Authors / metadata
DOI: 10.36205/trocar4.2023003
Abstract
Nonpuerperal uterine inversion (NPUI) is of extremely rare occurrence. It mostly results due to benign etiologies like leiomyomas but can be associated with malignancies as well. We report a case of chronic nonpuerperal uterine inversion where successful uterine reposition and repair was done by a combined vaginal and laparoscopic approach. A 35-year woman presented with complaints of heavy menstrual bleeding and dysmenorrhea. Her uterine inversion was promptly diagnosed on clinical examination and a definitive surgery was then performed. To begin with prolapsed submucous myoma was shaved off vaginally by cauterization and myoma bed was sutured with vicryl. Following this vaginal reposition was attempted which failed. Owing to this decision to perform Haultain’s procedure was made. Midline vertical 3cm incision was made over the constriction ring. After the constriction ring was released an upward push from vaginal end combined with simultaneous upward traction on round ligament resulted in reposition of uterus. Uterine incision was sutured with continuous non interlocking barbed sutures. Postoperative period was uneventful and patient was discharged with advice regarding future conception. It should be taken into consideration as one of the differential diagnoses in females with mass protruding through vagina. A high index of suspicion is essential for prompt diagnosis and appropriate surgical intervention.
Introduction
Nonpuerperal uterine inversion (NPUI) is a rare clinical condition which poses challenge in diagnosis as well as surgical management. The precise incidence of nonpuerperal uterine inversion (NPUI) is unknown. NPUI may occur by the intrauterine tumor’s weight, manual traction on the tumor, or elevated intra-abdominal pressure due to sneezing, coughing, and straining. Patients of NPUI present with foul-smelling vaginal discharge or irregular vaginal bleeding, anemia, abdominal cramps, pelvic discomfort, and fullness of the vagina or pressure in the vagina. Accurate clinical examination, imaging, histopathological evaluation, examination under anesthesia, laparoscopy all aid in the diagnosis of NPUI. Stages 2, 3, and 4 inversions are probably going to be more difficult, although stage 1 inversions can have more chances of successful uterine