Authors / metadata
DOI: 10.36205/trocar1.2023014
Abstract
Diagnostic hysteroscopy is associated with less complications as compared to operative hysteroscopy, but one should remain vigilant about any complications that may occur as it may be lethal. The main purpose of this paper is to summarize the complications of diagnostic hysteroscopy and its diagnosis, the necessary preventive measures and management according to the available papers through a non-systematic review of the literature.
Outcome: Perforation being most common complication of diagnostic hysteroscopy can be managed either conservatively or laparoscopically. The other serious complications such as fluid overload, electrolyte imbalance and air embolism may be associated with the diagnostic hysteroscopy.
Conclusion: The gynecologists should be alert in order to assess, prevent and manage various complications associated with diagnostic hysteroscopy. The focus should be on proper patient selection, appropriate surgical technique and good instruments, so that the complications could be avoided.
Introduction
Diagnostic hysteroscopy is considered to be a safe procedure as it is associated with minimal complications. Hysteroscopy is gaining popularity amongst the gynecologists as a diagnostic and therapeutic tool for various gynecological pathologies such as polyps, myoma, intrauterine adhesions (IUA), uterine anomaly, infertility and cervical pathology etc. It is very important to prevent, recognize and appropriately manage complications associated with hysteroscopy. Disregarding contraindications and/or the appropriate technique of the procedure can lead to complications in hysteroscopy.
The main purpose of this non-systematic review of the literature is to summarize the complications of diagnostic hysteroscopy as well as its diagnosis and management according to the available data.
Various complications associated with diagnostic hysteroscopy
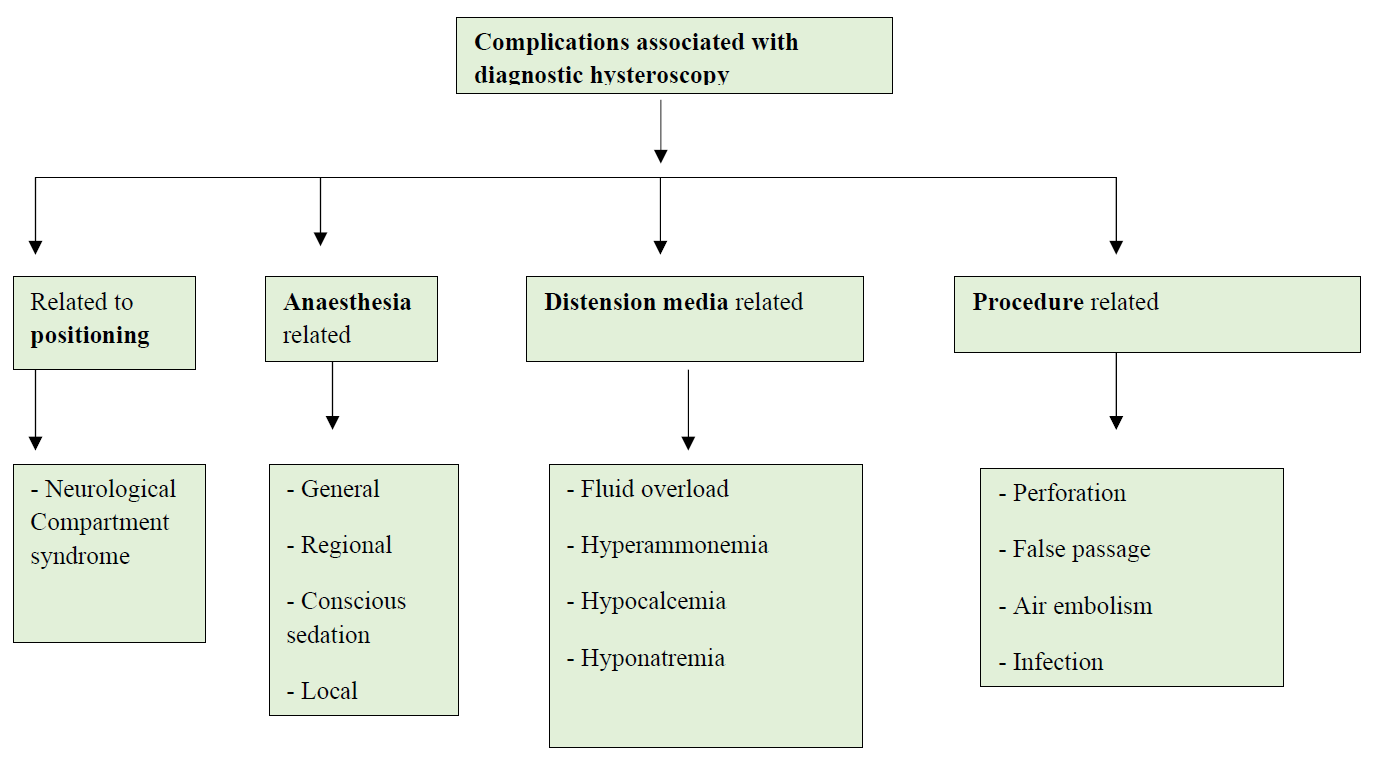
Diagnostic hysteroscopy is a relatively safe and well-tolerated procedure as compared to any other invasive gynecological procedure. Following are the rare complications associated with the procedure and if left unnoticed can become lethal (figure 1). Hence one should be vigilant and efficient enough to prevent them or if in case it occurs recognize them immediately and manage accordingly.
