Metadata
Posters
PSTR Diagnostic Laparoscopy in Herlyn-Werner-Wunderlich (HWW) syndrome: A case series
- Akbar Novan Dwi Saputra1, Nuring Pangastuti1, Rika Erlinawati1
1 Department of Obstetrics and Gynaecology, Faculty of Medicine, Public Health and Nursing, Gadjah Mada University, Sardjito Hospital, Yogyakarta, Indonesia.
Email: Akbarnovan1986@ugm.ac.id Phone number: +62821 20989802 Introduction: The Herlyn-Werner-Wunderlich (HWW) syndrome is a rare congenital anomaly involving Müllerian (paramesonephric) and mesonephric ducts characterized by the triad of uterus didelphys, unilateral obstructed hemi-vagina and ipsilateral renal agenesis, also known as OHVIRA. Clinical suspicion and early diagnosis are crucial in providing a timely treatment to prevent complications. Diagnostic laparoscopy is indicated when radiological imaging is inconclusive and for treatment of concomitant conditions or complications.
Objective: To report four different cases of Herlyn-Werner-Wunderlich (HWW) syndrome in which laparoscopy was performed due to suspected presence of complications.
Methods: A retrospective case series of HWW syndrome at our hospital during 2019-2021. Data were obtained from medical records, including general patient information, history of disease, surgical procedures, and outcomes. Surgical procedures consisted of laparoscopy and vaginal septum resection (septectomy).
Results: We report four cases of HWW syndrome in which diagnostic laparoscopy is performed due to suspected presence of complications. Laparoscopy was able to detect complications in all the four cases, including hematocolpos, adhesions, endometriosis, and hematosalpinx, some of which were not detected by imaging. These complications were managed during laparoscopy, namely drainage of hematocolpos, adhesiolysis, removal of endometriosis, and salpingostomy. On follow-up visits, patients reported regular menstruation without any pain and no complications.
Conclusion: Prompt and accurate diagnosis is important to provide early treatment, prevent complications of HWW syndrome, and preserve future fertility. Despite being considered as the most accurate imaging method, MRI has also been demonstrated to have significant discrepancies with diagnostic laparoscopy in complicated cases of HWW syndrome. In such cases, laparoscopy can be both diagnostic and therapeutic. Laparoscopy is able to clarify the pelvic anatomy, detect presence of complications, and become a therapeutic approach for complications. Laparoscopy should be considered the gold standard for complete evaluation of HWW syndrome and be reserved for cases of HWW syndrome with suspected presence of complications.
PSTR Struma Ovarii: A case report of a rare ovarian mass
- Woo jeng Kim
Department of Obstetrics and Gynecology, Incheon St. Mary’s Hospitals, College of Medicine; The Catholic University of Korea, Seoul, Korea.
Email: yoteam0811@nover.com Tel + 82-10-9171-1392 - Struma ovarii is a rare type of ovarian mass that has a predominance of thyroid tissue. In most cases, it is benign and accounts for about 2.7% of teratoma. Most patients are asymptomatic and, it is rarely diagnosed before surgery and is often diagnosed histologically after surgery. We would like to report a case related to struma ovarii. A 16-years-old patient was referred for abdominal distension and intermittent abdominal pain. Computed Tomography (CT) scan showed a 21 x 14 cm sized huge multi-chambers cystic mass arising from a left ovary with different attenuation at each chamber. The serum tumour marker CA-125 was considerably increased. A laparoscopic Left ovary cystectomy was performed. The mass contains mucinous fluid. Patient had an uncomplicated postoperative course. Prior to the surgery the mass was speculated to be a mucinous cystadenoma. However, histopathology showed thyroid tissue, confirming the diagnosis of Struma ovarii. All components of the solid portion consisted of thyroid tissue, and some thyroid follicles were identified between the fibrotic tissues in the cystic wall. Postoperative thyroid function test was normal. Looking at previous studies, it is reported that struma ovarii has a higher rate of benign cases and that fertility conserving management can be implemented. Clinical hyperthyroidism is associated in 5-8%, and malignant cases are associated with papillary and follicular thyroid cancer. Additionally, there was a case in which struma ovarii was later found in a patient with thyrotoxicosis. In the present case, the TFT was in the normal range. In conclusion, although it is a rare form, diagnosis of struma ovarii should be considered when evaluating and treating the ovarian masses.
PSTR Fallopian Tube Recanalization (FTR) Outcome in Bilateral Non-Patent Tubes at Dr. Moewardi Hospital Surakarta: Case Series
- Iham Ramadhanis, Abdurahman Laqif, Agung Sari Wijayanti, Eriana Melinaw
Department of Obstetrics and Gynecology, Faculty of Medicine, Sebelas Maret University, Dr. Moewardi Hospital Surakarta, Indonesia
Correspondence: ilhamramadhanis@live.com / 081215778947 Introduction: Tubal obstruction is one of the common causes of female infertility and almost always in need of artificial reproductive technology. Anatomical improvement of the tubes using surgical procedures are expected to restore their function. However, it increases the risks, cost, and morbidity. Previous studies show good technical success rates for fallopian tube recanalization (FTR) using minimally invasive transcervical tubal catheterization.
Objective: To report the outcome of three cases of infertility due to bilateral non-patent tubes after performing FTR.
Method: We retrospectively evaluated three cases of FTR procedures performed from July to November 2022 at Dr. Moewardi Hospital. The three cases had undergone a basic infertility evaluation with the final diagnosis: infertility due to bilateral non-patent tubes. Infertility due to anovulatory and male factor were excluded. Minimally invasive transcervical tubal catheterization-hysterosalpingography with high pressure contrast injection followed by fluoroscopy were performed. The success of the technique was confirmed if both tubes were patent at the end of the procedure. Clinical pregnancy was confirmed if a gestational sac was seen at transvaginal sonographic examination within 12 weeks post-procedure.
Result: Case-1 with five years primary infertility: the technique was successful but patient did not get pregnant. Case-2 with one-year primary infertility: the technique was successful and a spontaneous pregnancy did occur eight weeks after the procedure. Case-3 with a five years secondary infertility: the technique was successful, but patient did not get pregnant.
Conclusion: There were three technical successes in the three cases that underwent FTR, one of which became pregnant.