reposition. However, where uterine reposition fails hysterectomy remains the only option. Various surgical approaches for NPUI have been described so far which include abdominal, vaginal, combined abdominal-vaginal, laparoscopic. We report a case of chronic nonpuerperal uterine inversion where successful uterine reposition and repair was done by a combined vaginal and laparoscopic approach.
Case description
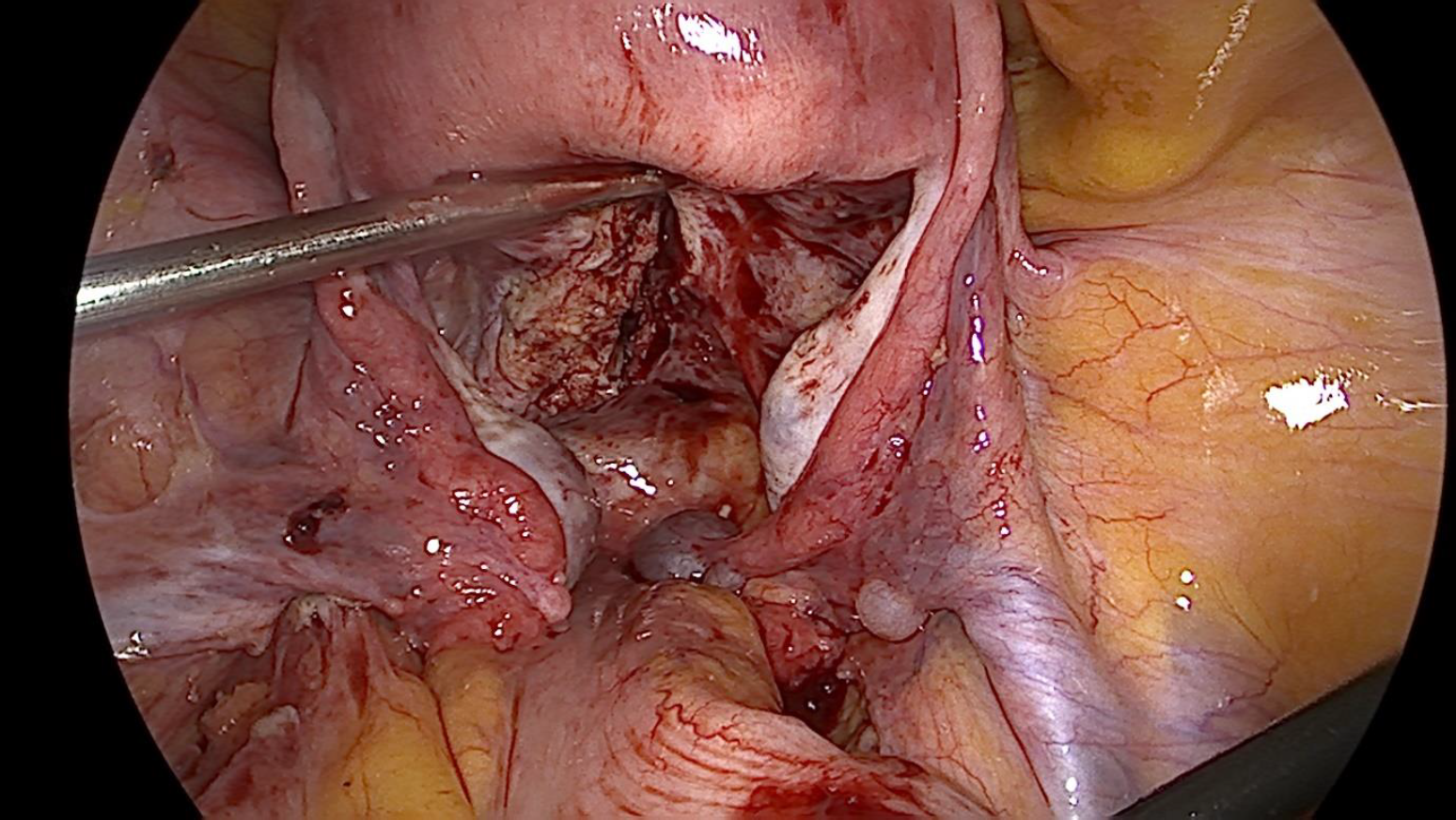
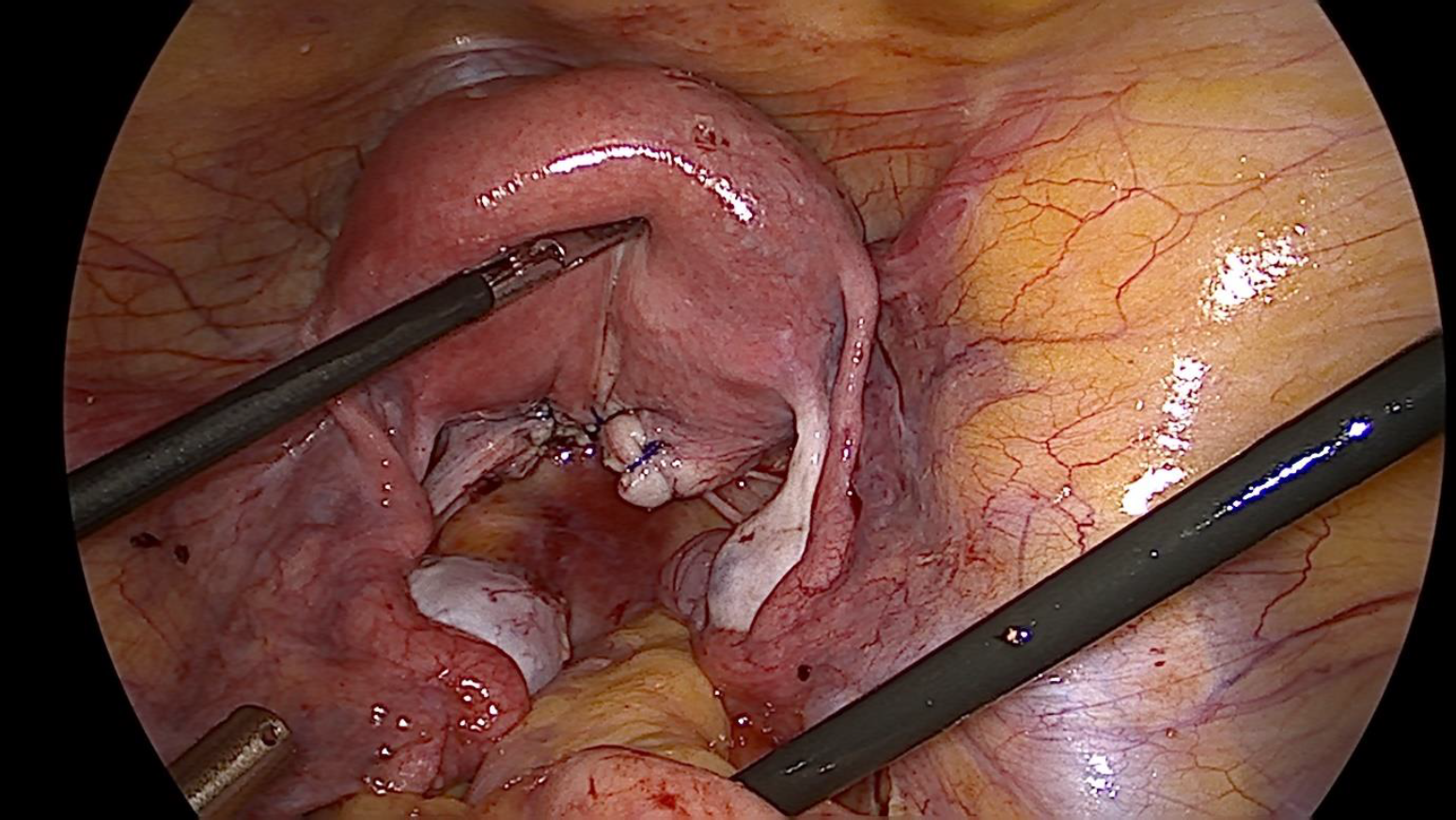
A 35yrs female reported to us with history of heavy menstrual bleeding for 2 years. Her ultrasound report done 2 years back was suggestive of 3 cm submucous myoma for which she was advised surgery but she did not follow up for the same. Over 2years her complaints increased with dysmenorrhea. However, the dysmenorrhea increased significantly over last few months and patient noticed a mass coming out of the vagina 1 month back for which she went to her family physician. She was advised by family physician to do ultrasound which was s/o Uterovaginal prolapse. She was then referred to us for further evaluation and management. On local examination in OPD, a 5×6 cm mass was seen protruding from the vagina with another globular swelling 3x3cm in size attached to the larger mass at the cranial end. On per speculum examination, neither a uterine sound nor a gloved finger could be passed around the pedicle of protruding mass encircled by the cervical rim. Uterine fundus was not palpable on bimanual examination. This raised a clinical suspicion of uterine inversion due to a large submucous myoma. Also, two small dimples were seen equidistant from the midline at 3 o clock and 9 o clock position on the cranial swelling, which were suspected to be tubal ostia. Hence, the patient was counselled for laparoscopic surgical repair of the chronic inversion. On doing laparoscopy, no uterine fundus was seen and medial ends of all cornual structures were pulled in the center at the constriction ring formed by uterine isthmus and cervix. This confirmed the diagnosis of uterine inversion. To begin with, the prolapsed submucous myoma was shaved off vaginally by cauterization and the endo-myometrial junction line which was actively bleeding was sutured with Vicryl™. Excessive use of cautery over the endometrial lining was avoided as the patient wanted future fertility.
