Authors / metadata
DOI:10.36205/trocar1.2023009
Abstract
The Fallopian tubes are the passageway for the oocytes and sperms to meet and form an embryo to make its way to the uterus to implant. Infertility is a common problem of couples with reproductive age. Tubal abnormality is an important cause of infertility, accounting for 25%–35% of female infertility [1].
Tubal patency testing is important during infertility work up, before any assisted reproductive technique is performed. During hysteroscopy tubes are important guidance points as well, but during this procedure any lesion of the uterus or endometrium can be detected, not to mention the possibility for the tubal patency test.
Aim and method Our aim was to investigate the results of women who underwent selective pertubation via office hysteroscopy through a retrospective study. A total of 221 women were included in this retrospective study, who chose this method during their infertility work-up. The selective pertubation with office hysteroscopy was performed in an outpatient setting, without anaesthesia.
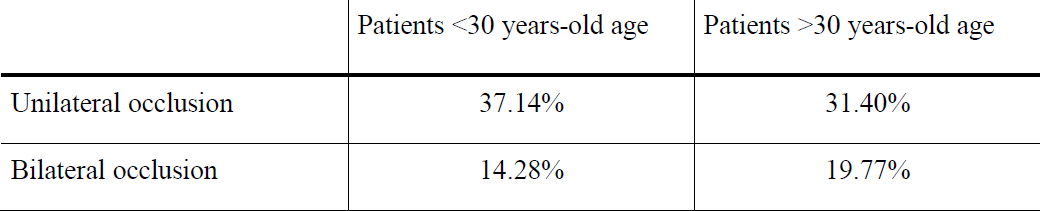
Results: Primary infertility in 158 cases (75.96 %), secondary infertility 43 (20.67 %), repeated abortions 3 (1.44 %) were the indications for office hysteroscopy. Regarding the selective perturbation test, we detected positivity (tubal blockage) in 61,32 % of the women. We divided patients into two groups. Under 30 years-old age unilateral occlusion had significantly higher prevalence (37.14%, p=0.001) compared to the group of patients over 30 years-old (31.40%) and in 19.77% of patients over 30 years-old had bilateral occlusion which is significantly higher than patients under 30 years-old (14.28%, P=0.0001). No complications occurred during the 221 diagnostic office hysteroscopies. During the follow-up questionnaire regarding all pregnancies 30 (88%) of patients had successful conception within one year. 46 women (92%) would suggest this method to other women.
Conclusion: Our results suggest this novel method, selective pertubation with office hysteroscopy, which is an effective, accurate, minimally invasive method to investigate tubal patency, in outpatient circumstances to choose proper assisted reproductive techniques. This way the complications of general anesthesia or radiation (HSG) can be avoided. Due to the tubal flushing effect, this method can be therapeutic, as well. Moreover, with the examination of the uterine cavity, other uterine factors can be detected and treated so fertility can be improved as well.
Introduction
Anatomic position, origin and function
The Fallopian tubes are important structures of the female genital tract, emerge from the posterior and superior part of the uterine corpus, supported by the broad ligaments. During the embryologic development Fallopian tubes, as well as the uterus, cervix, and upper third of the vagina, develop from the Müllerian ducts which originate from the mesonephric kidneys and mesonephros [2].
The lumen of the Fallopian tubes communicates with the uterine and the intraabdominal cavity. Each tube is divided into four parts named from the uterus: a broad interstitial section, with a narrowed lumen the isthmic part, again with a larger lumen the ampulla and the fimbria which is located at the end of the tubes with a spacious area.
The Fallopian tubes are the passageway for the oocytes and sperms to meet and form an embryo to make its way back to the site of implantation in uterus [3].
Fallopian Tubes during hysteroscopy
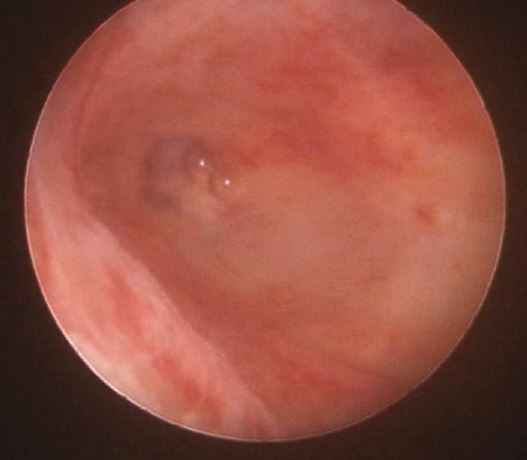
During hysteroscopic evaluation of the uterus the most important guidance points right after entering through the endocervical canal are the entrance of the Fallopian tubes both sides (Figure 1.). Having a panoramic view of the uterine cavity, tubal Ostia should be present at 2 and 10 o’clock location. The lack of the visualization of tubal ostium should warn the surgeon of false passage during the entrance, or severe intrauterine adhesions [4].
