Authors / metadata
DOI: 10.36205/trocar4.2022003
Abstract
The paired uterosacral ligaments, important supporting structures of the uterus and the apical vagina, have been reported to be the most common side of deep endometriosis in pelvis. On transvaginal ultrasounds, they appear as hyperechoic stripes starting from the cervix with a semi-horizontal direction. A lesion is suspected when their regular or irregular hypoechoic thickening is visualized. This paper presents the ultrasound technique used in the author’s institution for the detection and analysis of the uterosacral ligaments. Knowing their location and ultrasound morphology can increase the detection rate of endometriosis and other lesions affecting the uterosacral ligaments.
Introduction
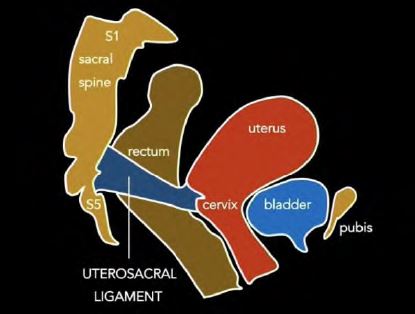
The paired uterosacral ligaments (USL), sometimes called the sacrouterine or rectouterine ligaments, are important supporting structures of the uterus and the apical vagina (1, 2). They extend posteriorly from the uterine cervix, define lateral boundaries of the rectouterine and rectovaginal spaces, and attach to the sacral spine indirectly, via the presacral fascia (1, 3), as schematically presented in Figure 1. However, there is conflicting information in the literature regarding the exact location of the USL insertion points at the pelvic wall, as previously summarized by Donaldson et al. (1).
Being composed of collagen, smooth muscle, autonomic nerves, blood vessels and lymphatic channels, the USLs are distinct from fibrous joint ligaments (4). They can be divided into three sections: distal cervical section (mainly comprised of smooth muscle), intermediate, and proximal sacral section (made predominately of looser connective tissue) (1, 3, 4). The inadequate use of the term “ligament” reflects the still insufficient knowledge of this important anatomical structure.
Weakened or damaged, the USL plays a significant role in the pathophysiology of pelvic organ prolapse (2). Besides, they can be affected by malignancy, especially by locally spreading cervical cancer (5). The USLs have been also reported to be the most common side of deep endometriosis (DE) in pelvis (6).
Over the past decades, various imaging techniques have been advocated for non-invasive (non-surgical) visualization of pelvic endometriosis to shorten the well-documented delay in the diagnosis (7). It has become widely accepted that transvaginal ultrasound (TVUS) can reliably diagnose DE in pelvic structures (8). Contrary to the long-standing belief that the USLs can be only seen on TVUS if they bear a lesion or if there is a fluid in the pouch of Douglas, the sonographic visualization of normal USL (the proximal section) is possible (9). This article aims to present the technique used at the author’s institution for the detection of the USLs.
Material and Method
For this demonstration, a female volunteer of reproductive age was selected, in whom normal USLs were observed by TVUS. Subsequently, a patient diagnosed in our Gynecological Ultrasound Unit with a DE lesion of the USL, who accepted to participate in the project, was included for comparison. Scanning was performed in both cases using an Aplio i700 ultrasound machine (Canon Medical Systems Ltd).