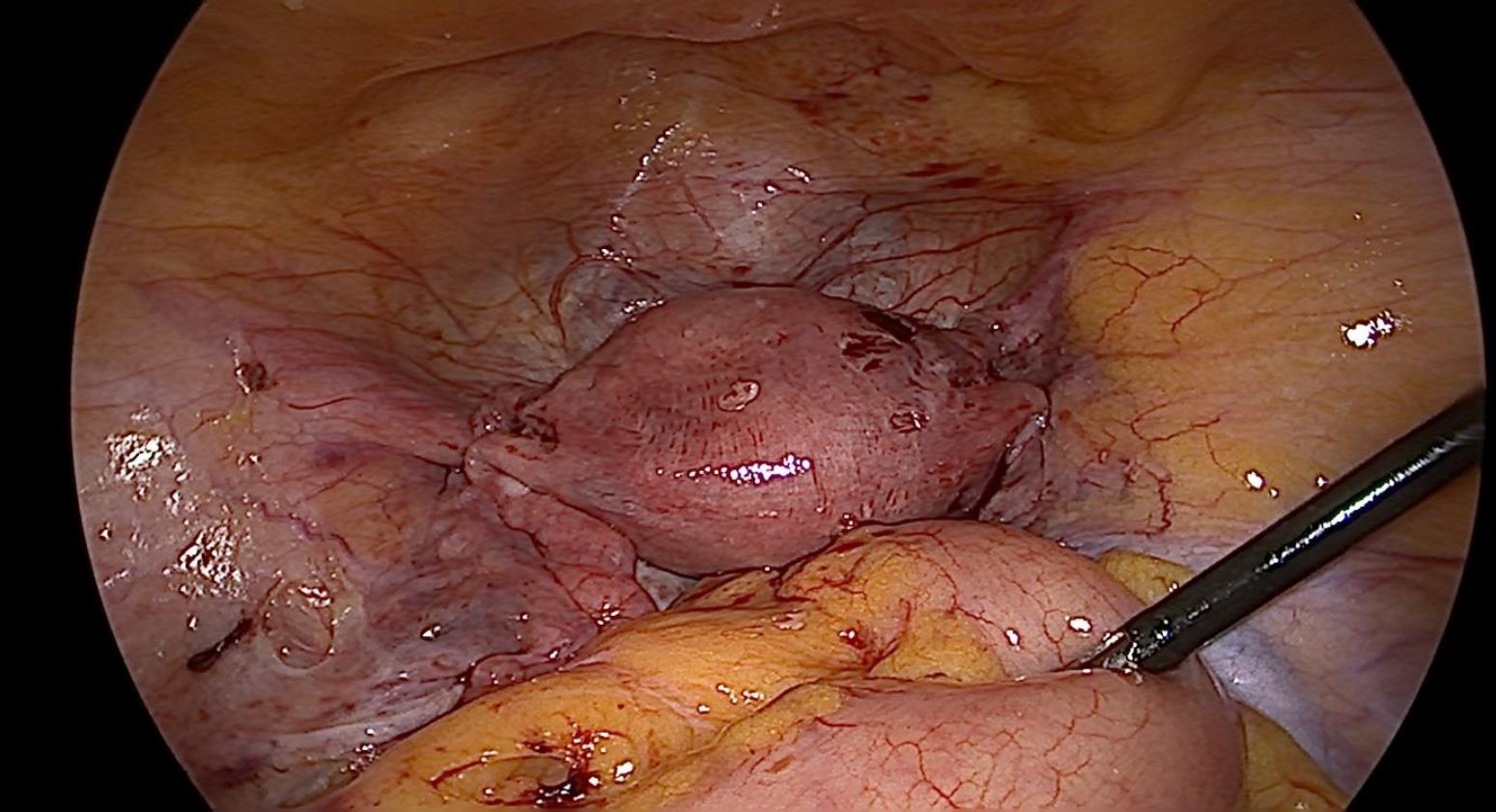
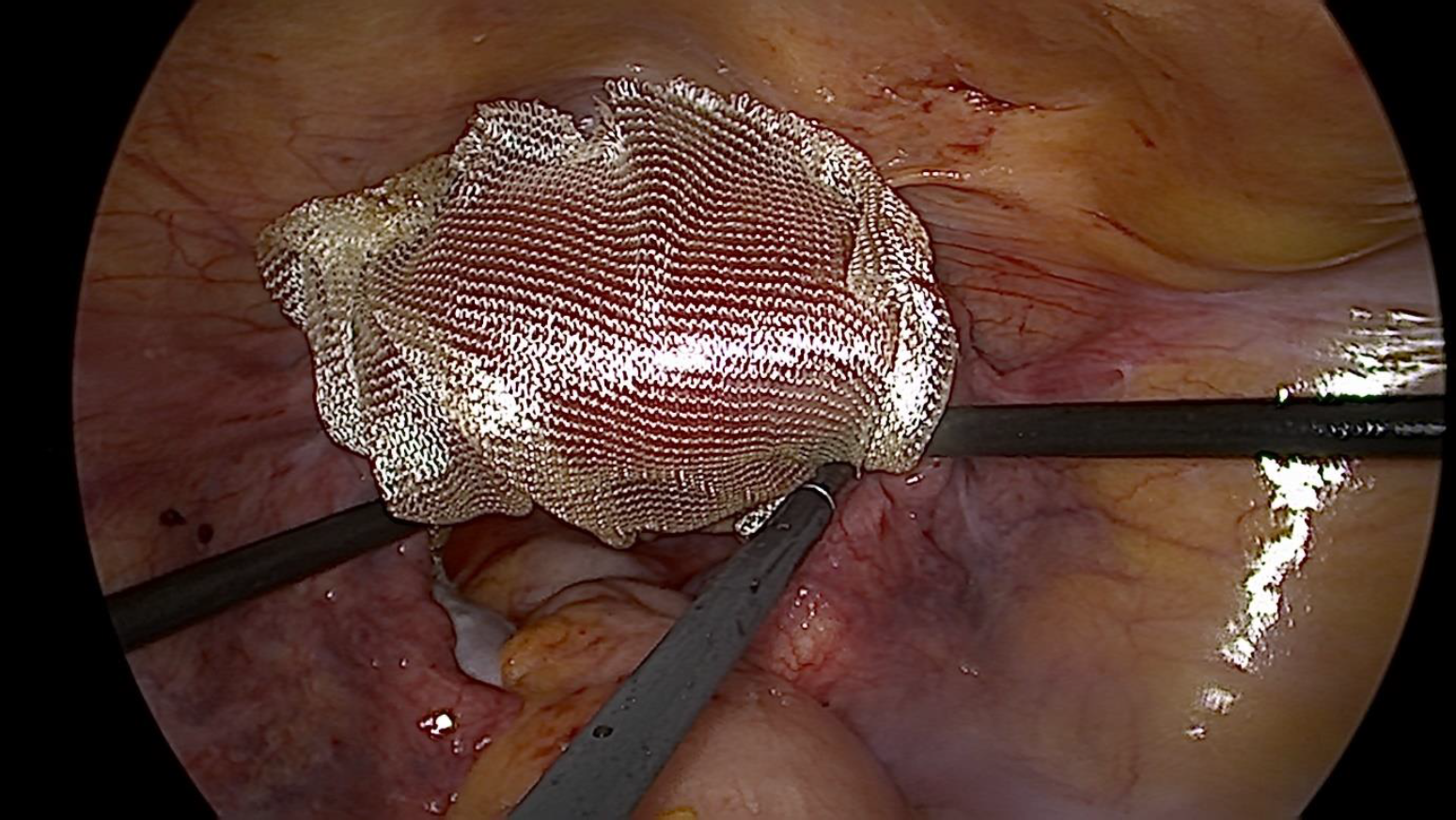
Bilateral ureters were visualized and traced caudally till the level of uterosacral ligaments. Lateralization of ureters was performed. Following this, vaginal reposition of the prolapsed fundus by pressure was attempted which failed. Owing to this, a decision to perform Haultain’s procedure was made. The posterior part of the constriction ring was made prominent by inserting a sponge on holder in the vagina. Vasopressin was infiltrated over the posterior part of the ring in the midline using Pisat’s Visual Vasopressor Injection Needle (VVIN).1 Midline vertical incision approximately 3 cm in length was made over the constriction ring. After the constriction ring was released an upward push from vaginal end combined with simultaneous upward traction on round ligament which resulted in reposition of uterus. Uterine incision was sutured with continuous non interlocking barbed sutures. Adhesion barrier was placed over the uterine incision line. Intra uterine pediatric foleys catheter was kept postoperatively for 3 days. Postoperative period was uneventful and patient was discharged with advice regarding future conception.
Etiology
In a study by Herath RP et al, leiomyoma was the most frequent cause of NPUI, accounting for 86 (56.2%) of the cases.3 Another study by Takano et al observed 92% cases were associated with uterine tumors of which 71.6% were leiomyomas and 20% were malignant tumours.4 Amongst the malignant causes leiomyosarcomas are the most common, followed by endometrial carcinoma, rhabdomyosarcoma, malignant mixed müllerian tumor, and endometrial stromal sarcoma 5.
Diagnosis
