Authors / metadata
DOI: 10.36205/trocar5.2024003
Introduction
Tumors of the broad ligament are rare with most of them being secondary to other pelvic pathologies. Most neoplasms in this region present clinically with insidious and nonspecific symptoms and are discovered only incidentally during a gynecological examination for lower abdominal pain or discomfort (1). They are often difficult to distinguish from other adnexal lesions considering their location and rare occurrence. Confusing such lesions with ovarian or tubal masses is very common and hence a high index of suspicion is needed for their accurate preoperative diagnosis. Suspicion of such a lesion may allow for planning minimally invasive surgical interventions, with organ-preserving techniques in young patients.
Here, we present a rare case of True Broad Ligament Adenofibroma in a young asymptomatic woman.
Case presentation
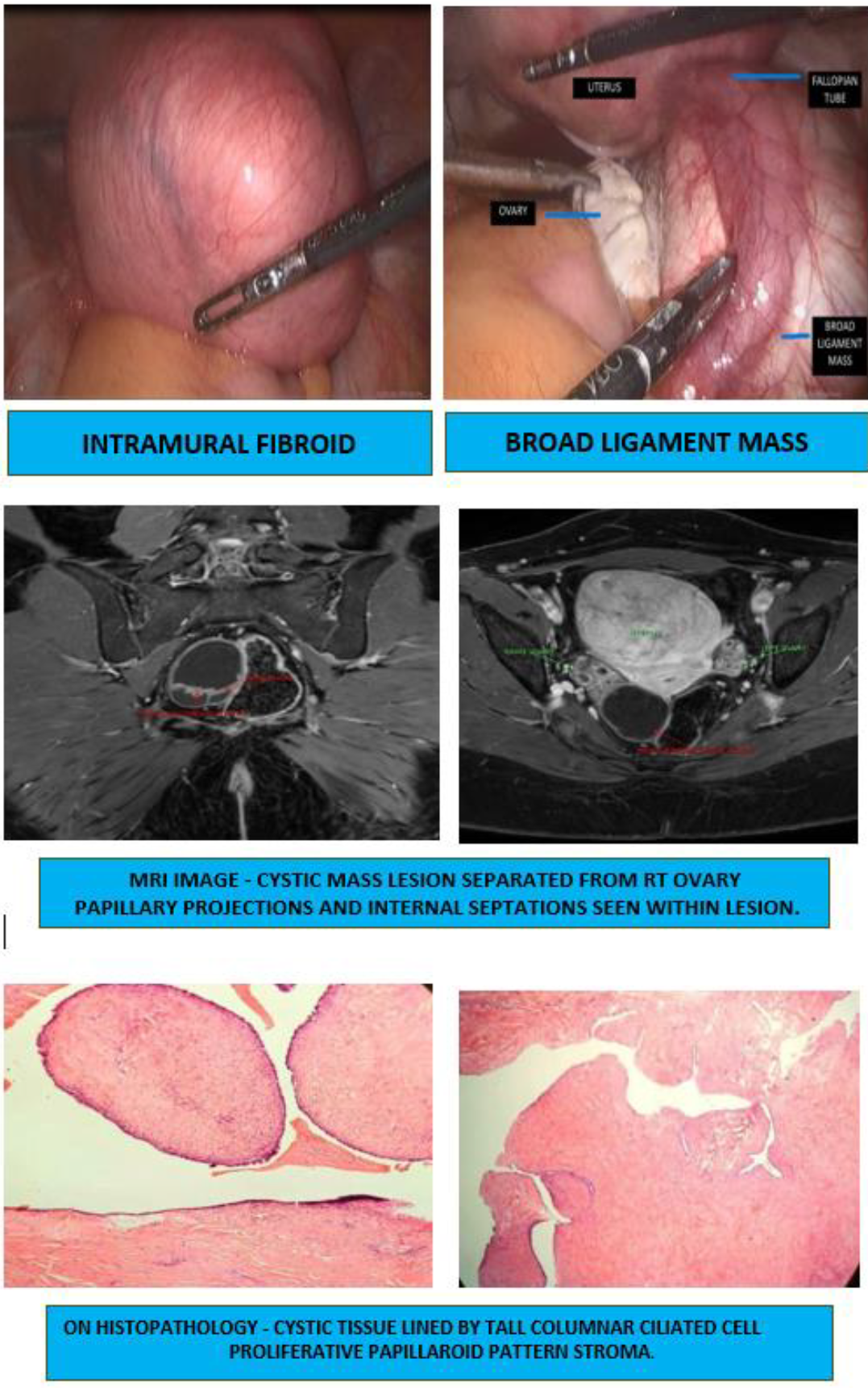
A 32-year-old female presented to the outpatient department for pre-conceptional counseling. She was married for 2 years and was planning to conceive. There were no menstrual complaints. Couple was co-habiting with no coital error. She had an average built with a body mass index of 29.4 kg/m2. General examination was unremarkable. On abdominal examination, a freely mobile lump with smooth margin was felt arising from the pelvis. Vaginal examination revealed a freely mobile, 14-16 weeks size retroverted uterus. On bi-manual examination, the lump was felt to arise from the uterus. Also, another non-tender mass, approximately 3 x 2 cm was felt in the right adnexa, separate from the uterus. Transvaginal ultrasonography revealed 7.85 x 7 x 8 cm large intramural fibroid (FIGO 2-5)at the uterine fundus. Another 5 x 2.8 cmright adnexal complex mass was also visualized, with uniform margins, multiple septations (septal thickness of 3.4 mm) and minimal vascularity. Right ovary could not be visualized separately from the mass. On Contrast Enhanced MRI pelvis, fibroid as discussed prior was noted. 3 x 3.8 x 5.2 cm well defined cystic mass with enhancing internal septations and tiny papillary projections was visualized in the right adnexa separate from ovary s/o- either Hydrosalpinx or para ovarian cyst (Fig 1). Tumor markers viz CA-125, Serum LDH, CA-19.9 and Alpha fetoprotein were sent, which came out to be normal. Hence, a laparoscopic procedure was planned. On laparoscopy, peritoneal fluid cytology was sent to rule out malignant cells which came out to be negative. 