PSTR Successful Pregnancy after RFA treatment in Cases of Intramural Myoma Type 3 in IVF Program
- Doddy Susanto
Department of Obstetrics Gynecology, Prof. Dr. Soerojo Mental Hospital Magelang, Indonesia Introduction: Uterine myomas are non-cancerous tumors that most often appear during the reproductive years. Myomas have a high prevalence and may be a cause of infertility. The study about the effect of myomas being constrained within the wall of the uterus known as intramural fibroids on implantation is still limited. Intramural fibroids that distort the endometrial cavity are associated with reduced implantation rate following IVF treatment. There are no medical procedures for myoma removal, except myomectomy, which is widely acknowledged to be suitable for long-term fertility. Ultrasound-guided uterine myoma ablation therapy has been proven to be effective, less invasive than other modalities, and has minimal adverse effects, therefore it may be the best procedure approach. There have been no previous reports of pregnancy after laparoscopic, transcervical, or transvaginal radiofrequency ablation of fibroids in Indonesia.
Case report: We present the outcomes of the first viable pregnancy after a transvaginal ultrasonography-guided radiofrequency ablation of intramural myomas in an IVF program. A 33-year-old gravida 1, para 0 female requested treatment for dysmenorrhea of uterine fibroids and had future pregnancy wish. She had a history of being married for four years and had uterine cysts. Transvaginal ultrasonography revealed an anteromedial type 3 myoma measuring 3,1x 3,2 x 3,0 cm with a volume of 17,30 cm3. The patient had previously undergone a laparoscopic cystectomy and salpingectomy.
PSTR Successful Management of Extrauterine IUD Translocation
- Adhitya Yudha Maulana1, Malvin Emeraldi2
1 Obstetrics and Gynecology Resident in Faculty of Medicine, University of Indonesia
2 Reproductive Endocrinology Fertility – Obstetrics and Gynecology Department, Fatmawati National Hospital Background: Intrauterine devices are the most commonly used long term contraception in Indonesia. This is due to their 98-99% effectiveness in preventing pregnancy. However, frequent use of IUD’s is associated with complications such as IUD translocation. The prevalence of IUD translocation is 1,3/1000 these mainly occur during insertion. Extrauterine IUD translocation may further cause chronic pelvic pain, perforation of bladder or intestines, intestinal obstruction, abscess, adhesions, fistula formation, and undesired pregnancy. Therefore, removal of extrauterine IUD translocation is recommended.
Objective: The aim of this study is to describe the effective management of extrauterine IUD translocation.
Methods: We report a case of patient who underwent laparoscopic removal of an extrauterine IUD on January 30th 2022 in the Obstetrics and Gynecology Department of the Fatmawati National Hospital Jakarta.
Results: A 22-year-old G1P1 woman complained of chronic pelvic pain (VAS 4) for two weeks before admission. The patient had a history of spontaneous labor two month earlier and then had an IUD insertion in the puerperal period. On transvaginal US examination, the IUD was not visible in the uterine cavity but in the pelvic cavity a hyperechoic elongated structure was seen suspicious of an extrauterine IUD location. Diagnostic hysteroscopy was performed followed by laparoscopy. On hysteroscopic view there were no IUD or IUD threads visible in the uterine cavity. Laparoscopy showed that the IUD string was attached to the omentum and the IUD rods imbedded in the anterior peritoneum. The uterus and both adnexa were normal. Adhesiolysis was performed between the omentum and the anterior peritoneal wall until the IUD could be completely removed. The IUD and omentum then were removed from abdominal cavity. One day postoperatively, the patient was in good condition and was discharged.
Conclusion : Extrauterine IUD translocation is rare complication of the IUD insertion. Laparoscopic removal is the procedure of choice which has proven to be highly successful in the removal of IUD translocations.
PSTR Scoping Review of High-Intensity Focused Ultrasound (HIFU) Procedure in Adenomyosis
- Indra Adi Susianto 1, Relly Yanuari Primariawan 2, Riyan Hari Kurniawan 3, Christina Meilani Susanto 2, Rima Yulia Effriyanti 4, Aries Joe 5
1. Medical Faculty of Soegijapranata Catholic University
2. Medical Faculty of Airlangga University, Surabaya
3. Medical Faculty of Universitas Indonesia, Jakarta
4. Morula IVF Melinda, Bandung
5. Bunda, General Hospital, Jakarta, Indonesia Introduction: Adenomyosis is a gynecological disease characterized by ectopic endometrial tissue in the myometrium which often occurs in women of reproductive age, between 30-40 years. The prevalence of adenomyosis currently ranges from 20-35%. The patient’s main clinical symptoms include abnormal uterine bleeding, menstrual pain (dysmenorrhea), and impaired fertility (infertility). The pathological mechanism for the occurrence of adenomyosis is an imbalance of steroid hormones, a local inflammatory process that causes changes in cell proliferation which may lead to neuro angiogenesis in myometrial tissue (1,4). Current therapy for adenomyosis includes oral medications, progesterone, contraceptive pills or anti-inflammatory pills as well as GnRH Agonist injections and adenomyomectomy that can be performed by conducting minimally invasive laparoscopic surgery/laparotomy surgery (5). Surgical removal of the uterus (hysterectomy) is the main option for women who no longer want children, but hysterectomy for adenomyosis that occurs in infertile couples is not a good choice for women who still want children. Although UEA treatment can improve patient symptoms, its effect on ovarian function and pregnancy is still uncertain (4,5).
High Intensity Focused Ultrasound (HIFU), an emerging non-invasive surgical technique for the treatment of benign tumors, has been used for adenomyosis since 2008. Under ultrasound or magnetic resonance (MRI) examination, HIFU high intensity ultrasound energy can penetrate the abnormal target tissue and remove the lesion through thermal effects and cavitation and allows the preservation of normal tissue around the lesion. The cavitation process is a condition in which HIFU will create static pressure on the targeted cells so that the liquid in the cells decreases until it is under the pressure of liquid vapor, which results in the formation of bubbles filled with small vapor bubbles in the liquid. The bubble eventually explodes and the liberated gas passes into the surrounding liquid through a mechanism that initially softens and then gets absorbed by healthy body tissue.
In recent years, HIFU therapy has become a viable surgical alternative for patients who still wish to retain their uterus. However, adenomyosis is a disease that is very sensitive to the estrogen hormone, and HIFU therapy will not change the working of hormones in the body. The risk of recurrence therefore still exists. Gonadotrophin Releasing Hormone Agonist (GnRH-A) is a hormone that is commonly used for the treatment of adenomyosis, it lowers estrogen levels to menopausal levels and increase adenomyotic apoptosis in the myometrium.