The clinical diagnosis of non-puerperal uterine inversion is challenging and a high index of suspicion is necessary for accurate diagnosis. Important clinical signs that aid in diagnosis are absence of identifiable cervical rim around the proximal portion of the mass (in case of complete inversion), failure to find the opening of uterine cervix or probe the endometrial cavity, cupping of fundus on bimanual palpation (in incomplete inversion cases), no palpable uterine fundus on per rectal examination. Both the diagnosis of NPUI and the identification of its etiology can be aided by ultrasound imaging. Incomplete uterine inversions show sonographic signs of a “Y”-shaped uterine cavity in the longitudinal plane. The base of “Y” indicates the noninverted endometrial lining. Complete inversion in the longitudinal view on ultrasound results in a “U”-shaped structure, with the limbs of the “U” standing in for the entire inverted endometrial lining.
The diagnosis of NPUI using magnetic resonance imaging (MRI) has been found to be sensitive. U-shaped uterine cavity, thicker and inverted uterine fundus on a sagittal view, and a “bull’s eye” arrangement on the horizontal section are the three distinct observations noted on MRI in cases of uterine inversion. In case of difficulty in clinical diagnosis and interpretation of imaging findings comes the role of examination under anesthesia, laparoscopy and biopsy of the vaginal mass prior to definitive surgical management. Malignancies though rare have been associated with NPUI hence histological assessment of the mass is justified prior to definitive surgery unless there is an obvious cause like fibroid as in our case.