Results
TVUS technique to identify and analyze the USLs
To visualize and analyze the USLs, according to our technique, the following steps are performed:
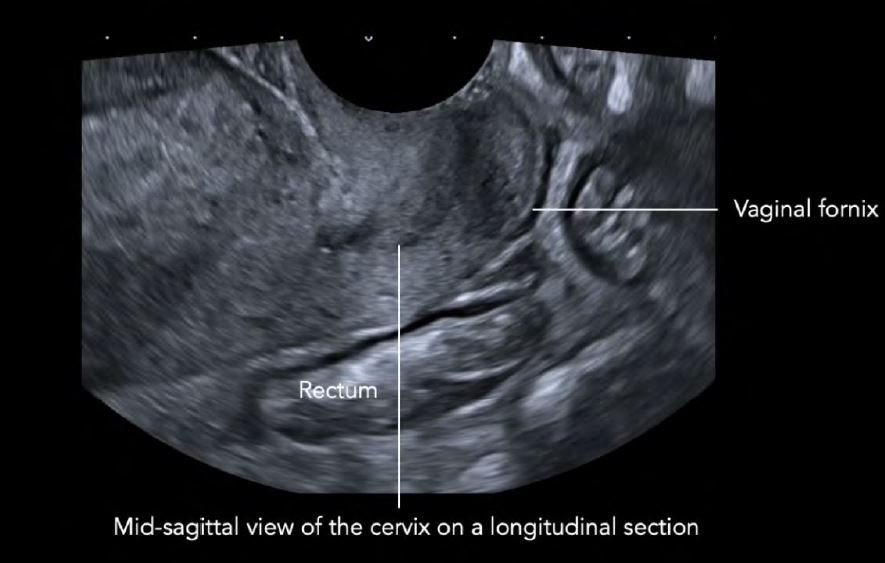
1.The TVUS probe is inserted into the anterior vaginal fornix to reach a mid-sagittal view of the cervix ona longitudinal section (Figure 2).
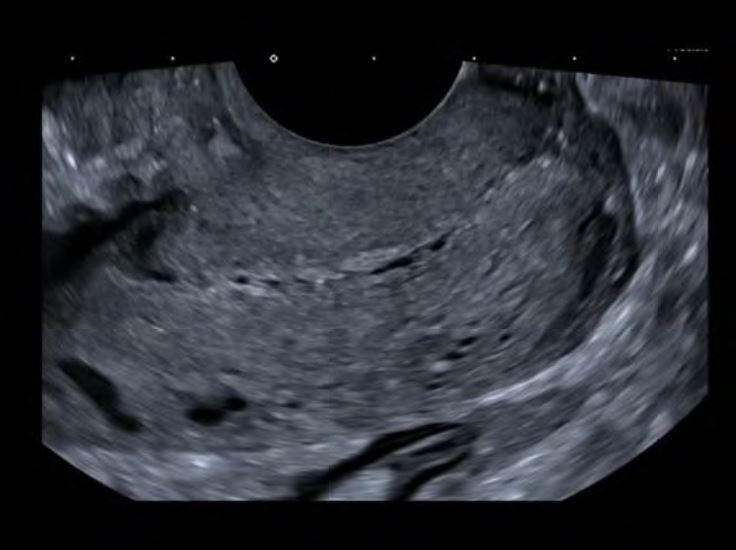
2.The penetration depth is adjusted so that the cervix fills 2/3 of the screen (Figure 3).
3.In order to obtain a transvers section of the cervix, the probe is rotated for 90o. (Figure 4).
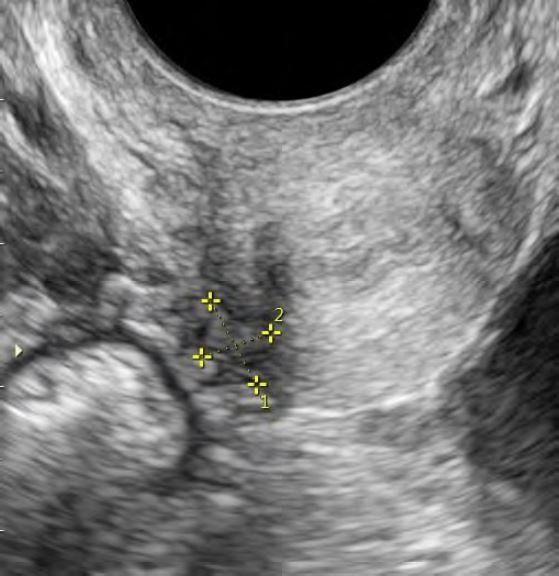
4.Then, the probe is directed laterally (and slightly posteriorly) until the hypoechoic structuresrepresenting uterine vessels are visualized (Figure 5).
5.The USL appears posteriorly to the uterine vessels, as a hyperechoic stripe starting from the cervix witha semi-horizontal direction (Figure 6).
6.The probe can be rotate by a few degrees in order to visualize the US on a longitudinal section.
7.The same maneuver is performed on contralateral side to identify the contralateral USL (Figure 7).
