Authors / metadata
DOI : 10.36205/trocar2.2023001
Abstract
Myomectomy is a surgery at risks for per operative hemorrhage. Intra rectal misoprostol administered the day before the operation and the use of a peri cervical tourniquet per operative are both methods used to reduce peri operative blood loss. In order to be able to compare the two methods, a randomized, controlled study was carried out at our institute. 48 patients were enrolled in the study and followed up and the data analyzed. Both methods proved to be equally effective and both can be used routinely.
Introduction
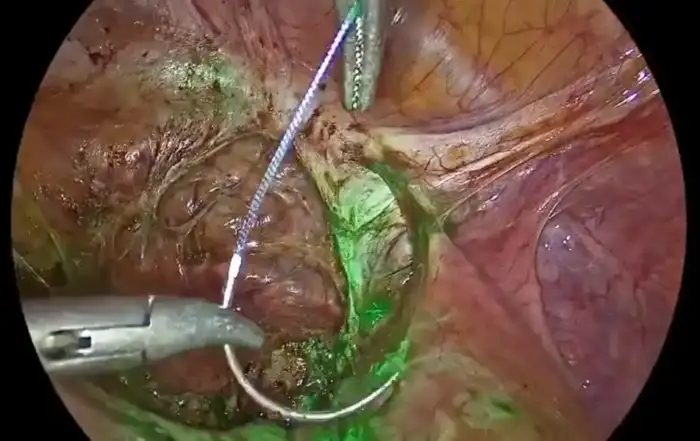
Uterine myoma are considered to be the most frequent benign tumours in female patients both in reproductive age and menopause. 80% of African women are diagnosed with myoma before the age of 50 years (1,2). The treatment of choice in women with a desire to procreate is the operative myomectomy by laparoscopy or laparotomy. The myoma surgery is associated with blood loss due to the enucleation of the myoma. The blood loss gives rise to blood transfusion and a possible conversion to hysterectomy when the bleeding becomes uncontrollable (3,4). The use of a peri cervical tourniquet is the widest spread method to prevent incontrollable blood loss in the countries with limited resources in view of its efficacy, simplicity and low costs (5). On the other hand, studies have proven that the use of misoprostol, due to its contractile effect on the myometrium, is also a good method to prevent excessive blood loss during myomectomy (6,7). This treatment could become an alternative to the peri cervical tourniquet in the low-income countries as it is a simple method also with low costs but at this moment in time the method is scarcely used in these countries. This study has been set up to compare the efficacy of a single, peroperative doses of 400 g of intra-rectal administered misoprostol and the haemostatic peri cervical tourniquet used during the laparotomic surgery for myomectomy.
Material method
At the CHRACERH a Randomised Controlled Trial (RCT) single blinded has been set up over a period of nine months from February 2022 onwards. All patients needing a laparotomic myomectomy have been included in the trial after giving consent. All patients presenting with symptomatic myomata, documented by pelvic medical imaging over the last 12 months, all patients aged over 18 years of age and all patients who did sign a consent form who were in need of a laparotomic myomectomy have been included in the study. Patients with coagulation disorders have not been included in the study. Further have been excluded from the study all cases where other surgical acts and every other method to reduce blood loss had been used. Also excluded have been the patients where the administration of misoprostol was contraindicated and in the group of the peri cervical tourniquet all cases presenting with difficulties to apply the tourniquet. The sample has been built on a consecutive, random and comprehensive basis. Patients have been assigned to each group (group I =misoprostol, group II=tourniquet) on the principle of assignation by lot after selection of the patient for one or the other techniques. The study did use the formula of Charan&Biswas to find out the number needed to diagnose:
n = [(Z1-α/2 + Z1-β) 2 x {2(ó) 2}]/ (μ1 – μ2)2 [8]
Based on this formula and on the data of a prior study where the mean of the blood loss had been 230,66 ml in the misoprostol group and 322,39 in the control group, the number needed to diagnose has been defined on 19 patients per group (9). This implies that the total sample has to be 38 patients.