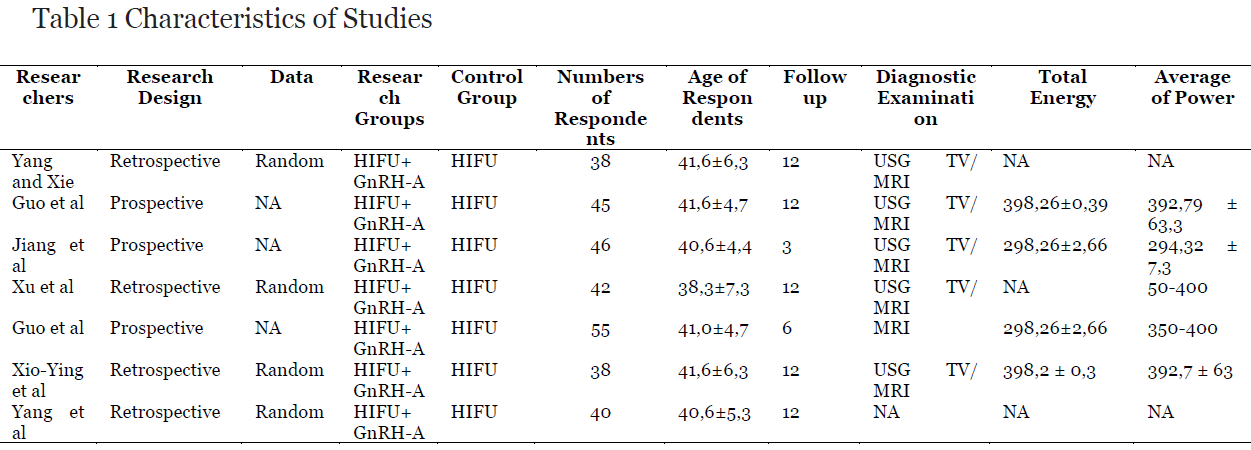
This chapter provides several systematic reviews and meta-analyses of HIFU combined with GnRH- A in adenomyosis and provides proof-based medical evidence for clinical applications.Material and methods: Vannuccini and Petraglia’s study that is included in this meta-analysis met the following criteria. It compares HIFU combined with GnRH-a versus. HIFU solely in patients with adenomyosis. The HIFU group combined with GnRH-a is defined as the experimental group, the HIFU group itself is defined as the control group. Strubel et al. The objects of the study: (1) women aged 18–50 years; women with focal or diffuse adenomyosis diagnosed by ultrasound, MRI, or computed tomography (CT); patients who have not received any treatment for adenomyosis within 3 months prior to the study. Abbott Outcome indicators: The main outcome indicators are changes in uterine volume while adenomyotic lesions are defined as the main outcome. The secondary outcomes are the visual analog scale (VAS) score for dysmenorrhea, menstrual volume score, serum CA125 level, and recurrence rate. The exclusion criteria for the inclusion of studies in this report are the following: animal experiments, case reports, conference abstracts, conference proceedings, editorial letters, guidelines or comments; repeated study; studies in which the full text is not available; patients with uterine fibroids or other gynecological diseases, whose clinical symptoms are similar to adenomyosis and study less than 3 months HIFU after ablation.
Results: Of the 390 articles, 9 studies were retained with data of 766 patients analyzed in this meta-analysis (11-19). Of the nine studies, one of them was using MRI for the imaging diagnosis of adenomyosis, six were using transvaginal ultrasound or MRI, and the other two did not report specific imaging diagnostic methods. Although these studies provide information about the diagnostic imaging methods used, they do not provide specific imaging criteria for the diagnosis of the adenomyosis.
Changes in the physiology of adenomyosis
- Changes in uterine volume: Among the nine studies included, only three reported a method of generating random-location sequences, which was the random number table method. The analysis demonstrated the change of Uterine Volume as the rate of uterine volume reduction after HIFU in 232 patients. The results of the meta-analysis showed that the rate of uterine volume reduction in the HIFU group with GnRH- a was higher than that in the HIFU only group at 12 months after the procedure 13,20).
- Changes in volume of adenomyotic lesions: Three studies (239 cases) reported changes in lesion size before and after HIFU ablation which showed that the volume of the lesions in the experimental group was smaller than that in the control group in 3 and 6 months after the procedure. Although the results of the study showed no significant difference in both groups (p > 0.05) (11,12,17).
- VAS Score for Dysmenorrhea: A total of five studies (367 cases) used VAS to assess patient with dysmenorrhea. The results of the meta-analysis showed that the VAS score for dysmenorrhea in the HIFU group with GnRH-a was lower than the HIFU group alone after the procedure (11,13,14,17,18).
- Menstrual Volume Score: Three studies (243 cases) used the menstrual volume score to assess menstrual bleeding. The results of the meta-analysis showed that the menstrual volume score of the HIFU group with GnRH-a was lower than that of the HIFU group itself after the procedure (14,16,19).
- Levels of Serum CA125: Three studies (252 cases) evaluated patients’ levels of serum CA125. The results of the meta-analysis showed that serum CA125 levels in the HIFU group with GnRH-a were lower than the HIFU group alone after the procedure (11,17,18).
- Recurrence Rate: Three studies (314 cases) compared the recurrence rates in the experimental and control groups. The results of the meta-analysis showed that the relapse rate in the HIFU group with GnRH-a was lower than that in the HIFU group itself (15,16,19).
- Pregnancy Outcome: One study reported patient pregnancy outcomes at 6 months after treatment. There were five pregnancies reported after the HIFU intervention combined with GnRH-a (n = 45), three of which delivered naturally and two ended in abortion. In the HIFU only group (n = 46), there were four reported pregnancies following HIFU ablation, one resulting in natural delivery, one resulting in miscarriage and two ending in abortion.
Discussion: The results of the data of this meta-analysis from 766 patients showed that, HIFU combined with GnRH-a compared to the HIFU only group, for the treatment of adenomyosis had greater effectiveness in reducing uterine volume and adenomyotic lesions and alleviating symptoms.
Adenomyosis is a common and difficult gynecological disease that seriously affects women’s health and quality of life. Effective symptom relief, relapse prevention, and increased pregnancy rates are problems that must be solved. Compared to currently available therapies, HIFU is a non-invasive and innovative technology for adenomyosis while still at risk of recurrence. The working mechanism of HIFU resides in producing thermal and cavitation effects that are altered by the mechanical effects of ultrasound causing the target tissue temperature at of the focal point to rise above 60–100◦C, causing non-coagulation thermal necrosis lesions. At the same time, the surrounding structures are not damaged. Previous studies found that uterine smooth muscle tissue in adenomyotic lesions was sensitive to HIFU. HIFU treatment was an effective and ideal treatment for adenomyosis. A retrospective study by Lee et al. enrolled 889 patients with adenomyosis who underwent ultrasound-guided HIFU (USgHIFU). The results revealed that the uterine volume reduction rate was 60.1% at 3, 6, and 12 months after the procedure, respectively. This was consistent with the results of a recent systematic and meta-analysis showing a substantial effect in reducing uterine volume after HIFU treatment for adenomyosis in 12 months (20).