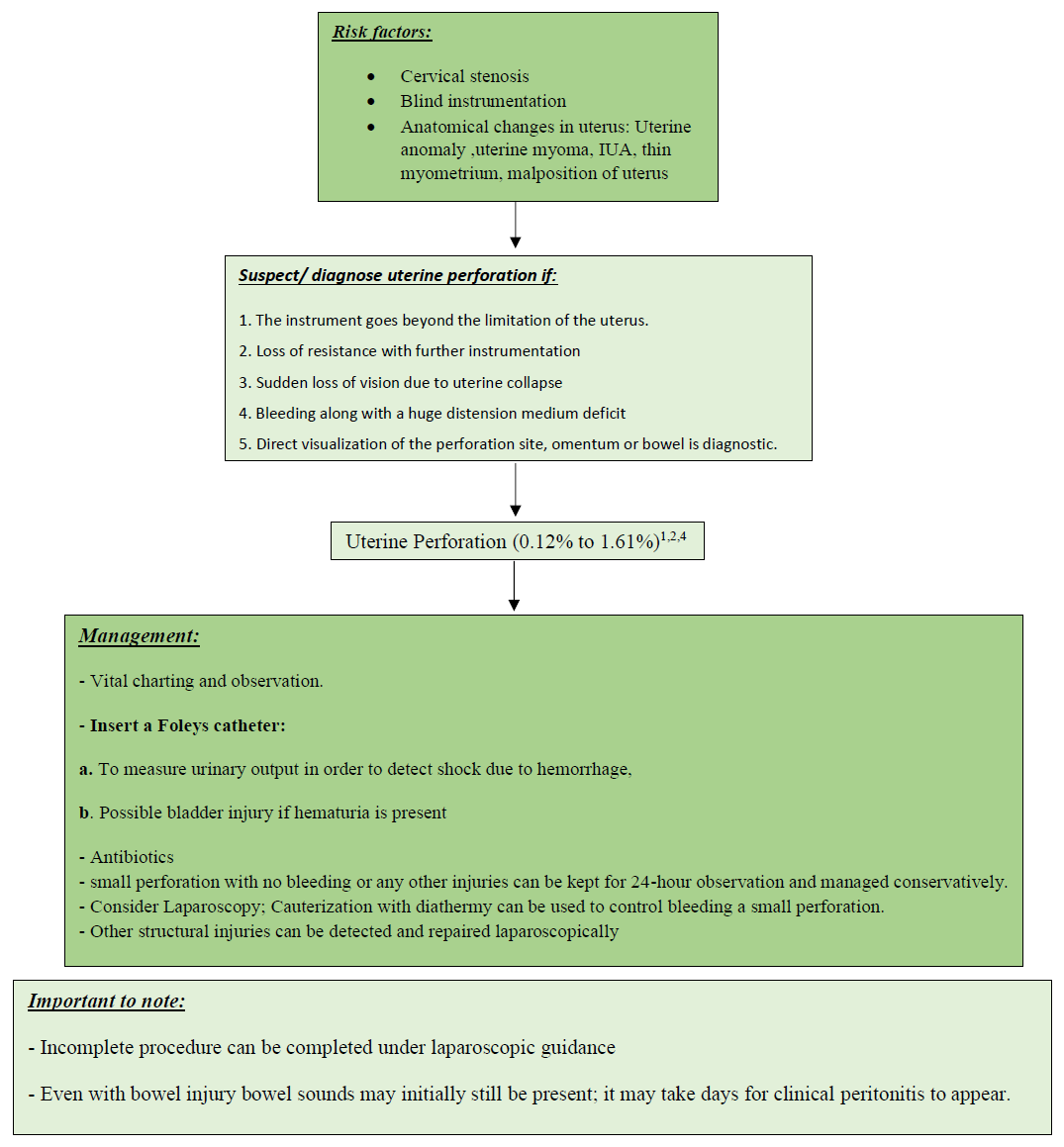
The most common complication associated with both diagnostic and operative hysteroscopy is uterine perforation (1,2). Figure 2 depicts uterine perforation during hysteroscopic procedure and its management on laparoscopy.