Practically the patient of the misoprostol group – group I – did receive a single dose of 400 μg of intra rectal misoprostol two hours before surgery. The patients of group II were treated with the placement of a Foley urinary catheter n° 18 as peri cervical tourniquet, placed through the round ligaments, during the surgery. The tourniquet was released within the hour after its application. The factors registered were: the characteristics of the myoma, the peroperative blood loss, the necessity for blood transfusion and postoperative AUB and eventual conversion to hysterectomy. As far as the measurement of the per operative blood loss is concerned these have been measured in both groups with the same technique: blood has been aspirated with an aspiration cannula into a bag and further by weighing the pads, uniforms worn and operation field drapes. Estimation have been made on the equation that one gram to be equivalent to one milliliter blood.
To interpret the results the following programs have been used C’s Pro and SPSS 26.0. Qualitative variables have been represented by the real events and the frequencies of the latter. The quantitative variables have been described by the mean +/- put aside principle. The association between quantitative and qualitative variables has been evidenced by the Chi-square test when the theoretical events have been equal or higher than five, or the Fisher Exact test when at least one event scored less then 5. The means have then be subjected to the Student T test. The P<0.05 has been considered zs statistically significative.
Results
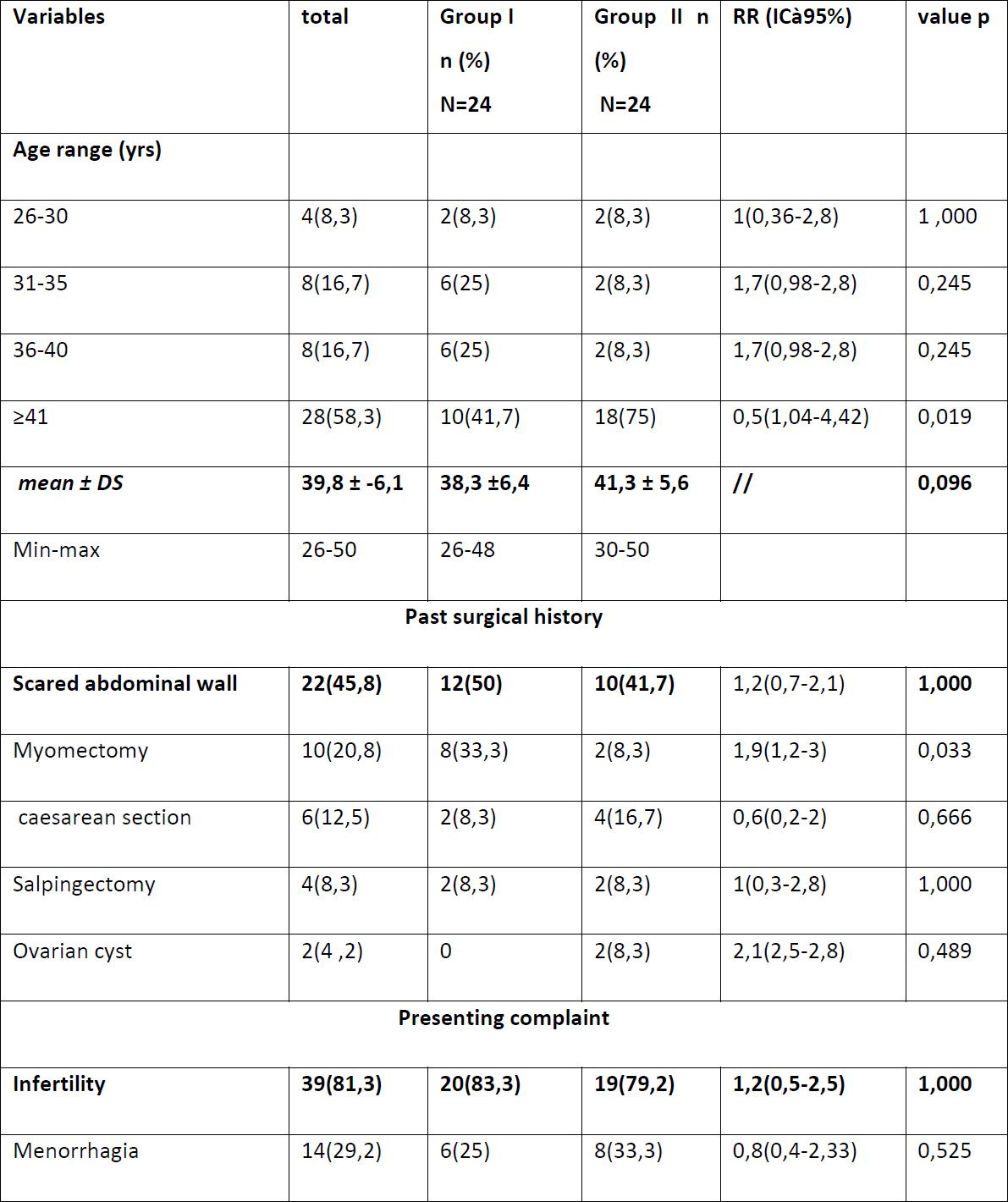
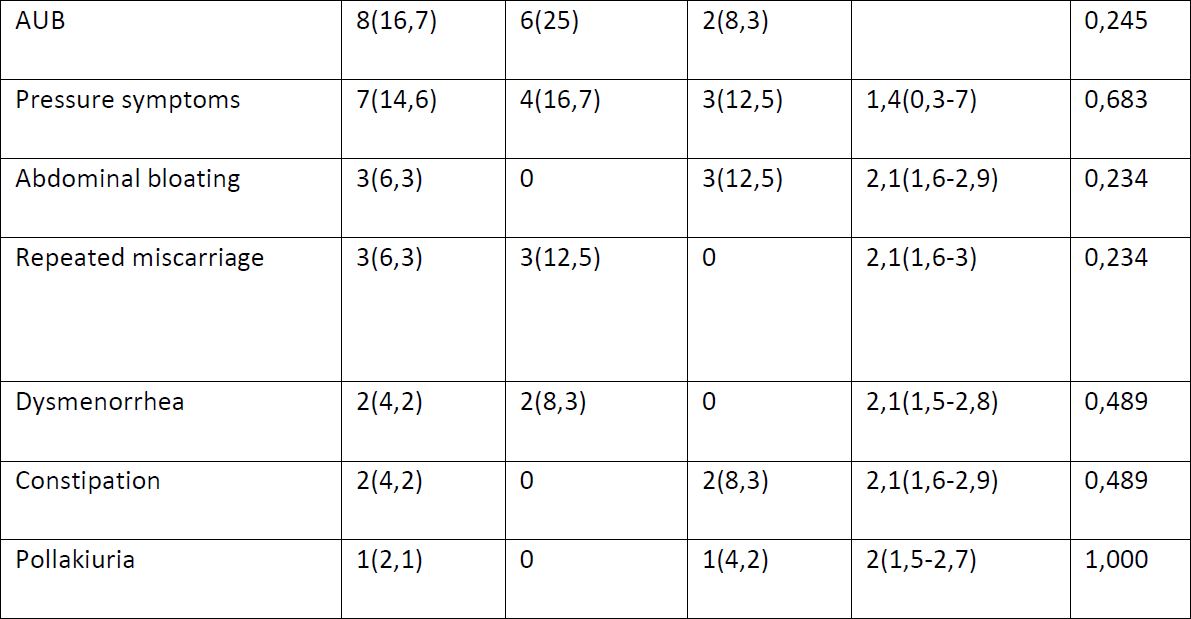
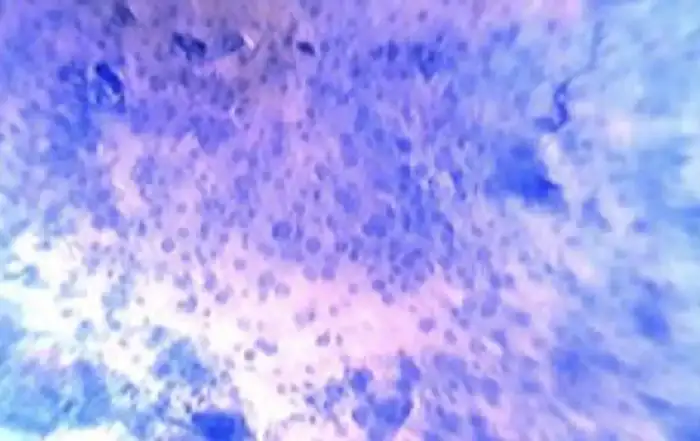
A total of 51 patients have been assigned to the study. Three patients have been excluded because of pelvic adhesions not allowing for the placement of the peri cervical tourniquet. Finally, 48 women did participate to the study, 24 in each group. The median of age has been comparable in both groups, 38,3+/-6,4 years in the misoprostol group versus 41,3+/-5,6 in the tourniquet group (P=0,096) (Tab 1) The frequency of patients with a scared uterine surface was comparable in both groups 50 % in the misoprostol group versus 41,7% in the tourniquet group (P=1,000) (Tab 1). Infertility has been the main complaint to seek advice in both groups with 83,3% in the misoprostol group and 79,2% in the tourniquet group (Tab 1).