GnRH-a therapy can effectively relieve pain in adenomyosis patients by reducing regulation of GnRH receptors in the body, thereby reducing the level of gonadotropins secreted by the pituitary gland which results in decreased ovarian function. HIFU combined with GnRH-a can help maintaining the effect of HIFU therapy and reduce relapse rates. Most of the studies involved, suggest that patients should be given GnRH-a three times after HIFU ablation. The first GnRH-a is given on the first to third day of the first menstruation after HIFU therapy. Then, the interval between the two GnRH-a injections is within 28 days. The results of the existing study show that the symptoms of both groups are all improved after the procedure, but the VAS or dysmenorrhea scores and menstrual volume scores in the HIFU group combined with GnRH- a are lower than in the HIFU only group. The levels of serum CA125 are also decreased. Although the results of the VAS score for dysmenorrhea show that HIFU combined with GnRH-a can better alleviate dysmenorrhea in each patient, there wis still excessive heterogeneity.
The relationship between adenomyosis and infertility is not clear, but adenomyosis can affect a woman’s fertility, this is mainly related to disruption and thickening of the myometrial junctional zone (JZ), and hypo- acceptability of the endometrium. In recent years, due to the continuous improvement of various ultrasound diagnostic methods and the increasing age of women seeking infertility treatment, the rate of women with a diagnosis of adenomyosis among infertile women has increased. Traditionally, infertile patients with adenomyosis are treated with GnRH-a or they may have adenomyosis (adenomyomectomy) removed surgically. Studies have shown that HIFU is a safe and effective procedure for infertile women and it does not increase obstetric risk (21).
- Conclusion: The results of this meta-analysis show that compared with HIFU only treatment the HIFU accompanied by GnRH-a therapy used on adenomyosis, obtained a greater level of effectiveness in reducing uterine volume and adenomyotic lesions and alleviating symptoms. However, because the number of studies included is too small, further research that has a long-term evaluation is needed.
References
- Vannuccini S, Petraglia F. Recent advances in understanding and managing adenomyosis. F1000Research. (2019) 8:1– 10. doi: 10.12688/f1000research.17242.1
- Struble J, Reid S, Bedaiwy MA. Adenomyosis: a clinical review of a challenging gynecologic condition. J Minim Invasive Gynecol. (2016) 23:164–85. doi: 10.1016/j.jmig.2015. 09.018
- Abbott JA. Adenomyosis and abnormal uterine bleeding (AUB-A)- pathogenesis, diagnosis, and management. Best Pract Res Clin Obstet Gynaecol. (2017) 40:68–81. doi: 10.1016/j.bpobgyn.2016.09.006
- Vannuccini S, Tosti C, Carmona F, Huang SJ, Chapron C, Guo SW, et al. Pathogenesis of adenomyosis: an update on molecular mechanisms. Reprod Biomed Online. (2017) 35:592–601. doi: 10.1016/j.rbmo.2017. 06.016
- Dessouky R, Gamil SA, Nada MG, Mousa R, Libda Y. Management of uterine adenomyosis: current trends and uterine artery embolization as a potential alternative to hysterectomy. Insights Imaging. (2019) 10:48. doi: 10.1186/s13244-019-0732-8
- Yang Z, Cao YD, Hu LN, Wang ZB. Feasibility of laparoscopic high- intensity focused ultrasound treatment for patients with uterine localized adenomyosis. Fertil Steril. (2009) 91:2338–43. doi: 10.1016/j.fertnstert.2008. 03.017
- Cheung VY. Current status of high-intensity focused ultrasound for the management of uterine adenomyosis. Ultrasonography. (2017) 36:95– 102. doi: 10.14366/usg.16040
- Vannuccini S, Luisi S, Tosti C, Sorbi F, Petraglia F. Role of medical therapy in the management of uterine adenomyosis. Fertil Steril. (2018) 109:398– 405. doi: 10.1016/j.fertnstert.2018.01.013
- Khan KN, Kitajima M, Hiraki K, Fujishita A, Nakashima M, Ishimaru T, et al. Cell proliferation effect of GnRH agonist on pathological lesions of women with endometriosis, adenomyosis and uterine myoma. Hum Reprod. (2010) 25:2878–90. doi: 10.1093/humrep/deq240
- Cumpston M, Li T, Page MJ, Chandler J, Welch VA, Higgins JP, et al. Updated guidance for trusted systematic reviews: a new edition of the Cochrane Handbook for Systematic Reviews of Interventions. Cochrane Database Syst Rev. (2019) 10: ED000142. doi: 10.1002/14651858.ED000142
- Guo Y, Duan H, Cheng J, Zhang Y. Gonadotrophin-releasing hormone agonist combined with high- intensity focused ultrasound ablation for adenomyosis: a clinical study. BJOG. (2017) 124(Suppl. 3):7– doi: 10.1111/1471-0528.14736
- Yang F, Xie CZ. Effect of high intensity focused ultrasound combined with GnRHa on adenomyosis and its effect on hemoglobin level. Chin J Fam Plann Gynekol. (2017) 9:64–8.
- Xiao-Ying Z, Ying-Shu G, Jiu-Mei C, Jin-Juan W, Hong Y, Chun-Yi Z, et al. Effect of pre-treatment with gonadotropin-releasing hormone analogue GnRH-α on high-intensity focused ultrasound ablation for diffuse adenomyosis: a preliminary study. Int J Hyperthermia. (2018) 34:1289– 97. doi: 10.1080/02656736.2018.1440014
- Guo Q, Xu F, Ding Z, Li P, Wang X, Gao B. High intensity focused ultrasound treatment of adenomyosis: a comparative study. Int J Hyperthermia. (2018) 35:505–9. doi: 10.1080/02656736.2018.1509238
- Li JM, Zhang Y, Xie SL. Clinical efficacy analysis of HIFU combined with GnRH-a in the treatment of adenomyosis. Med Diet Health. (2019) 17:1– 2. Available online at: http://lib.cdutcm.edu.cn:7001/rwt/CNKI/http/ NNYHGLUDN3WXTLUPMW4A/kcms/detail/detail.aspx?FileName= YXSL201918001&DbName=CJFQ2019
- Jiang J, Zhou HG, Chen Y, Zhang M, Wu H. Prospective study of high intensity focused ultrasound combined with gonadotropin releasing hormone agonist in treating adenomyosis. Chongqing Med. (2019) 48:1705–8. doi: 10.3969/j.issn.1671-8348.2019.10.020
- Tan YT, Li ZA. Observation on the curative effect of non-invasive high- intensity focused ultrasound therapy combined with gonadotropin releasing hormone agonist in treatment of adenomyosis. Maternal Child Health Care China. (2019) 34:4811–5.