The general condition of the patient, cause, location, bleeding and severity of the uterine perforation are the basis of management of uterine perforation. It is important to note that at every step of hysteroscopy like dilatation of cervix, sounding of the uterus, the placement of hysteroscope, or the use of instruments for specimen removal, may lead to defect in the uterine myometrium. In cases where the uterine entry is difficult due to stenosis, nulliparous or menopausal cervix there are chances of formation of false passage during hysteroscopy as depicted in figure 3 but insufficient data is available on false passage creation till date due to underreporting.
In a recent study, the use of misoprostol for pre-procedure ripening of cervix showed decreased incidence of false passage creation but uterine perforation rates were not reduced (3). Immediate surgical intervention is needed in case of perforation by an electrosurgical electrode, heavy bleeding or suspected visceral injury (fig 2). The scheme for diagnosis, management and various risk factors of uterine perforation due to hysteroscopy are listed in figure 4.
Infection
For routine hysteroscopic procedures use of antibiotics as a prophylaxis is not recommended. In women with active pelvic infection or herpes infection hysteroscopy is contraindicated5. The incidence of infections like endometritis and urinary tract infections as a postprocedural complication of hysteroscopy is rare which ranges from 0.01% to 1.42% (1, 6).
In various studies, in both diagnostic and operative hysteroscopy the antibiotic prophylaxis coverage has not found to decrease the incidence of post procedural infection (7,8,9). In a study conducted on 1,952 cases with operative hysteroscopies, the higher risk of endometritis was found after adhesiolysis as compared to myomectomy or polypectomy (10).
Fluid Overload
In some rare cases lethal complications such as neurologic complications, pulmonary edema and even death may occur due to excessive distension media absorption.
There is an increased risk of hypotonic hyponatremia and cerebral edema associated with the use of hypotonic, electrolyte-free distension media. With the proper pre-operative assessment of the intrauterine lesions, vigilant prior planning and use of a hysteromat to measure fluid deficit one can minimize these complications associated with fluid overload.
Fluid deficit is observed mostly with operative as compared to diagnostic hysteroscopy affected by intra uterine pressure kept during procedure, duration of the procedure, number and size of the pathologies removed, the number of myometrial sinuses opened, and the depth of myometrial resection.
It can be prevented by limiting excessive fluid absorption, early and prompt recognition and management of fluid overload, and selecting a distending medium that minimizes risks. Intravasation of fluid can be reduced by injecting Vasopressin in the cervical stroma (11). A close and frequent monitoring of the fluid deficit during the hysteroscopy is the best way to limit excess fluid intravasation. Fluid overload is firstly managed by termination of hysteroscopic procedure; followed by evaluation of hemodynamic, respiratory, cardiovascular and neurologic status; osmolality and serum electrolytes are to be checked; and diuretic administration may be considered. Nowadays fluid monitoring has become easy and precise with the newer fluid management systems like hysteromat; however, these are not readily available in all settings due to their high cost.
Fluid Monitoring guidelines and the measures to limit fluid excess (12)
- Close monitoring of intravenous hydration of patients during both preoperative and intraoperative period.
- Close watch on intra operative hysteroscopic fluid absorption.
- For old aged patients, or having associated comorbidity, having cardiovascular or kidney dysfunction, and in an outpatient setting lower fluid deficit thresholds should be considered.
- The upper limit of fluid deficit in healthy patients is 2,500 mL for isotonic fluids, 1,000 mL for hypotonic fluids, and 500 mL for high-viscosity fluids. But, if fluid deficit reaches 2,000 mL of isotonic fluid, 750 mL of a hypotonic fluid, or 300 mL of a high-viscosity fluid, further infusion should be stopped and finish hysteroscopy. Anesthetist must be involved in such decision and further management, if applicable.