8 x 8 cm fibroid was noted, arising from the fundus anterior wall of the uterus and 5 x 4 cm complex cyst visualized in the right mesosalpinx separated from the fallopian tube and right ovary. Myomectomy and right meso-salpingeal cyst/broad ligament cyst excision was done without disturbing tubal anatomy. Care was taken to avoid any cyst rupture during excision. It was removed in toto, using the Endo bag without spillage in the pelvic cavity and specimen was sent for histopathological examination.
Histology report showed leiomyoma for the first specimen. Gross examination of the second specimen suggested congested and hemorrhagic external surface with polypoidal growth arising from the cyst wall. On microscopy: – Cystic tissue seen, lined by tall columnar ciliated cells. Stroma showed benign proliferation forming a papilloid pattern. No e/o atypia or malignancy. The findings were suggestive of adenofibroma of the mesosalpinx. The postoperative period was uneventful, and the patient was discharged the next day.
Discussion
Broad ligament is the fold of parietal peritoneum that is reflected over the female genital tract, extending from the uterus to the lateral pelvic wall. This double-layered sheet of mesothelial cell is continuous with each other, and between them is the extraperitoneal tissue (parametrium), containing the connective tissue, smooth muscles, and neurovascular elements. Embryonic remains are also normal component and may give rise to some of the unique neoplasms of the broad ligament, arising from the mesonephric (Wolffian) and paramesonephric (Müllerian) duct remnants (2). Other incidental tissues may also exist, such as heterotopic hilar cell clusters or adrenal cortical rests.
Tumors of the broad ligament can be classified on the basis of their place of origin or histology. Those arising exclusively from the broad ligament are called “Primary or True broad ligament tumors”, which are rare. Majority of tumors in the broad ligament are secondary to malignancies arising elsewhere in the pelvis, like endometrial, cervical, ovarian and other tumors not arising in the female reproductive tract (3). According to Gardner et al, a tumor primarily arising from the broad ligament, must occur on or in the broad ligament, but be completely separated from, and in no way connected, with either the uterus or the ovary (4).