- Xu F, Tan LX, Li P, Quo Q. Clinical study of high-intensity focused ultrasound ablation combined with GnRHa in the treatment of adenomyosis. J Int Obstetrics Gynecol. (2019) 46:618–40. Yang LJ, Liu J, Su YY. Clinical study of HIFU alone and GnRH-a combined treatment for adenomyosis. Shenzhen J Integrated Traditional Chin Western Med. (2019) 29:96–8. doi: 10.16458/j.cnki.1007-0893.2019.10.043
- Gong C, Setzen R, Liu Z, Liu Y, Xie B, Aili A, et al. High intensity focused ultrasound treatment of adenomyosis: the relationship between the features of magnetic resonance imaging on T2 weighted images and the therapeutic efficacy. Eur J Radiol. (2017) 89:117–22. doi: 10.1016/j.ejrad.2017. 02.001
- Zhang L, Zhang W, Orsi F, Chen W, Wang Z. Ultrasound-guided high intensity focused ultrasound for the treatment of gynaecological diseases: a review of safety and efficacy. Int J Hyperthermia. (2015) 31:280– 4. doi: 10.3109/02656736.2014.996790
- Levgur M, Abadi MA, Tucker A. Adenomyosis: symptoms, histology, and pregnancy terminations. Obstet Gynecol. (2000) 95:688–91. doi: 10.1097/00006250-200005000-00011
PSTR The value of Truscreen (an artificial intelligence cervical cancer screening system) in high-risk HPV positive patients
- Lianmei Luo1,Jia Kong1,Jun Zhang1
1 Department of Obstetrics and Gynecology, Beijing Anzhen Hospital, Capital Medical University, Beijing, 100029, China
Email: lianmeimerry@vip.163.com Phone number: +8613581566336 Objective: To investigate the value of artificial intelligence cervical cancer screening system TruScreen (TS), an artificial intelligence cervical cancer screening system in high-risk human papillomavirus (HPV) positive patients in real clinical environment.
Methods: 318 patients with high-risk HPV positive in the gynecological clinic of our hospital from May 2020 to June 2021 were analysed retrospectively. Colposcopy was performed when there were colposcopy referral indications.
Results: Among the 318 patients, 203 were TS negative and 115 were TS positive, of which 84 were referred to colposcopy and biopsy under the guidance of colposcopy. Among the 318 patents, 74.53% (237/318) were single type HPV infection, and 25.47% (81/318) were more than two types of HPV infection. In terms of HPV types, the top 5 types are 52, 58, 51, 56 and 16. Hpv52 accounted for 27.4% (87/318), followed by HPV58, accounting for 17.30% (55/318). A total of 84 patients underwent colposcopy. The negative predictive values of TS and TCT screening for cervical cancer and precancerous lesions were 33.33% and 16.90% respectively; The positive predictive values were 88.41% and 92.31% respectively; The sensitivity was 85.92% and 16.90% respectively; The specificity was 38.46% and 92.31%, respectively. Among 251 patients with TCT < ascus and non- 16/ 18 high-risk HPV positive, 49 underwent colposcopy. The positive predictive value of TS for cervical cancer and precancerous lesions was 84.78% and the sensitivity was 92.86%.
Conclusion: This study shows that in the real clinical environment, TS has better sensitivity than TCT in cervical cancer screening, but less specificity than TCT. In the population with TCT results < ascus and non 16/18 HPV positive, TS screening can be considered as one of the means of hierarchical management. However, the current research sample size is small, which needs to be further discussed by large sample clinical research.
PSTR Diagnostic hysteroscopy for infertility: An incidental finding or misdiagnosis? Synchronous endometrial and ovarian cancer (SEOC).
- Priyanka Kathuria, Garima Yadav, Pratibha Singh
All India Institute of Medical Sciences, New Delhi, India Objective: To highlight the perplexity in diagnosis of endometriosis in an infertile female
Method: A 37 years old patient, P0010, presented with secondary infertility and dysmenorrhea (congestive and spasmodic) for last 2 years. She had no menstrual irregularities or coital difficulties and had adequate coital frequency. Spouse history was insignificant. There was a history of a spontaneous abortion at 1.5-month POG, 8 years ago. When she was conceived with Ovulation Induction. On examination the uterus was normal in size, anteverted, fixed with 6×6 cm cystic masses palpable in B/L adnexa with restricted mobility and tenderness. On further investigating, semen analysis was normal. HSG showed bilateral fill and spill. AMH was 0.47 ng/ml. CA 125 levels were 151 IU/L. USG pelvis revealed normal size uterus with ET-11 mm and Bilateral masses with typical picture of endometrioma with 6-7 cm in largest dimension. She was planned for diagnostic hysteroscopy and laparoscopy.
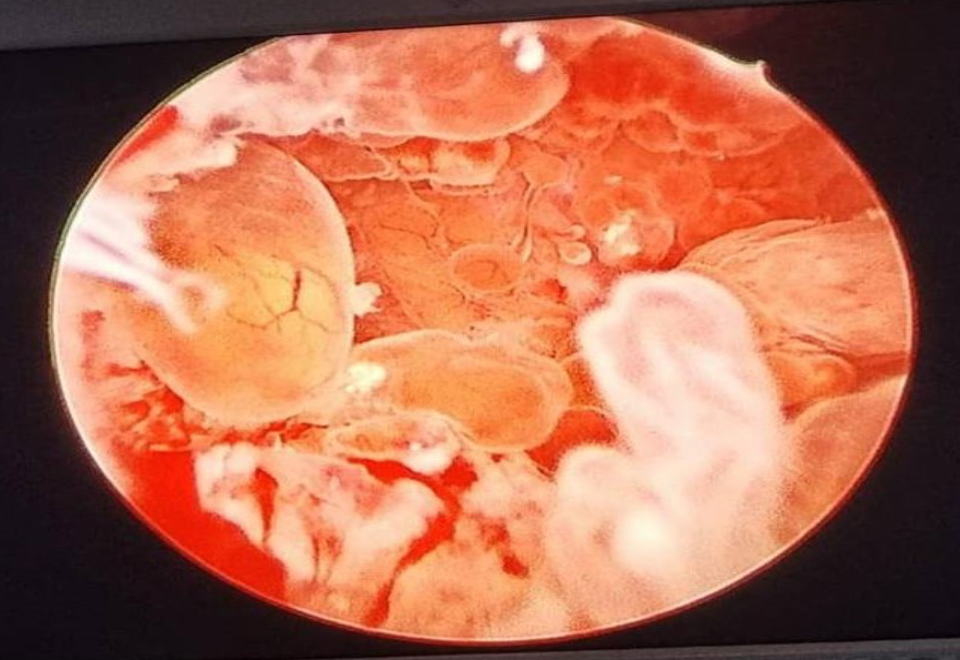
On hysteroscopy: the endocervical canal was normal. The uterine cavity volume was normal. Fluid filled vesicles like structures seen arising from all endometrial walls more on right side (fig. 1). B/L Ostia visualized, no current seen. Endometrial biopsy taken.