Management
Techniques of uterine reposition such as Huntington (traction on round ligaments abdominally), Haultain (abdominal – posterior incision), Spinelli (vaginal- posterior incision), and Kustner’s (Vaginal- anterior incision) operations were traditionally described for puerperal inversions. Subsequently, the above procedures have been used to treat NPUI also. Our case was managed with a combined vaginal and laparoscopic approach for uterine reposition and repair. Vaginal myomectomy was done which resulted in debulking of the uterus. This was followed by laparoscopic Haultain procedure for uterine reposition and repair. As per a study conducted by Herath RP et al, Haultain procedure seems to be the most successful method to achieve repositioning in 18.0% cases of NPUI.2 This study also found that majority 48.8% were managed by only abdominal approach while 27.1% had both abdominal and vaginal approach. The majority 39.7% required abdominal hysterectomy while 15.0% had uterine repair after repositioning.3
Future Outcome
Unfortunately, future fertility has not been found to be satisfactory following uterine reposition in NPUI cases. A case was reported by Irani et al where the uterus was repositioned with the Haultain procedure but the woman failed to conceive for two years after the operation.6 Similarly Herath RP et al. failed to find any evidence of successful pregnancy following repositioning of a nonpuerperal uterine inversion.3 However, following successful uterine reposition in NPUI cases women should be counselled regarding associated risks in future pregnancy like uterine rupture, cervical incompetence. Pregnancies following NPUI repair may warrant need of prophylactic cervical cerclage