- Fluid deficit threshold is further lowered in an outpatient setting due to limitation of quick care and laboratory facilities.
- Early recognition of fluid deficit in real-time can be best measured by an automated fluid monitoring system.
- A person should be made in charge to evaluate intake and outflow of the fluid frequently and inform the fluid deficit to the surgical team.
- If maximum fluid deficit occurs general condition and systemic assessment apart from signs and symptoms of fluid overload should be done. Thorough evaluation of osmolality and serum electrolytes is done, diuretics given, and other measures taken as indicated. Further treatment of fluid overload or hyponatremia may need corrective fluid infusion, multidisciplinary team management in a critical care setting.
Air and Gas Embolism
The use of carbon dioxide (CO2) as a hysteroscopic distension medium may lead to air embolism as a complication in hysteroscopy, various risk factors include room air entering during cervical instrumentation or dilatation, Trendelenburg position or gaseous byproducts released during electrosurgery especially seen in operative hysteroscopy (13). As CO2 is more soluble in blood as compared to oxygen; so, greater risk of development of air embolism is associated with room air, which is a mixture of oxygen and nitrogen as compared to carbon dioxide (14). Cardiac or pulmonary failure or death are the lethal complications due to air or gas embolism. Dyspnea and chest pain are the usual symptoms associated with air or gas embolism, while if the patient is under anaesthesia then air embolism should be suspected with a decrease in end-tidal carbon dioxide (EtCO2) pressure or hypotension, tachycardia like hemodynamic changes are noted. The reported incidences of clinically significant gas embolism episodes associated with hysteroscopic procedure are very less in the literature (15,16).
Preventive measures for air or gas embolism include evacuation of air from hysteroscopic equipment and in flow tubing; restrict constant cervical insertion of instruments, which can push air in a “piston-like” manner in the uterine cavity and limiting intrauterine pressure. Minimize cervical trauma and if required, osmotic dilators may be considered preoperatively. Always keep the os closed so that room air entry inside uterus is avoided. Try to keep the previous dilator inside till hysteroscope or resectoscope is set up. Primary management of air and gas embolism consists of both conservative and active measures, like quick stoppage of the hysteroscopic procedure and uterine cavity deflation. Durant’s maneuver, can be done to help in migrating air in the direction of right ventricle in order to decrease the obstruction at the right ventricular outflow tract, it can be performed by placing the woman in the Trendelenburg and left lateral decubitus position (14).
Vasovagal Reaction
The procedure should be stopped soon after identification of vasovagal features such as vomiting, diaphoresis, pallor, hypotension, bradycardia, nausea, or loss of consciousness and patient evaluation and conservative measures should be taken. Just by supportive measures like raising the patient’s legs or placement in the Trendelenburg position will correct majority of the cases. Intravenous administration of atropine 0.5 mg every 3 to 5 minutes, up to 3 mg maximum is considered for treating bradycardia if present (17).
Intra-procedural and post-procedural pain may be reduced by ‘vaginoscopic entry technique’. The efficacy of vaginoscopic approach is same as conventional entry technique (18).
Conclusion
Complications associated with diagnostic hysteroscopy are relatively rare and can be averted to a great extent with proper patient selection and pre-procedure evaluation, thorough technique and alertness for impending problems. Gynecologists must be aware about different types of distension media and specific enigma related with each in order to ensure the safety of the hysteroscopy. It should be made a priority for any consultant to understand the physiology and management of air embolism during hysteroscopy. In order to avoid any surgery related litigation clinicians must counsel the patients well regarding various complications and consequences associated with hysteroscopy and obtain a detailed consent before the procedure.
Main Points
- Proper patient selection, appropriate surgical technique and good instruments are to be checked always to prevent such complications.
- A thorough knowledge of various distension medias and associated problems are must for safe surgery.
- Complications from fluid overload may be minimized with careful perioperative planning, use of a fluid management system.
- The gynaecologists should be made aware about the pathophysiology and management of air embolism.
- Small things like positioning also matters in this procedure.
References
Figure 1. Schematic representation of various complications associated with diagnostic hysteroscopy
Figure 2. Iatrogenic uterine perforation due to hysteroscopy and its laparoscopic management
Figure 3. False passage located posteriorly to the internal cervical os.
Figure 4. Scheme for diagnosis and management of uterine perforation