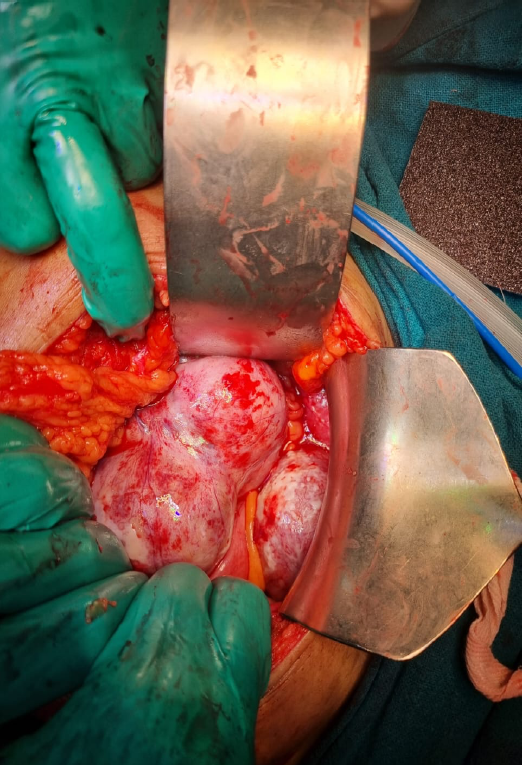
On diagnostic laparoscopy, bilateral ovarian masses suspicious of malignancy were seen. Decision for staging laparotomy was taken. Peritoneal fluid cytology sent. Bilateral multiloculated Ovarian masses seen (Fig. 2a). On the left side, 10x12cm bosselated a multiloculated solid cystic mass was removed and sent for frozen section which was suggestive of Borderline tumour (Fig. 2b). Similar mass of size 6x5cm was present on right side. Patient’s attendant was counselled about the prognosis. They opted for B/L Salpingo-oophorectomy. An infracolic omentectomy was performed and Multiple Peritoneal biopsies were taken.
Post-operative histopathology report disclosed: fluid cytology to be negative for malignant cytology, category II with Endometrioid borderline tumour. Endometrial biopsy showed Ca endometrium (endometrioid type) IHC demonstrated Tumour cells to be positive for oestrogen and progesterone receptors. Negative for WT1 –peritoneal biopsy /omental free of tumour, P53-normal expression (wild type).
Result: Ultrasound imaging may not be conclusive in large bilateral endometriomas.
- Conclusion: Synchronous endometrial and ovarian cancer of endometrioid type may be a rare presentation in females presenting with bilateral endometriomas.
Fig. 1– Diagnostic hysteroscopy revealed Fluid filled vesicles like structures arising endometrium globally. Final histopathology- endometrioid Ca endometrium.
Fig. 2a– Bilateral suspicious looking masses on laparotomy.
Fig. 2b– Left ovarian mass. 10*12 cm, bosselated, solid cystic mass.
Fig. 3– Gross specimen prior to frozen section.
PSTR The Role of Hysteroscopy in Patients with Recurrent Implantation Failure Before Starting In-Vitro Fertilization: A Systematic Review and Meta-Analysis
- I Wayan Agus Surya Pradnyana1, I Gde Sastra Winata2, I Gusti Bagus Mulia Agung Pradnyaandara1
1 Bachelor of Medicine, Faculty of Medicine, Udayana University, Denpasar, Bali, Indonesia
2 Gynecologic Oncology Division, Department of Obstetrics and Gynaecology Faculty of Medicine, Udayana University, Denpasar, Bali, Indonesia.
Email Address: suryapradnyana@student.unud.ac.id Phone number +62 81353912795 Objective: Recurrent implantation failure (RIF) remains the most challenging in-vitro fertilization (IVF) problem to treat. This is because the overall success rate is only approximately 30%. Hysteroscopy remains the gold standard for diagnosing and treating intra-uterine anomalies. This study aimed to evaluate the role of hysteroscopy (HC) in improving pregnancy outcomes in patients with RIF.
Methods: A systematic search was performed in PubMed, ScienceDirect, and Cochrane using MeSH terms if applicable and in accordance with the PRISMA guidelines, to determine the role of hysteroscopy compared to patient who didn’t undergo hysteroscopy. The Newcastle–Ottawa scale (NOS) was used to assess the risk of bias in this analysis and Review Manager 5.4 to calculate the result of 95% CI for the outcomes. The endpoints of interest were clinical pregnancy rate, live birth rate, implantation rate, and miscarriage.
Results: A total of 3 randomized controlled trial (RCT) and 5 cohort studies with 4,679 patients were included. Pooled analysis showed patients who underwent HC was associated with higher clinical pregnancy (OR 1.56, 95%CI 1.36-1.80), live birth (OR 1.44, 95%CI 1.20-1.72), lesser miscarriage (OR 1.27, 95%CI 1.01-1.61), and implantation rate (OR 1.32, 95%CI 1.09-1.59). Further subgroup analysis suggest HC had significantly greater effect in clinical pregnancy rate for patients with abnormal HC finding (OR 1.20, 95%CI 1.01-1.42), but no significant difference in live birth and miscarriage.
Conclusion: HC plays a significant role in improving clinical pregnancy rate, especially in patients with abnormal HC findings. HC also improves implantation rate, live birth, and lesser miscarriage in patients with RIF. Since the number of the study is still limited, further investigations are still needed to confirm the results.
