Authors / metadata
DOI : 10.36205/trocar3.2023006
Abstract
Objective: To demonstrate technique of a delayed laparoscopic hysterectomy in the management of placenta accreta in a postpartum setting.
Design: Stepwise demonstration of the technique with narrated video footage.
Setting: The incidence of placental accreta spectrum disorder has risen over the years due to the increasing number of caesarean sections being performed. A caesarean hysterectomy for placenta accreta is usually performed through a laparotomy. There is a lack of consensus in performing this procedure laparoscopically due to the increased risk of bleeding and the size of the uninvoluted postpartum uterus.
A laparoscopic approach may be considered for delayed surgical management of abnormal placentation, the key factors for success are a multidisciplinary approach, availability of skilled laparoscopic surgeons, appropriate equipment and resources and a tertiary hospital setting.1 Only case reports have been published about the laparoscopic management of these placental adhesive accreta spectrum disorders.2-3.
Patients or participant: Written consent was obtained from the patient and an ethics approval was granted from the local Ethics Committee through Townsville University Hospital, Australia.
Case Report: We present the case of a 42-year-old Para 5 patient referred from a regional hospital with ongoing vaginal bleeding 4 weeks following a caesarean section for placenta 1accreta, the diagnosis was made intra-operatively at caesarean section and adherent placenta was only partially removed owing to blood loss totaling 1500 ml. She had a BMI of 37 with a complex obstetric history, including a first delivery at 24 weeks for incompetent cervix, followed by 4 lower segment caesarean section for her subsequent deliveries. Her past medical history includes a gastric sleeve for weight loss, appendicectomy and a D&C.
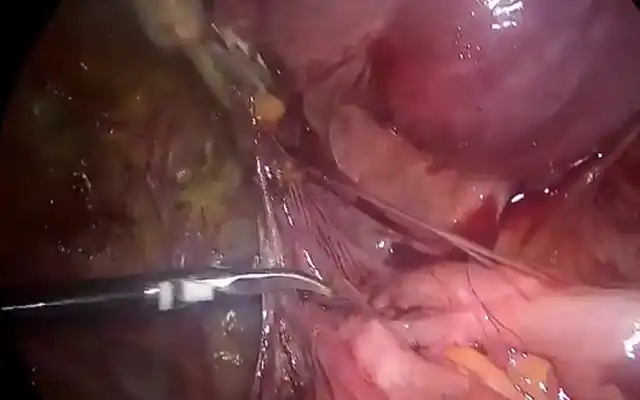
Laparoscopic hysterectomy was performed with three 5mm laparoscopic trocars and a 10mm port using a 30-degree endoscope. In this video, we describe our technique for a delayed laparoscopic hysterectomy of placenta accreta in a postpartum setting. Intra-operatively, bilateral ureteric catheterization was performed. The uterus was a bulky 18-week size uterus that was occupying the pelvis limiting access to the pelvic side walls. There was also a residual placental bulge on lower segment with a moderately adherent bladder from the Caesarean section. Blood loss was 100mls and specimen were removed from the vagina. No complications were encountered during the hysterectomy. The patient was discharged home day 1 following the procedure.
There were several key strategies to success:
Ureteric catheterization and ureterolysis
Adequate development of potential pelvic spaces
Ligating the uterine artery at its origin
Late insertion of uterine manipulator after ligation of bilateral uterine arteries
Conclusion: This video highlights the ability to perform a delayed (post-partum) laparoscopic hysterectomy for placenta accreta, a minimally invasive alternative to the usual laparotomy.
Introduction
Placenta accreta spectrum disorder (PASD) is defined as the abnormal attachment of all or part of the placenta to the uterus (1,2) Depending on the invasion of trophoblast past the normal decidual-myometrial junction zone it can be classified into superficial placenta accreta, where it attaches itself to attaches to the myometrium without invasion, increta where there is myometrial invasion, and percreta which involves penetration through the uterine serosa, potentially into surrounding organs (3).
It is a fairly rare condition, with a recent meta-analysis suggesting a prevalence rate of 0.01-1.1%, albeit increasing in incidence over the last few years (4,5). The incidence may be attributed to the increase in rates of caesarean sections, placenta previa, utilization of assisted reproductive technologies, surgeries of the uterus causing endometrial scarring, and advanced maternal age in pregnancy (6,8). This condition poses a significant risk patient’s mortality and morbidity, with complications such as massive hemorrhage, caesarean hysterectomy, cystotomy, ureteric trauma, infection, multisystem organ failure, disseminated intravascular coagulation, intensive care admission and death (4,5,9). In this case study we are looking at a technique of delayed hysterectomy in the post- partum period, using minimally invasive laparoscopic surgery as an alternative approach (10).
Case
The patient was a 42-year-old G8P5 with a complex obstetric history who was referred to our tertiary unit for potential retained products of conception after an elective lower segment caesarean section.
Her obstetric history included:
G1: Neonatal death at 24 weeks of age from cervical incompetence.
G2: Live birth at 39 weeks of age after an elective cerclage
G3: Live birth at 36 weeks of age following a double embryo transfer
G4: First trimester miscarriage at 8 weeks managed with suction dilatation and curettage
G5: Miscarriage at 5 weeks
G6: Live birth at 37 weeks of age. Elective lower segment caesarean section but placenta was found to be very adherent at time of delivery.
During her last elective caesarean section, the placenta was only able to be partially evacuated, as it was morbidly adherent. A Bakri balloon was required to tamponade the lower segment, following a postpartum hemorrhage of 1500 ml. Despite having initial bleeding that was minimal, four weeks post-partum she started having intermittent erratic vaginal bleeding. Ongoing ultrasound surveillance revealed vascular retained products of conception with a large heterogenous echogenic mass in the lower segment with an almost complete incursion into the myometrium posteriorly as well as posterior cervical stroma. Following a lengthy discussion with the patient with management options, the patient made an informed decision to proceed with a laparoscopic hysterectomy.
