Authors / metadata
DOI: 10.36205/ trocar5.vid24001
Objective
To show how the use of indocyanine green would allow to identify and facilitate the resection of the isthmocele by laparoscopy.
Design
Stepwise demonstration of the technique with narrated video footage.
Setting
Every year around the world, between 20% and 35% of births occur via Caesarean section, and in most regions of the globe caesarean rates continue to grow [1-3].
Isthomecele was first described in 1961 by Poidevin, as an anatomical dehiscence in the uterine scar area, mainly identified through imaging techniques likes transvaginal ultrasound with or without fluid injection, hysterosalpingography, magnetic resonance imaging, and hysteroscopy [2, 4]. Reported prevalence varies from 24–70% with transvaginal sonography and 56–84% with sonohysterography [5]. Although most are asymptomatic, isthmocele should be suspected in women with spotting, dysmenorrhea, pelvic pain, and a history of infertility [6, 7]. Moreover, it could be associated with pregnancy complications, such as preterm delivery, uterine rupture, caesarean scar pregnancy, and abnormally adherent placenta [3]. Surgery is indicated in case of failure or contraindications to medical treatment. Currently, laparoscopic resection of the defect is the mainstay therapy method in patients with residual myometrium less than 3 mm and a desire to conceive [4, 8, 9]. Multiple strategies have been postulated to identify the isthmocele, such as the concomitant use of hysteroscopy, Foley catheter, or some dyes [3, 9, 10]. Indocyanine green is a dye used in medicine since the mid-1950s for various applications, due its extensive safety margin and near-infrared fluorescent optical advantage [11, 12]. Based on the ability of a dye to emit a fluorescent signal when excited with a light source at a specific wavelength and the highest tissue penetration depth, in this article, we propose the use of indocyanine green to identify the area to be resected in the laparoscopic treatment of Isthmocele.
Patient
A 41-year-old patient with a history of two previous cesarean deliveries presented a history of abnormal uterine bleeding and chronic pelvic pain that did not respond to medical treatment. The patient referred to desire for future fertility. Ultrasonography reveals residual myometrium of 2 mm, therefore, surgical treatment is decided. The patient underwent laparoscopic excision of Itshmocele using indocyanine green to locate and resect the defect.
Intervention
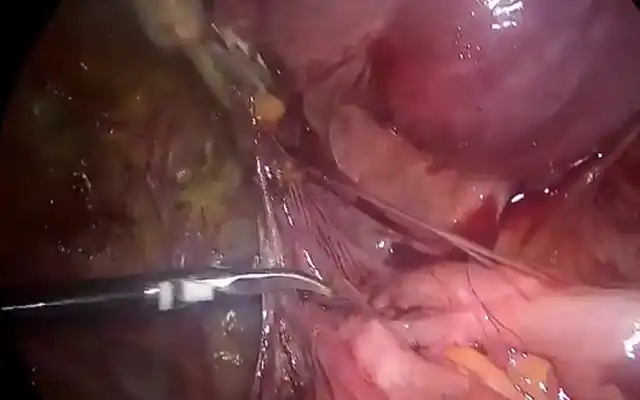
Laparoscopic repair of the Isthmocele was performed. Key strategies were: (1) Under laparoscopic vision, insertion of a uterine cannula into the uterine cavity reaching uterine Isthmus (3-4 cm from external cervical orifice). Through the uterine cannula 3 cc (7,5 mg) of indocyanine green dye without dilution was instilled and 3 minutes after, the uterine cannula was moved until achieving uterus fundus; (2) Careful dissection of the uterovesical peritoneal fold for mobilize bladder from the lower uterine segment; (3) Identification of the Isthmocele site with the use of near-infrared fluorescence imaging; (4) Resection of the defect is resected with monopolar scissors; (5) Placement of a uterine manipulator into the cervix to avoid the closure of the uterine canal to facilitate suturing; (6) Reapproaching of the edges with the use of a single layer of interrupted 2-0 Vycril sutures.
Conclusion
Laparoscopic surgical treatment of Isthmocele is a good alternative in patients with symptoms who do not respond to medical treatment, with wishes for fertility, and who present a residual myometrium of less than 3 mm. We propose using indocyanine green since it allows the evaluation and identification of the area to be resected without needing another procedure.