PSTR Unruptured Ectopic Pregnancy with Risk Factor History of Miscarriage
- Ach Fahrur Rozi Mukti1, Arif Tunjungseto2
1. Residence, Obstetric and gynecologic Airlangga University/ Dr. Soetomo Hospital Surabaya
2. Fertility Divison Staff, Obstetric and gynecologic Airlangga University/ Dr. Soetomo Hospital Surabaya, Indonesia
email : hsbrurymukti@gmail.com phone +6281215719969 Objective: Ectopic pregnancy is a known complication of pregnancy loss that can carry a high rate of morbidity and mortality when not recognized and treated promptly. It may present with pain, vaginal bleeding, or more vague complaints such as nausea and vomiting. Aim this study is to describe a case of unruptured ectopic pregnancy so we can prevent delayed diagnosis and serious complications.
Methods: This study is case report about Mrs. N 32 years old female, who came consulting with a main complaint of abdominal pain and vaginal bleeding with positive serum hCG levels. This is patients second pregnancy with a previous history of miscarriage and contraceptives used. The Ultrasound result found an extrauterine gestational sac with no sign of free abdominal fluid. Patient then underwent diagnostic laparoscopy and a tubal pregnancy on left fallopian tube was found. A salpingectomy was then performed. A chromo perturbation was also performed resulting in a patent right fallopian tube
Result: The diagnosis of ectopic pregnancy has important clinical implications, but is easily misdiagnosed. The history of miscarriage in this patient could become the risk factor for misdiagnosing the ectopic pregnancy. Abdominal pain and vaginal bleeding from this patient can be caused by damage to the fallopian tubes due to implantation following inflammation that leads to pain and bleeding. The diagnosis is confirmed with a positive serum hCG levels and the ultrasound result. Diagnostic laparoscopy was then chosen due these facts. Chromo pertubation was performed to demonstrate the patency of the remaining right fallopian tube
Conclusion: Because the early diagnosis of ectopic pregnancy is essential, all sexually active women with a history of lower abdominal pain and vaginal bleeding should be referred to a hospital early for ultrasonography and measurement of serum concentrations of hCG to verify the diagnosis. Diagnostic laparoscopy is necessary if the clinical situation cannot be clarified or if the patient’s condition deteriorates.
PSTR Laparoscopy vs Laparotomy in Ectopic Pregnancy: A Study from General Hospital Prof. Dr. R. D. Kandou Manado in 2021-2022
- Lisa P. Susanto, Erna Suparman, Juneke J. Kaeng
Obstetrics and Gynecology Department Faculty of Medicine Sam Ratulangi University
General Hospital Prof. Dr. R. D. Kandou Manado, Indonesia Background: This study aims to compare the operative findings, mean duration of surgery, mean hospital length of stay, and post operative complications of laparoscopy compared to conventional laparotomy in the management of patients with ectopic pregnancy.
Methods: A retrospective cohort study was conducted at General Hospital Prof Dr. R. D. Kandou Manado from 2021 – 2022. A total of 142 patients surgically confirmed with ectopic pregnancy were included in the study. The main outcomes were operative findings (site of ectopic pregnancy), mean duration of surgery, mean hospital length of stay, and post operative complications (the number of patients experiencing both hypovolemic shock and anaemia). Hypothesis was formulated during data collection.
Results: During the study period, 142 patients presented with an ectopic pregnancy. Patients were divided into 2 groups: Group I (N=8) had their EPs removed laparoscopically; Group II (N=134) had a laparotomy. On the Group I, most patients were 25–29 years old (4.22%), resided same between outside and inside the city (2.82%), housewives (3.52%), senior high school as last education (4.22%), most of them were multiparous 2-4 (4.93%), and never done antenatal care (4.22%). On the Group II, most patients were 30–34 years old (75.35%), resided inside the city (53.48%), housewives (66.19%), senior high school as last education (71.13%), most of them were multiparous 2-4 (75.35%), and never done antenatal care (91.54%). Fallopian tube (91.6%) was the most common site for ectopic pregnancy followed with fimbriae (5.6%) and cornual (2.8%). There was clinically significant shorter length of hospitalization on laparoscopy group compared to laparotomy group (3.38 vs 4.40 days, p=0.057). However, mean duration of surgery was not significantly different (95.94 vs 99.38 minutes, p=0.752). No significant difference or notable hypovolemic shock findings found within ectopic pregnancy sites. However, there was a significantly notable difference of anemia rate between fimbriae, cornual, and tubal (87.5% vs 50.0% vs 24.6%, p <0.001).
Conclusions: Laparoscopic is a safe and effective surgical management option for patients with ectopic pregnancy without complications. We conclude that Laparoscopy should be the choice in un- complicated ectopic pregnancy. Laparoscopy provides benefits as it offers shorter duration of surgery and hospital stays with no life-threatening post-operative complication (hypovolemic shock and anemia) with cosmetically better scar compared to conventional laparotomy. However, due to limited samples, study with better quality (i.e., RCT) bigger samples should be conducted to confirm laparoscopy superiority in better power and sample adequacy.
PSTR Intrauterine Device (IUD) Translocation in Young Women: A Case Report
- Joanna F. Kapojos, Linda M. Mamengko, Joice M. M. Sondakh
Department of Obstetrics and Gynaecology
Faculty of Medicine Sam Ratulangi University
General Central Hospital Prof. Dr. R. D. Kandou, Manado, Indonesia Background: Intrauterine device (IUD) translocation transposes the IUD from the initial intrauterine placement to another place within or outside the uterus. This might happen spontaneously or due to several factors, such as uterine contractions, pregnancy, or IUD insertion error. The prevalence of IUD translocation, in general, is very low, and the incidence rate is about 0.1 – 8% from the overall IUD acceptor, making this case very rare.
Methods: To report a case of IUD translocation, located outside the uterine cavity.
Results: A young P1A1 woman with an IUD translocated outside the uterine cavity with a history of Cesarean section in 2017, this woman decided to use an IUD for her contraception six months after the Cesarean. In 2019 the patient was diagnosed with a ruptured ectopic pregnancy and left salpingo oophorectomy was done. In 2021 the patient decided to remove the IUD but the attempt failed, translocation of the IUD was suspected, and pelvic Multi-slice Computerized Tomography (MSCT) was done, suggesting extrauterine IUD placement on the right adnexa up to the posterior part of the uterus. Laparoscopic extraction of the IUD was decided, during the operation the IUD was found to be covered by omentum and part of the intestine, adhesiolysis was done by a digestive surgeon. The IUD was then extracted on the right adnexa.
Conclusion: IUD translocation is a rare complication. Several known mechanisms are: insertion complications, uterine contraction, and myometrial erosion. While ectopic pregnancy is one of the side effects of IUD usage. IUD translocation can be evaluated by pelvic X-Ray and abdominal/pelvic CT scan making sure the location of the IUD. The preferred extraction method is laparoscopy. Even though IUD is one of the most used contraception methods and insertion can be done in primary health care units by a trained health care provider, caution should always be in mind for every insertion. In this case the translocated IUD was found in according to the imaging studies.