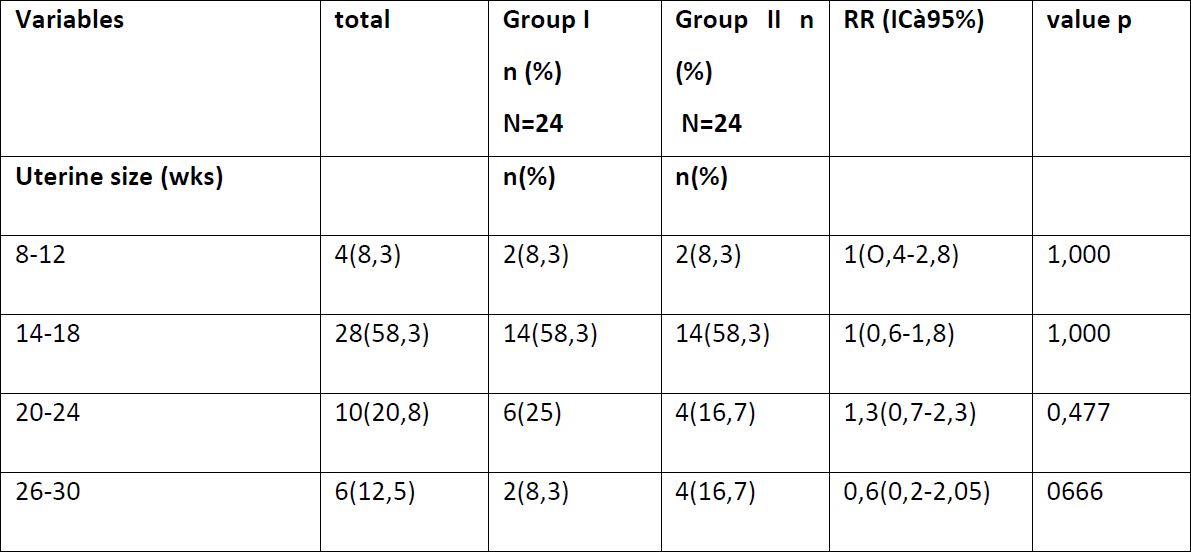
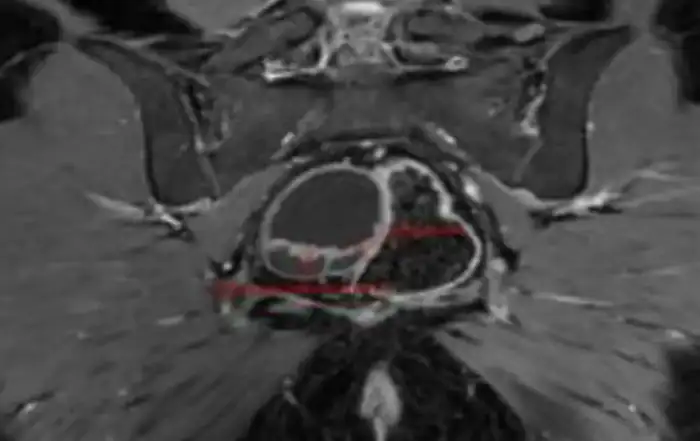
The mean size of the uteri was equal in both groups 18,25+/-4,7 pregnancy weeks in the misoprostol group versus 18,7+/-5,5 pregnancy week in the tourniquet group (Tab2). The most prominent feature has been intra mural myoma present in 100% in the misoprostol group and in 95,8% in the tourniquet group (Tab2). The total number of myomata has been 9,7+/-5,9 in the misoprostol group versus 10,2+/-6,8 in group II (Tab2).
