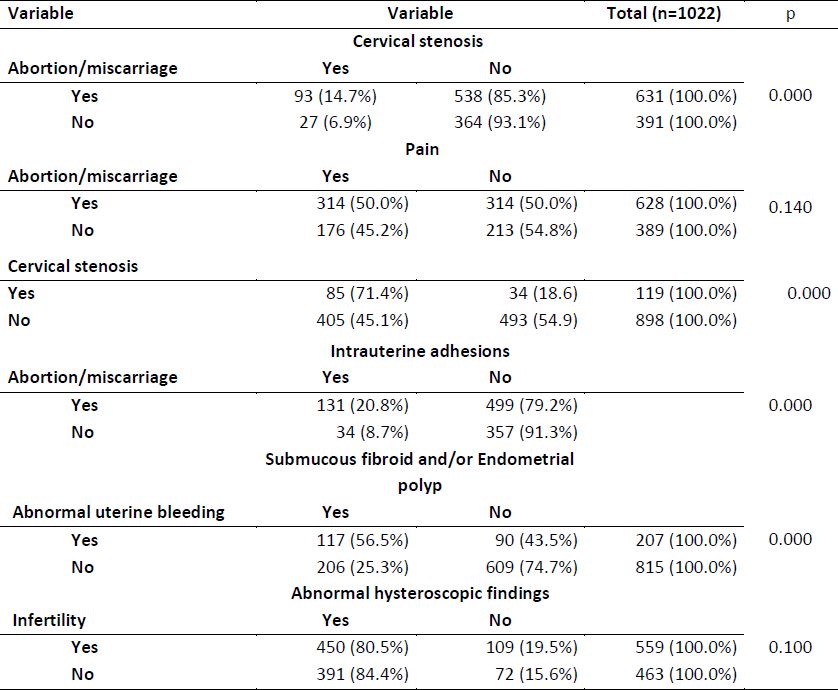
Associations between variables
Patients with history of abortion/miscarriage had more cervical stenosis (14.7%) and more intrauterine adhesions (20.8%) compared to those without this history (6.9% for cervical stenosis and 8.7% for intrauterine adhesions) (p = 0.000 for both) (table 3). Among patients with cervical stenosis, 71.4% experienced pain compared to 45.1% in the group without cervical stenosis and the difference between the two groups was statistically significant (p = 0.000). This study showed that patients with abortion/miscarriage history had more pain (50%) than others (45.2%) but it failed to establish a statistically significant difference (p=0.140).
Comparing patients with abnormal uterine bleeding to those without this complaint, the difference was statistically significant when taking in consideration the finding of submucous fibroid and/or endometrial polyp with respectively 56.5% and 25.3%. Hysteroscopic diagnosis didn’t differ in terms of abnormal findings when comparing patients with and without infertility.
Discussion
Indications
In literature, clinical presentations in patients benefiting from hysteroscopy are dominated by abnormal uterine bleeding with frequencies varying between 45 and 86,5% (10, 11).
In this study, hysteroscopic evaluation of the uterine cavity as infertility workup constituted the main indication (54,8%), and the abnormal uterine bleeding represented less than a half (20.3%). This result is different from those reported above but in accordance with 49,2% noted by Tangri et al. (12) in India. The difference could be related to the selection of patients in many studies and to the fact that routine evaluation of the uterine cavity even in conventional management or in In Vitro Fertilization is not uncontroversial. In fact, in the absence of suggesting complaints, ultrasound features or IVF failures, a systematic hysteroscopic evaluation of uterine cavity is not cost-effective (13, 14). Obviously, the debate still needs to be raised in our area on the usefulness and cost-effectiveness of routine hysteroscopic evaluation of uterine cavity in infertile women.
Hysteroscopic procedure
Almost all hysteroscopies were managed using vaginoscopic approach (99.7%). This result is in accordance with Pluchino et al. (15) in Italy (2010) and Stefanescu et al. (5) in Romania (2012) reporting respectively 90 % and 78 % of vaginoscopic approach. It differs from the 30% of vaginoscopic approach shown by Cooper et al. (16)in Great Britain (2013). This approach hasbeen widely recommended to allow moreprocedures in the office setting as it reduces thepatient discomfort induced by the speculum andthe tenaculum. But this is related to theexperience of practitioners and the policyregarding health insurance. In fact, in someareas, practitioners prefer to performhysteroscopy in the operating room, astraditionally, due to the lack of fiscal incentivesfor office procedures (17). However, it is obviousthat vaginoscopy, not only simplifies theprocedure, but lowers its cost and should berecommended particularly in low-incomecountries.
Pain during office hysteroscopy
Office hysteroscopy with vaginoscopic approach is well tolerated by patients as shown in the present study. In fact, 51.8% of patients had no pain and 44.2% reported to have experienced mild pain during the procedure. This is similar to the result published by Deffieux et al. (18) in France and also to the data in the literature.
The pain score did not display normal distribution because some operative procedures, producing more pain, were practiced. The median pain score was 0, varying from 0 to 8 out of 10. The experience of severe pain was less encountered compared to several studies in the literature. It was 0.2% in the present study, much lower than the 32.3% reported by de Freitas Fonseca et al. (19), the 20.4% by Bettochi et al. (20). and as reported by De Angelis et al. (21). This reality can reflect the disparity in relation to the perception of pain depending on the painful stimuli, the level of education, cultural factors, a previous bad experience in relation to pain and the circumstances of onset of pain (22). The question that should be asked is whether the patients in our setting are more resilient to pain than those studied in the above-mentioned publications. This question would raise a lot of speculation but deserves to be studied to adapt certain anesthesia protocol during hysteroscopy but also the caliber of the hysteroscope according to the characteristics of our populations in relation to pain.