She also had iron deficiency anemia during her pregnancy and had iron transfusions at gestational age of 4 weeks. She also has a BMI of 37. Her past surgical history included spinal fusion C 4/6 at age 13, knee construction, appendicectomy, gastric sleeve surgery, perianal abscess draining. She underwent a delayed laparoscopic hysterectomy and bilateral salpingectomy with ovarian conservation for placenta accreta with procedural methods highlighted below, with no further complications and was discharged the next day.
Method
An anesthetic assessment was undertaken to ensure fitness for surgery. The vascular and urology team were also notified beforehand. On the day of surgery, a cystoscopy was first performed to exclude placenta percreta and bilateral ureteric catheterization was performed. Intraoperatively, the uterus was 18 weeks of size bulky in appearance stretching from one lateral pelvic side wall to the other. Anatomic abdominal survey including the fallopian tubes and ovaries was normal. A residual placental bulge was noted on the lower segment ostensibly from the abnormal placentation. There were multiple omental adhesions to the anterior abdominal wall.
Abdominal entry with Veress needle at Palmer’s point was used to establish pneumoperitoneum. The round ligament was divided and the para vesical and pararectal spaces developed to isolate the uterine artery at the origin from the internal iliac artery which was identified in relation to the obliterated umbilical ligament. Bilateral ureterolysis was commenced at the pelvic brim past the ureteric tunnel. The medial pararectal space of Okabayashi was further developed to further lateralize the ureters. Subsequently the vesicouterine space was developed along with the medial and lateral para vesical spaces to mobilize and dissect the densely-adherent urinary bladder using a ‘low-lateral’ approach.
The uterine vessels were coagulated using an advanced Bipolar device. As the right superior vesical artery was contributing to an unusually enlarged vaginal artery it was secured it as well. Before continuing with bladder dissection, the uterus was completely de-vascularized. The uterine manipulator was inserted only after this point. A primary colpotomy was performed to further skeletonize the uterine vessels and these were coagulated at the traditional coagulation point.
A PDS 1 suture was used for uterosacral suspension reconstituting the peri-cervical ring, pubo-vesical and rectovaginal fascia. The V-loc 0 suture was used for two layered vault closure. The uterus was delivered easily through the vagina without morcellation. Bleeding from peritoneal bleeders was secured with surgical clips; the generalized vault ooze needed pressure and FLOSEAL hemostatic agent. Total estimated blood loss for this procedure was 100ml.
Discussion and conclusion
Some of the risk factors this patient had that may have attributed to having placenta accreta are complex obstetric history that involved multiple cerclage due to cervical incompetence, multiple invitro fertilization techniques for conception, advanced maternal age as well as parity. The mainstay of managing placenta accreta is a prenatal assessment of location, depth of invasiveness, using ultrasonographic imaging modality as well as MRI and a multidisciplinary approach of delivery planning (11,12).
Generally speaking, there are four ways to manage Placenta Accreta Spectrum disorder, the extirpative method, caesarean section hysterectomy, conservative management, and one-step conservative surgery (12). Conservative uterus preserving methods such as methotrexate administration and long-term antibiotics were considered.
Conservative management although currently portrays conflicting studies, and considerations for novel approaches for preservation of fertility, still poses significant risk of complications in women in the post-partum period with an increased risk of morbidity, mortality, infections and requiring delayed hysterectomy (13,14,15,16). A hysteroscopic resection was considered but was deemed would be a difficult approach due to the large exophytic mass obstructing the lower segment. An open caesarean hysterectomy remains the reference treatment for placenta accreta, considering reproducibility, rate of morbidity and complications in the other options mentioned (9,12). Although this may be the preferred method of management, there are studies that show relativity high morbidity rates, with significant outcomes of needing transfusion, cystotomy, ureteral injuries and infection (9,10,17).
There have been several case reports that highlight laparoscopic method of managing placenta accreta which have demonstrated good outcomes, with minimal
bleeding and injury to the bladder (18,19,20). The key factors for success are a multidisciplinary approach, availability of skilled laparoscopic surgeons, appropriate equipment and resources and a tertiary hospital setting (18,19,20). Surgically, the techniques to reduce complications include ureterolysis, ligating the uterine arteries along with other contributing branches at the origin from the internal iliacs, and delayed manipulation of uterus only after stepwise devascularization has been achieved. Ureterolysis along with ureteric catheterization is a vital step in this procedure to minimize risk of ureteric trauma owing to their proximity to the widened and broad lower uterine segment. Furthermore, delayed insertion of a uterine manipulator also assists with reducing blood loss (21Complete internal iliac artery ligation controls the blood that flows through the placenta via the cervical and vaginal arteries and therefore is considered superior to just uterine artery ligation (22).
In conclusion, placenta accreta spectrum disorder is a condition attendant with significant perioperative morbidity which can be offset to a certain extent with early recognition with ultrasound or MRI, proactive perioperative planning, a multidisciplinary approach and targeted surgical technique to ensure the best post-partum outcomes. Compared to laparotomy, delayed laparoscopic hysterectomy for placenta accreta spectrum disorder is a safe and effective alternative as it results in a lesser intraoperative blood loss, wound infections, postoperative pain, earlier mobilization, shorter hospital stay, as well as a faster return to normal activities (23.
Acknowledgments: We would like to thank Dr David Watson and Dr Cecilia O’Brien for their expertise in providing high quality ultrasound images to help guide our management of this patient.