Information
- Authors: O. Sizzi, A. Rossetti, M. Saldari (matteo.saldari@gmail.com), L. Manganaro (lucia.manganaro@uniroma1.it), M. Mercuri (mercurimassimo@yahoo.it)
VIDEO SURPRISES: THE GHOST CYST STORY:
Laparoscopic Ablation of a Pelvic Retroperitoneal Epidermoid Cyst.
O. Sizzi, A. Rossetti, M. Saldari, L. Manganaro, M. MercuriIntroduction: Experience with minimally invasive approaches, such as laparoscopic ablation and transanal endoscopic microsurgery ,to resection pelvic retroperitoneal and presacral tumors is limited. Masses arising from this anatomic position are usually removed using a transsacral approach or laparotomy. We report a detailed description of the laparoscopic procedure performed in a 32-year-old woman to remove a mass, which was detected with both ultrasonography and magnetic resonance imaging, that was closely adherent to the left sacrospinous ligament and compress in the rectum. Histopathologic findings were consistent with a rare case of pelvic retroperitoneal epidermoid cyst. This tumor, which usually occurs in the face, the scalp, the trunk, or the neck, has been described in the pelvic retroperitoneal space in only a few cases.
Case Description: A 32-year-old nulligravid woman was referred to our hospital because of an 11-month-long deep dyspareunia and left lower quadrant abdominal pain with radiation to the coccyx and anus. One month earlier, at another institution, she had undergone diagnostic laparoscopic exploration because of suspected left ovarian endometriotic cyst detected on transvaginal ultrasonographic scan. Laparoscopy had not shown any ovarian endometrioma, and the patient had been discharged the day after the intervention. Three weeks later, because of persistence of the symptoms, she underwent another transvaginal ultrasonographic scan, which confirmed the presence of an endometriotic cyst. Our gynecologic and rectal examinations revealed normal external genitalia; a normal-sized anteverted uterus; no abdominal masses, or hernias; and ultrasonographic finding of a well-circumscribed hypoechoic cystic pelvic mass, resembling an endometrioma of 8 cm in diameter on the left side at the level of the rectovaginal septum. The cyst was adjacent to but apparently cleavable from the rectal mucosa without signs of infiltration, although it was not movable with the vaginal probe. Laboratory tests revealed no abnormalities, and serum tumor markers (CA 125, CA 19–9, CEA, and αfetoprotein) were negative. A pelvic MRI examination was highly suggestive of a retroperitoneal epidermoid cyst. Surgical exploration was recommended.
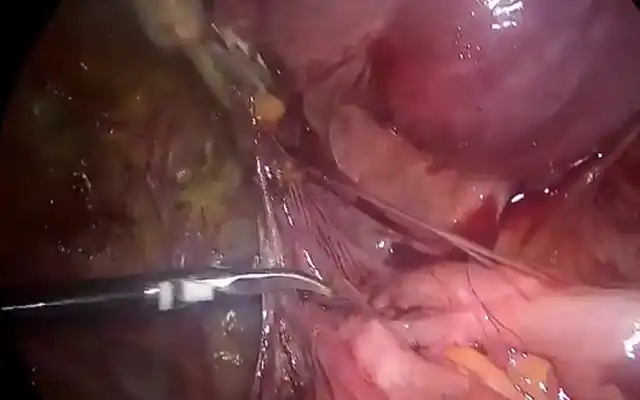
Operative Technique: a laparoscopy was planned with the presence of a general surgeon in case a rectal resection was necessary during the intervention. Laparoscopic examination of the peritoneal cavity showed no lesions, and the uterus and both ovaries were normal. Taking into account the MRI findings, we performed a more thorough laparoscopic inspection of the vagina and rectum. We found a softness and increased thickness at the level of the left pubococcygeal and puborectalis muscles and a slight protrusion at the level of the left uterosacral ligament next to the rectum. At this point, the left ureter was mobilized starting from the pelvic brim, and the peritoneum was incised between the left uterosacral ligament and the rectum. Through a sharp and blunt dissection, the underneath connective and fat tissue was removed and the visualization of the cyst was possible. The mass appeared to be tenaciously adherent to the pelvic floor muscles inferiorly and to the rectum medially. We proceeded with an accurate dissection of the lesion and with its progressive isolation. At the end of the dissection, the cyst was accidentally opened and an amorphous material spilled out. The thick fluid contents of the cyst were removed by suction, and after several washings, the wall of the cyst was inspected. The internal lining was void of vegetation or atypical blood vessels. After the cyst was emptied, the final enucleation turned out to be almost effortless.