The vagino-scopic approach, almost used in all cases but 3 in the present study, has been demonstrated to be associated with a statistically significance reduction in pain (9) and should be preferred in office setting. The knowledge of hysteroscopic anatomy (instrumentation and genital tract) is very crucial to allow a smooth navigation and avoid discomfort to patients (20).
Findings
Submucous fibroid was the main finding in hysteroscopy (15.7%) followed by intrauterine adhesions (14.5%), endometrial polyps (14.3%), cervical stenosis (10.3%) and adenomyosis (9.1%). Hysteroscopic findings vary from one study to another depending on the selection of patients and the epidemiology of pathologies in each area. In their study, Capmas et al. (6), noted submucous fibroid predominating, followed by endometrial polyps and intrauterine adhesions. Ajayi et al. (7) comparing infertile Nigerian to Indians patients, reported that intrauterine adhesions and submucous fibroid were the pronounced findings in Nigerians whereas in Indians, they noted that polyps and uterine malformations were dominating. In Kenia, Parkar et al. (8) found that submucous fibroid and endometrial polyps were the predominant pathologies.
In many studies and particularly in Africa, submucous fibroid, intrauterine adhesions and endometrial polyps are the main findings reported with different proportions. In sub-Saharan Africa, the racial disparity reported for fibroid; whose prevalence is 3 times higher in black women (23) and the prevalence of unsafe abortion could contribute to maintaining in top 2 or 3 the two main findings namely fibroid and intrauterine adhesions.
Adenomyosis had a significant proportion in the present study (9.1%). This should raise the question of its extent in our areas and its association with other forms of endometriosis. Cervical stenosis is another drawback of unsafe abortion and there was a statistically significant association to abortion/miscarriage (p=0,000) in the present study.
Operative procedures
In our practice, we apply a “see and treat” approach and that allowed us, in the present series, to perform some operative procedures mostly adhaesiolysis for intrauterine adhesions (97.6% of all adhesions) and polypectomies (98.8% of all polyps). Endometrial biopsy has not been considered as being an operative procedure. Several studies in the literature showed the great possibility of performing various hysteroscopic procedures in an office setting (24, 25) which drastically reduces the cost and promotes the extension of the practice, especially in low-resource countries.
Association
Regarding the associated factors, patients with a history of abortion had more cervical stenosis, those with cervical stenosis had more pain and this was statistically significant. Since all cervical stenoses were either resected with scissors or dilated with the tip of the hysteroscope or the jaws of the grasping forceps, the pain could be linked to this act and also to the loss of cervical smoothness related to fibrosis causing then pain when rotating to explore from one tubal ostium to another. The practitioner in our settings should learn how to manage cervical stenosis given that this pathology is frequent, especially in patients with a history of abortion. However, the history of abortion was not statistically associated with pain during hysteroscopy, probably because of not having differentiated abortions with dilation and curettage or aspiration from those without this treatment.
This study did not analyze other risk factors of pain during office hysteroscopy such as diabetes, age, previous curettage, dyspareunia, dysmenorrhea, hysteroscopist experience, anxiety and patient waiting time before the procedure (19, 26) Further specific studies will have to integrate these factors and analyze them to provide important information for the management of pain during office hysteroscopy in our environment.
Although the main pathological findings at hysteroscopy were uterine fibroids, intrauterine adhesions and endometrial polyps, which can to some extent lead to delayed conception or infertility, infertile patients did not have more abnormal findings than the others. This result may be supported by the predominance in Sub-Saharan Africa of tubal and peritoneal causes of infertility rather than uterine anomalies (27, 28).
Study limitations
Although the present study is the first in the DRC to address hysteroscopy and its sample size is large, it does have some limitations. On abortions, a clarification should be given regarding the practice of curettage. Surgical history, particularly caesarean section and myomectomy could be associated with certain findings such as intrauterine adhesions. Being a study of patients’ records, these details could not be retrieved mostly in patients coming from other colleagues. The analysis of factors associated with pain perception is another limitation that should be addressed in further studies.
Conclusion
Office hysteroscopy is a simple and acceptable procedure in experienced hands. It is very well tolerated even without analgesia or anaesthesia and the rate of complications is very low. This procedure is performed mostly in patients who are at their thirtieth, with university level, non-menopausal and married. The main indications are infertility workup and abnormal uterine bleeding. The experience of pain is less marked in patients and the most associated factor is the presence of cervical stenosis. A great number of the most common findings can be treated in the office setting in a “see and treat” approach and this could help in developing the practice of hysteroscopy in low-income settings. Further studies are therefore awaited to address various specificities of hysteroscopy to improve its performance in our setting.
Disclosure of interest; The authors declare that they have no competing interest.
References
Table 1. Patients’ characteristics
Figure 1: Proportions in percent of hysteroscopy indications in percent (n=1122)
Table 2. Characteristics of hysteroscopy procedure
Figure 2: Proportions in percent of hysteroscopic findings in percent (n=1150)
Figure 3: Some images of hysteroscopic findings. A: normal uterine cavity, B: endometrial polyps, C: intrauterine adhesions, D: submucous fibroids
Table 3. Association between some variables
Table 4. Operative procedures during office hysteroscopy