Fallopian tubes and infertility
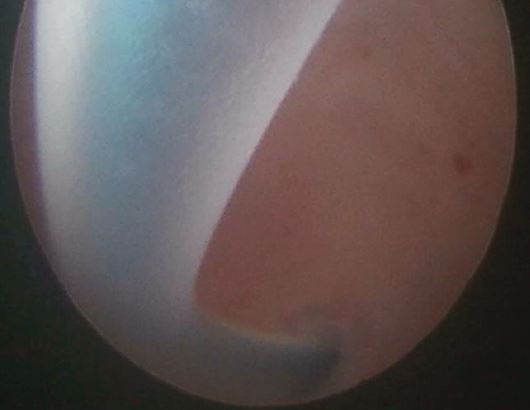
Worldwide one of the leading methods, during the infertility workup should be the hysteroscopy to exclude the organic pathology of uterus and Fallopian tube in women. As tubal occlusion is one of the main causes of female infertility, evaluation of tubal patency is one basic point during the early phase of these infertility examinations. The relevance of diagnostic hysteroscopy, especially when performed in an outpatient “office” setting, in the evaluation process of infertility has increased in the last years yet, not backed by evidence so far unfortunately. During hysteroscopy the uterine cavity and the entrance of the Fallopian tubes can be evaluated while dilated with distension media. Occlusion and therefore infertility can occur, if any endometrial or myometrial lesions, e.g., polyps and fibroids, block the entrance ofthe tubes (Figure 2.). With the help of operative tools such as resectoscope, scissors or HTRS, these lesions can be easily treated.
While using fluid distension air can be injected into the uterine cavity and the movement of air bubbles can be followed through the hysteroscopic monitor. As an indirect sign, the escape of the air bubbles towards the ostia of the Fallopian tubes from the uterine cavity can be rated as a sign of tubal patency. Several studies have examined this phenomenon and assessed the accuracy of the bubble sign. Unfortunately, this sign means proximal patency of the tubes. In case of distal blockage there will be passage of air bubbles through the ostia. In case of hydrosalpinx or peri tubal adhesions the risk for a false-negative results are increased [5, 6, 7].
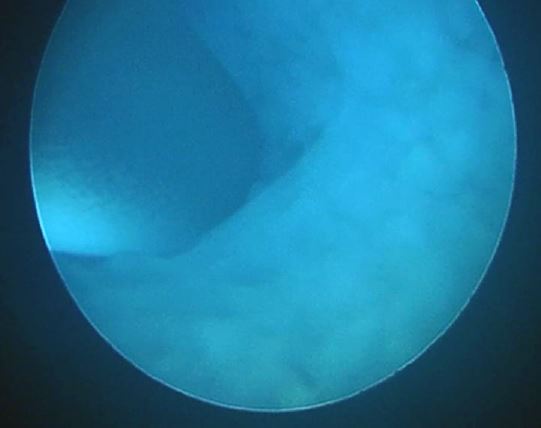
The gold standard for tubal patency test is the laparoscopic chromo-hydrotubation of the Fallopian tubes but still there are many disadvantages e.g., invasiveness, need of operating room, anaesthesia, missing from work, compared to the other hysteroscopic solution which is the office hysteroscopy-guided selective chromopertubation test. This method regarding the overall costs is less expensive, no need for anaesthesia, can be performed in an outpatient setting. A 2.7-mm optic is used for the evaluation with a 5.5-mm sheath (EMD Kft, Debrecen, Hungary). Vaginoscopic approach is used for the entrance to the cervical canal. As a distension media normal saline solution is used. The tip of a flexible, transparent plastic catheter is placed through the working-channel to each entrance of the Fallopian tubes. Through the catheter methylene blue dye is injected. If the catheter stained blue and no back-flow can be detected, view of the endometrium and uterine cavity remains clear, patent tube is diagnosed (Figure 3.). If the Fallopian tube is occluded, the uterine cavity becomes blue because of back-flow of the dye (Figure 4.). We can give lot confidence and credit for this method as specificity and sensitivity were estimated 82.1%, 83.3%. The accuracy of the test can be increased if the hysteroscopic evaluation is followed by a transvaginal ultrasound examination. So, the overall accuracy of this method is 82.9% with the laparoscopic method taken as reference [8, 9]. This diagnostic test, as others for patency test, can be therapeutic, as well. Due to the tubal flushing effect, endometrial detriments, sludges can be washed out of the tube, causing patency [10,11].
Material Method
Our aim was to investigate the results of women who underwent selective pertubation with office hysteroscopy. In each case before and after the procedure 3D ultrasound was performed. A total of 221 women were included in this retrospective study, after signed informed consent and accepted ethical approval, who chose this method during their infertility work-up between 2016.11.01.-2022.12.29.
For infertility we used the most common definition: no conception in more than 1 year (6 months above age 35), unprotected intercourses. As a follow-up, a questionnaire was submitted from 53 women after the procedure through phone call to evaluate post-procedure pregnancy and delivery.