and need for elective caesarian section near term. Also, in pregnancies following NPUI repair complicated with low-lying placenta morbidly adherent placenta is to be ruled out with imaging.
Discussion
Only one-sixth of all occurrences of uterine inversion are non-puerperal, and the majority of cases of uterine inversion occur during puerperium 2. The mechanism of non-puerperal uterine inversion is not clear. However, the chronic downward traction force exerted by the submucous myoma situated at the fundus caused inversion in our case.
Conclusion
NPUI is rare. It should be taken into consideration as one of the differential diagnoses in females with mass protruding through vagina. A high index of suspicion is essential for early diagnosis and appropriate surgical intervention so as to avoid devastating consequences.
References
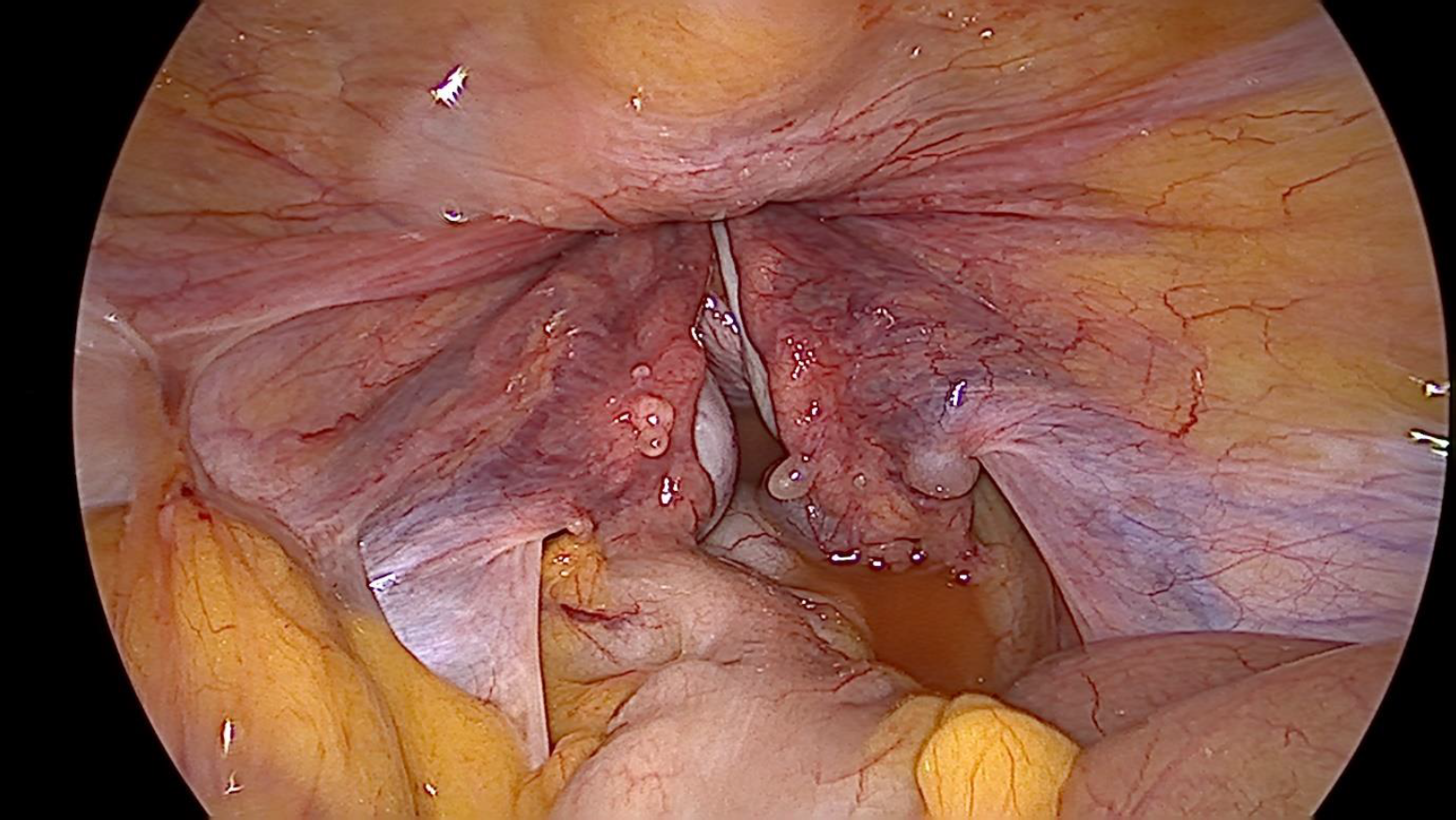