Conclusions: In conclusion, surgical excision represents the cornerstone in the diagnosis and treatment of pelvic retroperitoneal epidermoid cysts. MRI is useful to define the extent of the lesion and to guide operative therapy. Due to magnification of the anatomic elements in the narrow pelvis, laparoscopy may lead to a successful minimally invasive surgical ablation without using an additional perineal approach or laparotomy. It allows minimal resection of adjacent organs without damage and helps to avoid complications that could, on the contrary, occur in case of an additional perineal approach.
References:
- Yang DM, Yoon MH, Kim HS, et al. Presacral epidermoid cyst: imaging findings with histopathologic correlation. Abdom Imaging. 2001;26(1):79–82.
- Al-Khattabi M, Chouillard E, Louboutin A, Fauconnier A, Badger G. Giant pararectal epidermoid tumor mimicking ovarian cyst: combined laparoscopic and perineal surgical approach. J Minim Invasive Gynecol. 2010;17(1):113–115.
- Palanivelu C, Rangarajan M, Senthilkumar R, Madankumar MV, Annapoorni S. Laparoscopic and perineal excision of an infected “dumb-bell” shaped retrorectal epidermoid cyst. J Laparoendosc Adv Surg Tech A. 2008;18(1):88 –92.
- Loock MT, Forne`s P, Soyer P, Rousset P, Azizi L, Hoeffel C. MR imaging features of nongynaecologic cystic lesions of the pelvis. Clin Imaging. 2013;37(2):211–218.
- Shanbhogue AK, Fasih N, Macdonald DB, Sheikh AM, Menias CO, Prasad SR. Uncommon primary pelvic retroperitoneal masses in adults: a pattern-based imaging approach. Radiographics. 2012;32(3):795– 817.
- Yang DM, Jung DH, Kin H, et al. Retroperitoneal cystic masses: CT, clinical, and pathologic findings and literature review. Radiographics. 2004;24(5):1353–1365
- Sciaudone G, Di Stazio C, Guadagni I, Pellino G, De Rosa M, Selvaggi F. Retrorectal epidermoid cyst–a rare entity: the effectiveness of a transperineal posterior approach. Acta Chir Belg. 2009;109(3):392–395.
- Li GD, Chen K, Fu D, et al. Surgical strategy for presacral tumors: analysis of 33 cases. Chin Med J (Engl). 2011;124(23): 4086–4091.
- Sherer DM, Zinn H, Gavrilescu T, et al. Transvaginal sonographic diagnosis of a large retroperitoneal pelvic epidermoid cyst (monodermal teratoma). J Ultrasound Med. 2006;25(2):265– 268.
- Chen Y, Xu H, Li Y, et al. Laparoscopic resection of presacral teratomas. J Minim Invasive Gynecol. 2008;15(5):649–651.
- Zoller S, Joos A, Dinter D, et al. Retrorectal tumors: excision by transanal endoscopic microsurgery. Rev Esp Enferm Dig. 2007;99(9):547–550.
- Vaid S, Nicholson T. A novel approach to closure of perineal wounds during abdominoperineal resection: use of fibrin sealant. Arch Surg. 2012;147(8):778 –780. JSLS
Video
MEMBERS AREA
Categories