Based on histology, tumors of the broad ligament can be of different types including, Epithelial tumors of Müllerian type, mesenchymal tumors, tumor-like lesions, and secondary tumors (Table 1). The most common among them are the leiomyomas. Among all the reported carcinomas, serous adenocarcinoma, clear cell adenocarcinoma and endometrioid adenocarcinoma are the most common histologic variants.
Meso-salpingeal / Broad Ligament Adenofibromas are rare tumors with low malignant potential. Although its origin is not clear, it is hypothesized to be an embryological remnant originated from the mullerian duct rather than a neoplastic proliferation process. The precise origin of broad ligament carcinomas is not known, but there are several hypotheses concerning their histogenesis like their origin from Serous Tubal Intraepithelial Carcinoma (STIC) lesions, similar to the ovarian high-grade serous carcinomas. As per another hypothesis, borderline and benign serous tumors transform into carcinoma, similar to that seen in ovarian carcinoma. These benign serous tumors originate from inclusion cysts derived from the coelomic epithelium, which covers the ovarian and broad ligament surfaces. The primary endometrioid and clear cell adenocarcinomas of the broad ligament have their origin in the Mullerian ducts and arise from background endometriosis (5). Most likely, the endometrioid carcinoma originate from an occult focus of endometriosis. The association of broad ligament carcinomas with endometriosis, as well as endosalpingiosis, was also reported in a few cases (6,7). The Mullerian-origin broad ligament tumors occur predominantly in reproductive women, but in the infertile and nulliparous, pointing out a possible hormonal role in the histogenesis of these tumors (8).
As the first-line study, transvaginal ultrasound can suggest broad ligament tumor when it allows clear visual separation of the tumor from the uterus and ovaries, but magnetic resonance imaging (MRI), with its multiplanar imaging capabilities, can be useful for differentiating broad ligament tumors from masses of ovarian or tubal origin. Other information provided by the MRI, such as tumor size and presence of any metastatic lesion or lymph nodes, are crucial findings for preoperative planning and counseling, making it the gold standard imaging modality. Due to the location and size of several of these tumors, surgery is challenging, specifically since the surrounding structures such as the ureters and iliac vessels may be at risk. Commonly, accurate diagnosis of broad ligament tumors is difficult pre-operatively, it is commonly established during surgery or at the histopathological evaluation (9).
Elangovana et al reported a case of a primary broad ligament adenocarcinoma in a 43-year-old female with a prolonged complaint of abdominal pain and intermittent urinary retention, requiring frequent catheterization (10). She was diagnosed with obstructive right hydroureteronephrosis secondary to an endometrioid adenocarcinoma of the broad ligament for which total abdominal hysterectomy, right salpingo-oophorectomy, pelvic lymph-nodal sampling was done followed by adjuvant chemo and hormonal therapy.
Khatib et al reported a case of Serous papillary cystadenofibroma (SPCAF) of the fallopian tube in a 30-year-old female who presented with pain and large abdominal mass (11). It was wrongly diagnosed as ovarian neoplasm on computed tomography. However, during surgery the tumor was found to arise from the fallopian tube and was treated with tubal cystectomy with ovarian sparing.
Tavares et al reported another atypical case of giant tubal serous adenofibroma of the fallopian tube in a 17-year-old girl who presented with a palpable mass occupying the entire abdomen accompanied by urinary symptoms (12). She underwent a laparoscopic surgery with drainage of 1800 mL of yellow, citrine liquid from the cyst followed by left salpingectomy.
Most neoplasms in this region, whether benign or malignant, usually present with vague symptoms and are often discovered during a routine gynecological examination. Distinction of mesosalpingeal tumors from other solid tumors of ovary, uterus or retro peritoneum is challenging anatomically & radiologically. As a result, these lesions are frequently found incidentally during surgery. These tumors are usually benign hence extensive surgery is not required and simple excision suffices.
Conclusion
Masses arising from the broad ligament are rare. Because of their location, they represent a clinical and radiological problem. An accurate diagnosis can remain difficult despite good clinical and radiological prediction, and diagnosis is often made intraoperatively. Adenofibromas are rare tumors that can appear malignant macroscopically or on ultrasound. Due to their low malignant potential, an accurate index of suspicion may help avoid radical surgery, especially in young patients desiring fertility.