Figure 1. Submucous myoma with uterine inversion
Figure 2. Laparoscopic view -Uterine fundus not seen, medial ends of all cornual structures pulled in the constriction ring
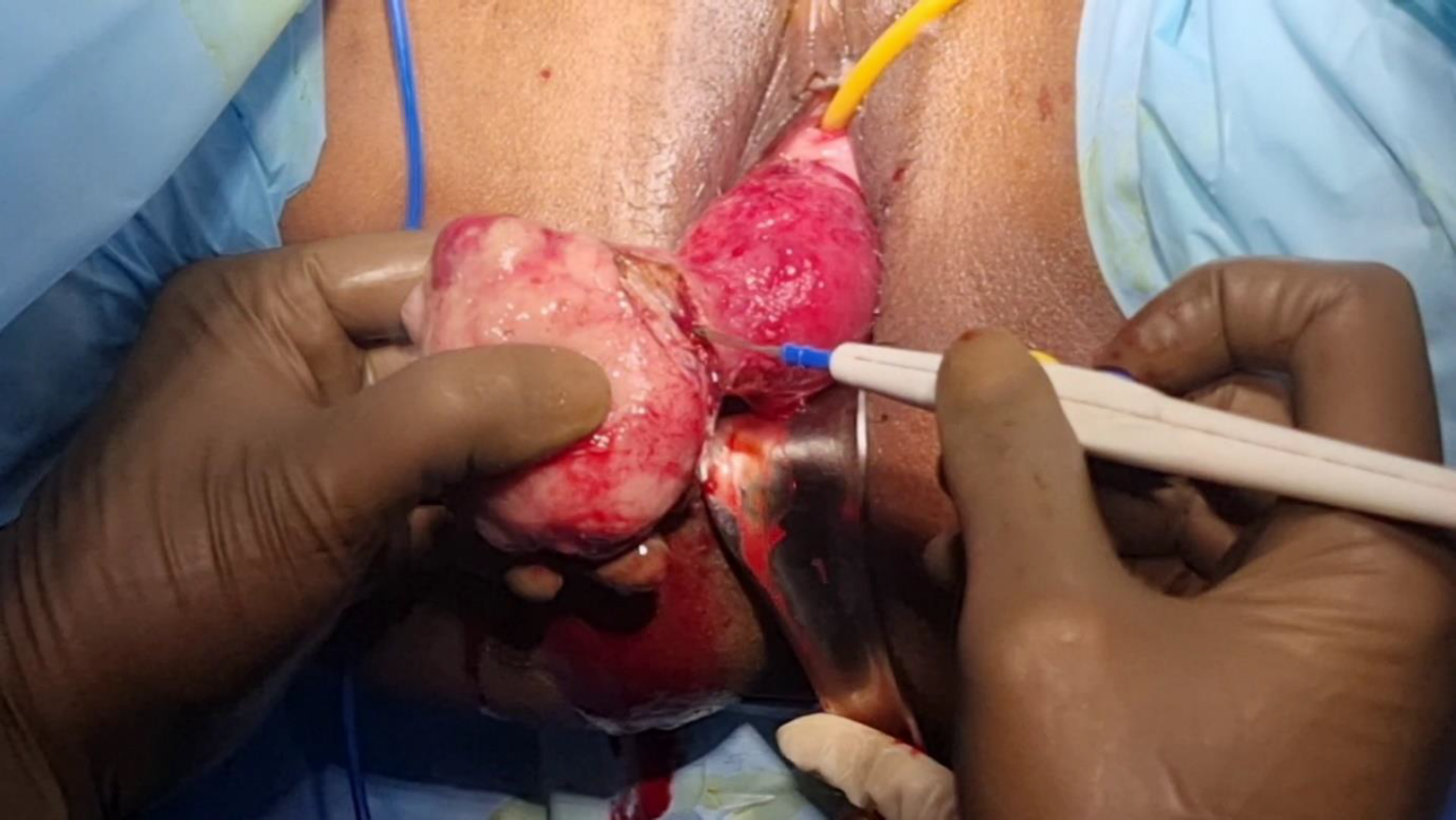
Figure 3. Vaginal myomectomy done to ease uterine reposition
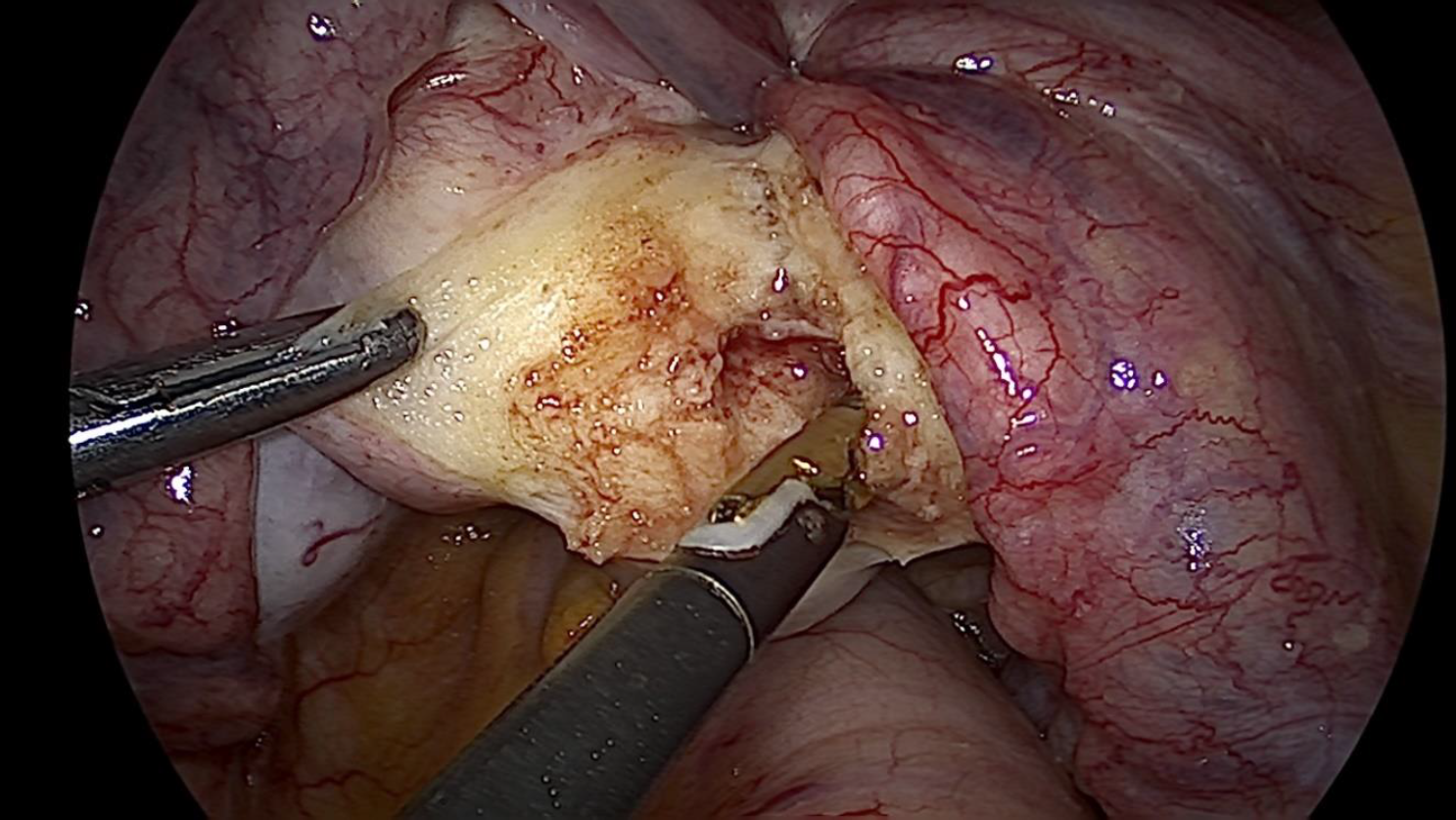
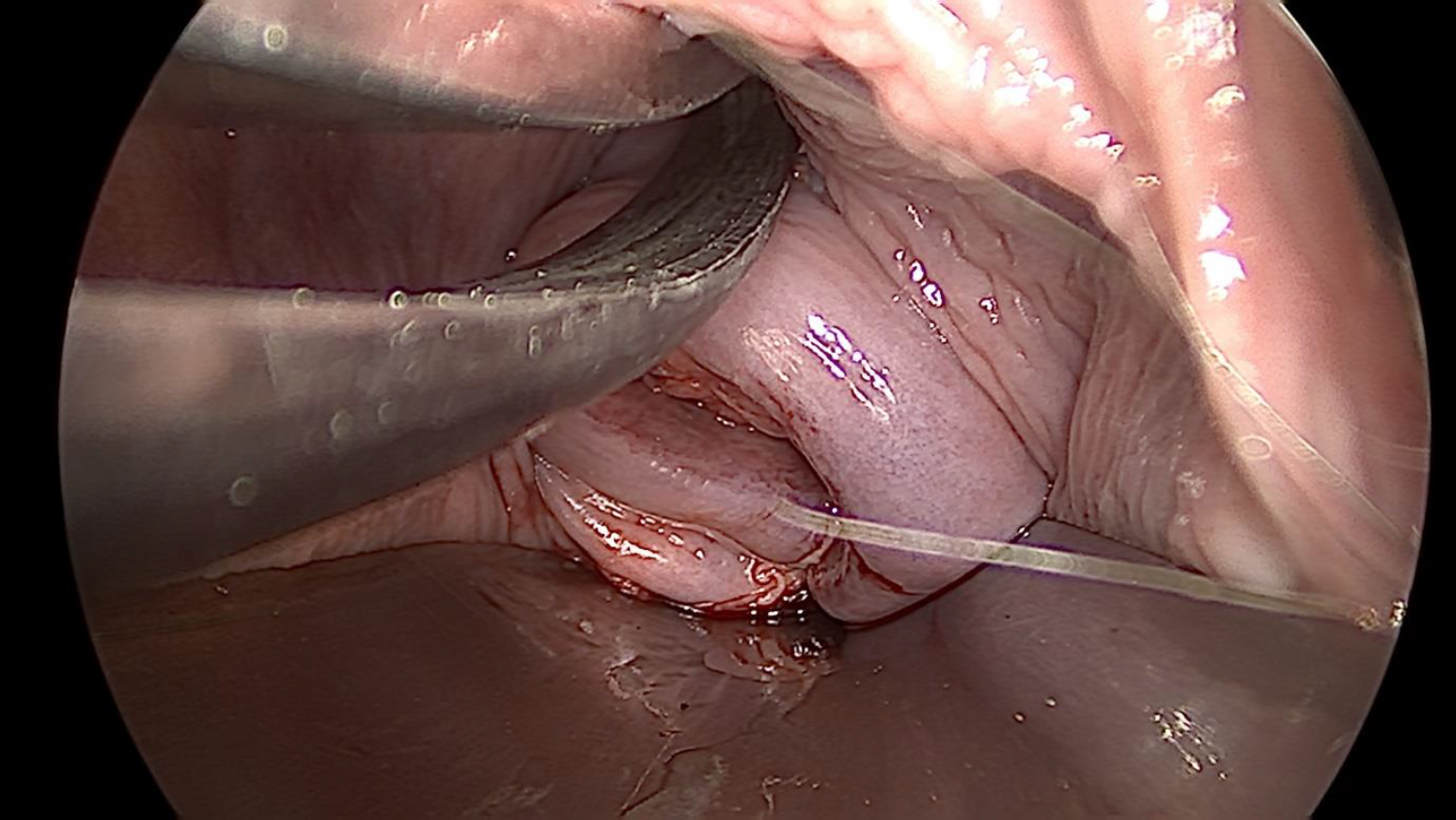
Figure 4. Uterine constriction Ring released with posterior incision on uterine isthmus and cervix
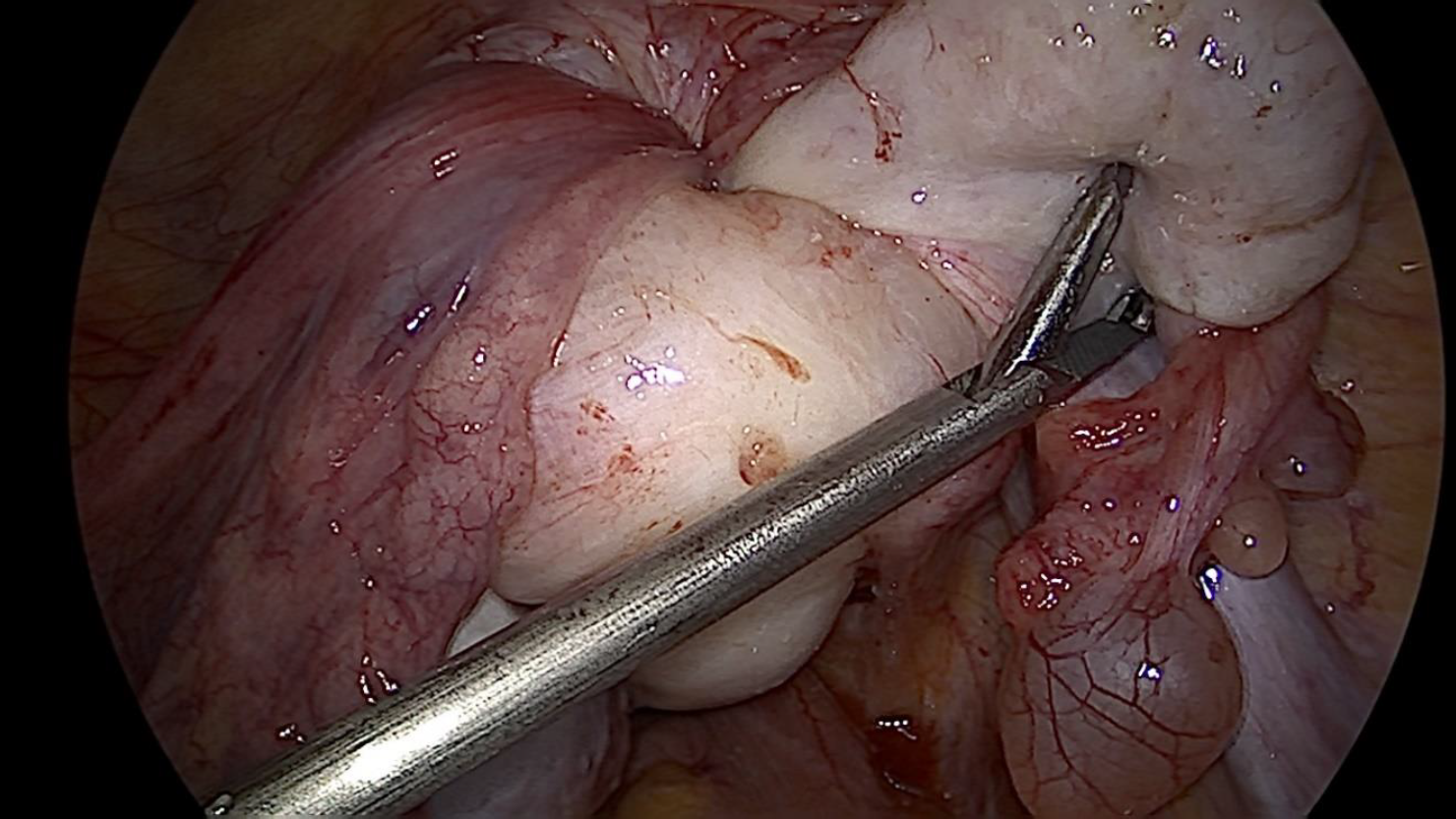
Figure 5. Upward traction on the medial ends of all cornual structures after release of constriction ring
Figure 6. Uterus reposited back
Figure 7. Uterine repair with barbed sutures
Figure 8. Final picture after uterine reposition and repair
Figure 9. Adhesion barrier placed over reposited uterus
Figure 10. Picture of cervix following uterine reposition