PSTR Clinical characteristics of infertile patients undergoing laparoscopic adhesiolysis: a descriptive study in a single center
- Astawa Pemayun TG, Putra Adnyana IB, Suardika A, Darmayasa M, Diningrat MA, Putra Adnyana IBP
Royal IVF Clinic, Bali Royal Hospital, Denpasar, Bali, Indonesia e-mail: tjokgedeap@gmail.com Objective: Infertility has been attributed to some pelvic pathologies such as endometriosis, gynecologic tumours, pelvic inflammatory disease, etc. The advancement of laparoscopic techniques has enabled definitive diagnosis and treatment for these women. Despite this development, the decision to do surgery remains controversial, especially in patients with minimal clinical symptoms. In this study, we aim to present clinical characteristics of patients treated with laparoscopic surgery prior to infertility treatment.
Methods: This study was conducted in Royal IVF Clinic, Bali Royal Hospital, Denpasar, Bali. We performed 318 laparoscopic gynecologic surgeries during the 2021-2022 period for various indications. We included 25 patients with a duration of infertility more than 2 years aged 20-35 years old, who underwent laparoscopic surgery due to suspicions of pelvic pathologies. Decision for laparoscopic surgery was based on ultrasound or hysterosalpingography findings suggesting non-patent fallopian tubes, hydro salpinges, or pelvic adhesion. Data were collected from hospital medical records.
Results: Clinical symptoms and signs including transvaginal ultrasound examination were assessed. All patients included had tubal pathology in the form of grade 2-4 hydrosalpinx and pelvic adhesion during laparoscopic surgery. Most patients experienced chronic pelvic pain (60%; n=15) and retroflexed uterus with stiffness (60%, n=15). Less common findings were menstrual pain (24%, n=6) and slinger pain (8%, n=2). From ultrasound examination, we found sliding sign negative (20%, n=20), echogenic filament (76%, n=19), free fluid in the Douglas pouch (80%, n=20) and hypoechoic tubular structure in adnexa (96%, n=24).
Conclusion: Laparoscopy is a minimally invasive surgery with extensive application in the field of infertility. This technique allows clear visualization of female organ, and treatment to many pelvic pathologies. Despite its benefits, it may not be suitable for some patients, considering its high-cost and limited availability. Thus, the decision to operate should also consider clinical aspects of the patients, to ensure patients’ satisfaction and treatment efficiency.
References:
- Cheong y, Saran M, Hounslow JW, Reading IC. Are pelvic adhesions associated with pain, physical, emotional and functional characteristics of women presenting with chronic pelvic pain? A cluster analysis. BMC Women’s Health 2018;18(11).
- Hammoud A, Gago A, Diamond MP. Adhesions in patients with chronic pelvic pain: a role for adhesiolysis. Fertil Steril. 2004;82(6).
- Diamond MP, Bieber E. Pelvic adhesions and pelvic pain: opinions on cause-and-effect relationship and when to surgically intervene. Gynaecological Endoscopy. 2001; 10:211-216.
- Moro F, Mavrelos D, Pateman K, Holland T, Hoo WL, Jurkovic D. Prevalence of pelvic adhesins on ultrasound examination in women with a history of Cesarean section. Ultrasound Obstet Gynecol. 2015; 45:223-228.
- Ayachi A, Jendoubi A, Mkaouer L, Mourali M. The value of ultrasound sliding sign technique in predicting adhesion related complications: The point of view of the gynecologist and the anesthesiologist. Saudi J Anaesth 2017; 11:250-2.
PSTR Challenges of morbidity management involving ruptured abdominal pregnancy in the third trimester: a case report
- Yona S. Pardede1. Bismarck J. Laihad1, Frank M. Wagey1
1Departement of Obstetrics and Gynaecology, Faculty of Medicine Sam Ratulangi University General Central Hospital of Prof. Dr. R. D Kandou, Manado, Indonesia. Background: Abdominal pregnancy is a very rare form of ectopic pregnancy in which the products of conception can be found in the pouch of Douglas, on the omentum, on the pelvic sidewall, the liver, the diaphragm, and even the great abdominal pelvic vessels. The incidence of ectopic pregnancy is 1:10,000 to 1:30,000 pregnancies and abdominal pregnancy accounts for approximately 1% of the ectopic pregnancies. It is important make an early diagnosis of abdominal pregnancy to avoid morbidity and mortality. Delayed diagnoses are mainly the result of difficulties in clinical assessment caused by a variety in presentation. Early laparoscopic management can be done to prevent complication. In this case report, challenges of the management of the morbidity involving abdominal pregnancy in the third trimester will be discussed.
Objective: To discuss the challenges of the management of morbidity involving ruptured abdominal pregnancy in the third trimester and the role laparoscopy to prevent complications.
Methods: A Case Report
Results: A female patient, 40 years of age, G2P1A0 with 25-26 weeks of gestation, was referred from a tertiary hospital with the suspicion of an abdominal pregnancy and anemia. This patient was previously known to have had an ectopic pregnancy at 10 weeks’ gestation and was advised to proceed to a hospital with laparoscopic facilities. The patient never checked on her pregnancy due to inadequate knowledge of the risks. An evaluation was performed later and an extrauterine pregnancy with a placenta that was attached to the posterior side of the uterus and to the pouch of Douglas, including severe oligohydramnios, and suspected congenital abnormalities was diagnosed. There appeared to be free fluid in the hepato-spleno-renal space with an image of hydronephrosis of the right kidney. Laparoscopy could not be performed due to unstable hemodynamics. Treatment was performed by stabilizing the general condition and transfusion of packed red blood cell (PRC) and emergency laparotomy. Due to massive bleeding, a total hysterectomy was performed. The placenta was partially removed and some of it was left in the pelvic cavity.
Conclusion: Laparoscopic management can be very beneficial for in the early treatment of abdominal pregnancy. Many hospitals in Indonesia cannot perform laparoscopic operative procedures due to several factors such as inadequate hospital facilities, shortage of personnel trained in laparoscopic surgery, overall cost of the laparoscopic procedure and lack of insurance coverage. There is also a lack of knowledge by the patients concerning this procedure. In patients with these or similar symptoms, the delay in response causes the patient to experience high morbidity. The early treatment in cases of ectopic pregnancy, can prevent morbidity and mortality in patients, especially in abdominal pregnancies.