Normal USLs are homogenous and hyperechoic (Figures 5 and 6). While the medial portion of the USLs can be easily identified during TVUS, the most lateral portion fades into the presacral fascia, to be inserted via this fascia into the sacrum. On their way, USLs pass medially to the ureters and laterally to the rectum.
A DE lesion appears as a regular or irregular, generally hypoechoic thickening/nodules within the hyperechoic USL (Figure 7). Site-specific tenderness of the USLs should be examined and documented, independently if a lesion is observed or not (10, 11). Observed lesions compatible with DE should be measured in three orthogonal planes (10, 11). The USL DE nodule can be classified as: type 0 – confined to the USL (no infiltration into parametrium or torus uterinus); type 1P – partially infiltrating parametrium (>50% of DE nodule within USL); type 1T – partially infiltrating torus uterinus (>50% of DE nodule within USL); type 2P – significantly infiltrating parametrium (<50% of DE nodule within USL); type 2T – significantly infiltrating torus uterinus (<50% of DE nodule within USL) (9). The evaluation of the ureters should be done in the patients with the USL/parametrial nodules, as well as in all patients with suspected or known endometriosis.
Superficial USL endometriotic lesions (usually small, only a few millimeters in diameter) can be visualized if there is endogenous intraperitoneal fluid (6). They also can be visualized by saline sonoPODography, as previously described (12).
Video
Discussion
This article demonstrates that it is possible to visualize normal and uterosacral ligaments affected by endometriotic lesions using TVUS. They should be systematically examined. Chapron et al. observed USL DE in 69.2% of patients with DE (13). Reidet et al. reported that in women with endometriosis who underwent laparoscopy, 35% had isolated superficial endometriosis, while 33% had DE (14).
The International Deep Endometriosis Analysis Group (IDEA) proposed a systematic approach to sonographic evaluation of the pelvis in women with suspected endometriosis (10). The International Society for Gynecologic Endoscopy (ISGE) established the recommendations for structured reporting of dynamic ultrasound findings, promoting the practice of standardized, comprehensive and systematic evaluation and reporting of pelvic endometriosis (11). In addition to the technique presented here, other ultrasound approaches for visualization and assessment of USL have been published (6, 9). Further studies are needed to show whether the different techniques have comparable accuracy.
In a prospective international pilot study, Leonardi et al. evaluated the diagnostic accuracy of transvaginal ultrasound for the detection of endometriosis using the IDEA approach (15). The overall performance of TVUS for DE, based on surgical visualization as the reference standard, was as follows: accuracy 86.1%, sensitivity 88.4%, and specificity 78.8%. However, for right/left USL DE, TVUS accuracy was 65.2%/72.2%, sensitivity 49.2%/58.7%, and specificity 77.8%/83.7%. Thus, the IDEA consensus methodology provides strong diagnostic accuracy for TVUS assessment of DE overall, but efforts should be made to improve USL DE detection rates. This can be achieved through operator training. The technique presented here could be useful, as it demystifies the USL visualization and analysis in a relatively simple and straightforward way.
Conclusion
On TVUS, the paired USLs appear as hyperechoic stripes starting from the cervix with a semi-horizontal direction. If a regular or irregular, generally hypoechoic thickening is visualized, a lesion is suspected. The knowledge of the USL location and ultrasound morphology may increase the detection rate of (endometriotic) lesions affecting these structures.
References
Figure 1. Schematic representation of the right USL in the female pelvis (adapted from Donaldson et al. 2021, (1))
Figure 2: TVUS technique for the detection and analysis of the USLs: placement of the TVUS probe in the anterior vaginal fornix
Figure 3: TVUS technique for the detection and analysis of the USLs: adjustment of the penetration depth (cervix fills 2/3 of the screen)
Figure 4. TVUS technique for the detection and analysis of the USLs: the TVUS probe 90º rotation
Figure 5: TVUS technique for the detection and analysis of the USLs: the TVUS probe lateral pointing (visualization of the left USL)
Figure 6: TVUS technique for the detection and analysis of the USLs: the same maneuver presented in Figure 5 performed on the contralateral side (visualization of the right USL)
Figure 7: TVUS showing an endometriotic lesion affecting right USL