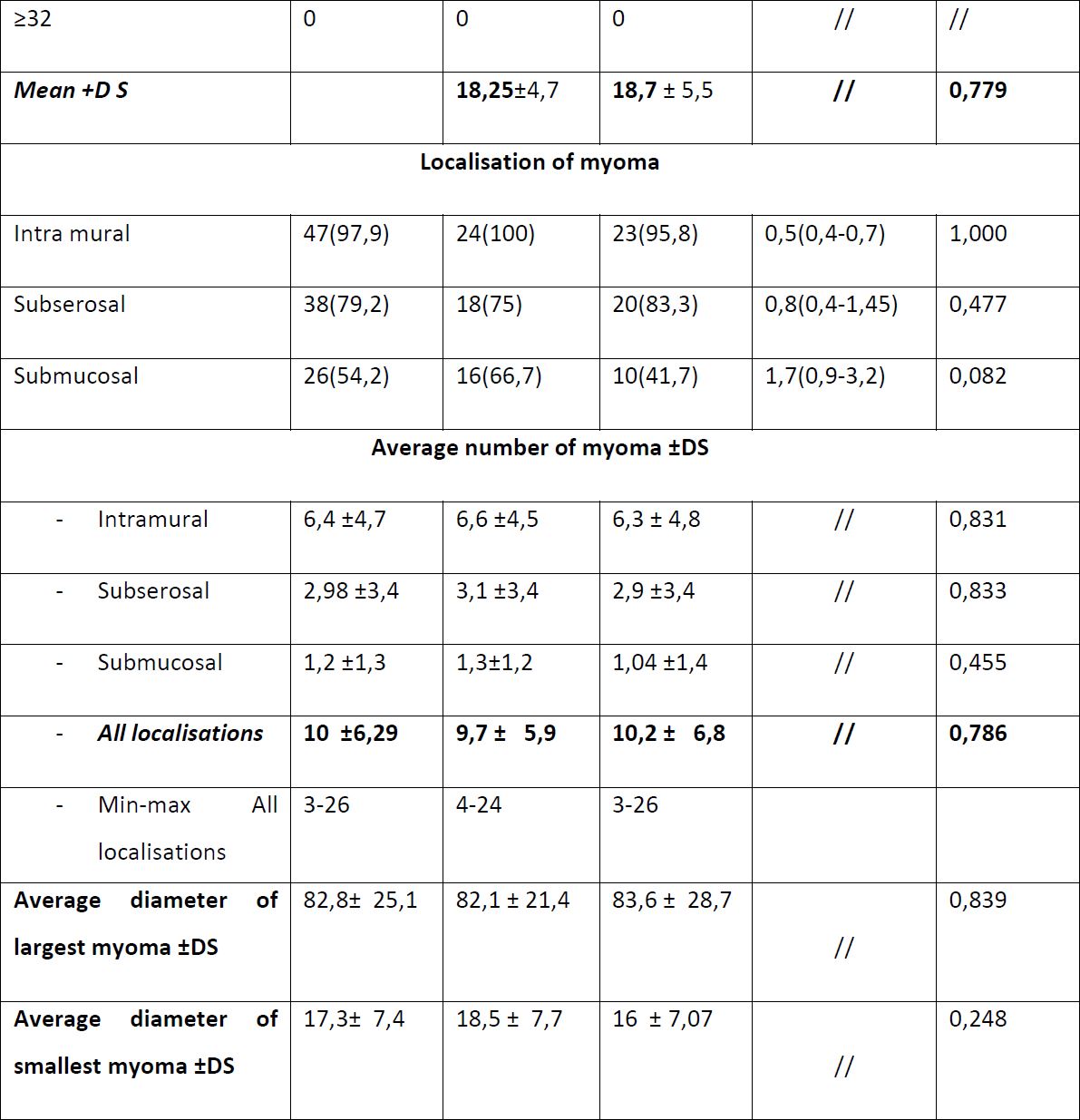
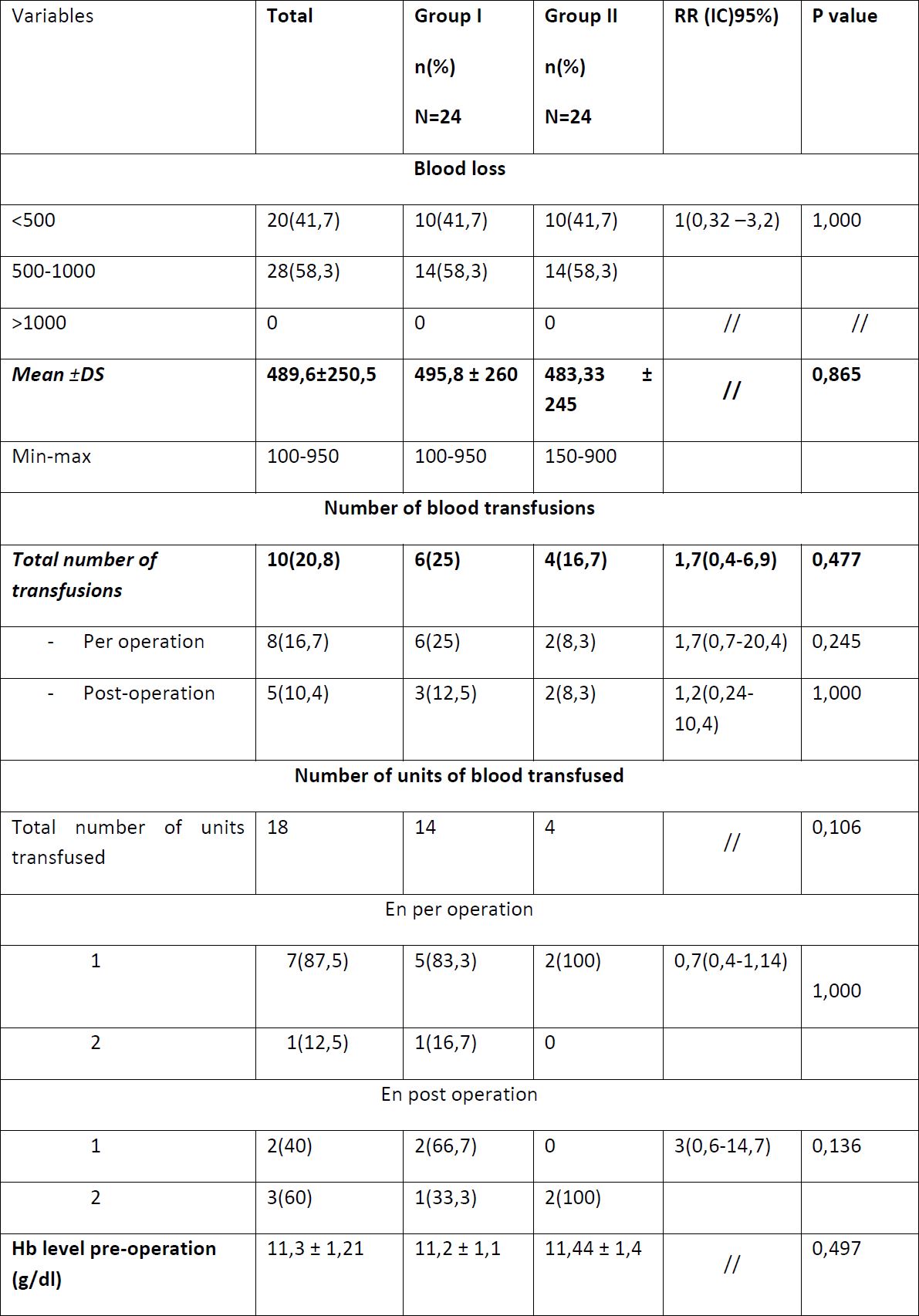
Blood loss has been comparable between both groups 495,8+/-260 ml in group I versus 483,33+/-245 in group 2 (Tab 3). Blood transfusions have been administered equally between both groups 25% in group I and 16,7% in group II (Tab3).
There has been no conversion to hysterectomy in the study. Complications: a haemorrhage, that could be managed, has been noted after the tourniquet had been released in two cases.
Discussion
Uterine myomata are the most frequent benign rumours in women of reproductive age. Age seems to be the most important factor and the prevalence of myomata increases with age up to the menopause. In this study the mean age of the patients was 38,3+/-6,4 years in the misoprostol group and 41,3+/-5,6 in the tourniquet group. These results are comparable with the data from Sharami 2020 (39,34+/-6,38 in the misoprostol group and 38,00+/-4,89 in the control group) or the results of Abdel 2015 (40,7+/-5,1 in the misoprostol group and 40,7+/-5,5 in the control group (10-11).