Results
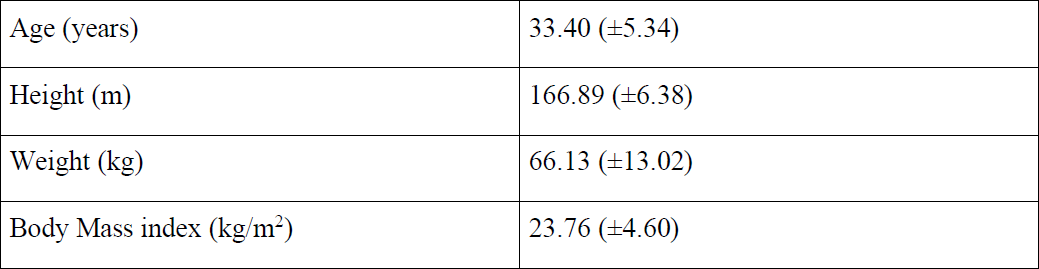
Primary infertility 158 (in 75.96 %), secondary infertility 43 (in 20.67 %), repeated abortions 3 (in 1.44 %) were the indication for office hysteroscopy. Besides the infertility in 5 (2.40 %) cases, previous positive ultrasound result was the indication of hysteroscopy as well. The mean age of the patients was 33.4 ± 5.34 years, body mass index was 23.76± 4.60 (table 1). During the evaluation of uterine cavity 13 cases required polypectomy as well, 2 patients needed uterine myomectomy, in 3 cases septotomy was performed. Endometrial visualization and strawberry like endometrial surface of 43 cases indicated biopsy as well during the evaluation with office hysteroscopy, this way 15 chronic endometritis were detected.
Regarding the selective perturbation test, we detected positivity (tubal blockage) in 61,32 % of the women, among them we explored unilateral occlusion 43,08 % of the cases and bilateral occlusion cases in 56,92 % of the patients. We divided patients into two groups. Under 30 years-old age unilateral occlusion had significantly higher prevalence (37.14%, p=0.001) compared to the group of patients over 30 years-old (31.40%). Regarding the bilateral occlusion, tests showed opposite results. In 19.77% of patients over 30 years-old had bilateral occlusion which is significantly higher than patients under 30 years-old (14.28%, P=0.0001) (table 2).
No complications occurred during the 221 diagnostic office hysteroscopy. During the follow-up questionnaire from 53 women 34 (68%) had at least one live birth since the procedure, out of them 5 (14%) women conceived spontaneously, 13 (38%) women had intrauterine insemination, and 16 women had successful ART. Regarding all pregnancies 30 (88%) of patients had successful conception within one year. 46 women (92%) would suggest this method to other women.
Discussion
Tubal factor contributes 30% of all female infertility, usually originate secondary due to tubal occlusion as a consequence of pelvic inflammatory diseases caused by several pathogens. Finding an accurate, cheap, easily available, painless method for diagnosis of tubal occlusion is crucial regarding the infertility work-up. Our results suggest office hysteroscopy, especially office hysteroscopy-guided selective chromopertubation method for evaluation tubal patency because this is an effective, reproducible, accurate, minimally invasive method to investigate tubal patency, with less or no pain in outpatient circumstances in order to choose appropriate assisted reproductive techniques to conceive. This way the complications of general anaesthesia or radiation (hysterosalpingography) can be avoided. With the accuracy of 82.9% compared to the gold-standard laparoscopic chromo-hydrotubation this method can be accepted as a first-line, out-patient test.
In our study we found bilateral blockage of the tubes significantly frequent (19.77%) in older (over 30 years old) subgroup compared to the younger (less than 30 years old) subgroup (14.28%). The diagnostic tubal patency test at the same time can be therapeutic, as well, caused by the tubal-flushing effect. Due to the feed-back of the patients, this method is acceptable and 92% of them is recommended to others. Moreover with the examination of the uterine cavity, visualization of the tubal Ostia, other factors, such as polyps, fibroids at the entrance von the tubes, or micropolyps, chronic endometritis can be detected and treated so fertility can be improve as well [12].
Conclusion
Our results suggest this novel method, selective pertubation with office hysteroscopy, which is an effective, accurate, minimally invasive method to investigate tubal patency, in outpatient circumstances to choose proper assisted reproductive techniques. This way the complications of general anesthesia or radiation (HSG) can be avoided. Due to the tubal flushing effect, this method can be therapeutic, as well. Beyond the tubal patency with this method intrauterine pathologies, other causes of infertility could be ruled out or treated as well.
References
Figure 1. Right tubal ostium with some air-bubbles. Image by P. Török
Figure 2. Left tubal ostium with a small polyp at the entrance. Image by P. Török
Figure 3. Transparent catheter in the tubal ostium. Due to patency, blue dye can be seen in the catheter, but cannot be seen in the uterine cavity. Image by P. Török.
Figure 4. Transparent catheter in the tubal ostium. Due to blockage, blue dye back-flows and can be seen in the uterine cavity. Image by P. Török
Table 1. Data of women who underwent office hysteroscopy selective pertubation.
Table 2. Results of office hysteroscopy selective perturbation tests regarding age-divided subgroups.