Although most of the uterine myomata are asymptomatic some 20-40% are symptomatic with symptoms including AUB, anaemia, dyspareunia, pollakisuria, abdominal discomfort and heaviness, constipation and reproductive dysfunction (miscarriages, infertility) that impair the quality of life of the patients and hence have to be treated. In the CHRACERH study the patients did present with the following complaints in decreasing order: first infertility (83,3% in group I versus 79,2% in group II), followed by menorrhagia (25% in group I versus 33,3% in group II) and AUB (25% in group I and 8,3% in group II) finally other complaints including feeling of weight in the pelvic area, abdominal bloating, repeated miscarriages, dysmenorrhea, constipation and pollakisuria. These results differ from the findings of Ali 2019 and Elourdighi 2012 both authors state that the principal complaint to be haemorrhage (14-15). The difference could be explained by the fact the CHRACERH is a center focused on the treatment of infertility.
The treatment of myomata in women with the desire to preserve their fertility is an myomectomy. Myomectomies are often complicated by per operative haemorrhages. There are multiple strategies to counter these haemorrhages, mechanical, surgical and pharmaceutical. Placing a Foley catheter as a mechanical peri cervical tourniquet is frequently used to reduce per operative haemorrhages. One arm of this study did look at its use. The misoprostol does act by causing contraction of the myometrial muscle fibres. The second arm of this study did look into this effect. Misoprostol can be administered by rectal or vaginal way or by mouth even sublingual some hours before the actual myomectomy. When misoprostol is administered by rectal way its peak plasmatic level is detected after two hours after administration and maintained for four hours. The side effects of misoprostol are minimal and reversible when compared to the other routes of administration. In the CHRACERH study the intra rectal misoprostol was administered two hours before the myomectomy.
The haemorrhages during myomectomy are conditioned by the characteristics of the myomata, especially the volume of the uterus, the number of myomata and their location. More important haemorrhages are to be expected if the myomata are large, if their number is important and if the location in intramural, within the myometrial wall. In the CHRACERH the measurements of the myomata where comparable in both groups 18,25+/-4,7 pregnancy weeks in group I and 18,7+/-5,5 pregnancy weeks in group II. These results are different from Celik 2003 (15,7+/-2,6 pregnancy weeks in his misoprostol group and 15,5+/-2,8 pregnancy weeks in his tourniquet group) (16). This fact can be explained as myomata tend to be larger in size in women of the black race. In our study, the total number of myomata has been 9,7+/-5,9 in the misoprostol group versus 10,2+/-6,8 in group II. Celik reported comparable number of myomata in both his groups 9,7+/-5,9 in the misoprostol group versus 10,2+/-6,8 in the tourniquet group. Finally, the intra mural myomata revealed to be 100% in the misoprostol group versus 95,8% in the tourniquet group. The findings concerning the per operative haemorrhages are different form the findings of Afolabi 2019 (931,89+/-602,13 ml in the misoprostol group versus 848,40+/-588,85ml in the tourniquet group P=0,532) (17). Here the volume of the uteri and the number of the myomata found in the CHRACERH were smaller that he one found in the study of Afolabi what can explain the differences.
However, the results are much worse in the studies where no measures had been taken to reduce the volume of the per operative haemorrhages. This is the case in the studies of Celik 2003 (621+/-121 ml in the placebo group) and of Niroomand 2015 (696+/-411 ml in the placebo group) (16-18). In the CHRACERH study the number of blood transfusions in both groups are comparable (25% group I and 16,7% group II). These results compare favourably with the study of Afolabi 2019 (60% in the misoprostol group and 55% in the tourniquet group) (17). The variation of the haemoglobin in the CHRACERH study have been comparable in both groups (1,22+/-0,6 g/dL in group I versus 1,5+/-1 g/dL in group II). In the Abdel 2015 study the results are 1,7+/-0,4g/dL in his misoprostol group and 2,1+/-0,5g/dL in his control group (11). These results can be explained by the fact that the peroperative blood loss was lesser in the CHRACERH study.
The only side effect of the misoprostol in our study has been one case of raised temperature. This finding is different from the Celik study (raised temperature in 38,4% of patients). This difference can be explained by the route of administration rectal in the CHRACERH study and vaginal in the Celik study.
Conclusion
In the CHRACERH study the haemorrhages are comparable in both the groups. The use of blood transfusion is the same in both groups. No conversion to hysterectomy was necessary. The side effects of misoprostol by intra rectal administration are minimal.
Acknowledgement: The authors wish to thank Bruno J van Herendael for his critical remarks and helping out in translating the article.